Abstract
Purpose
A nationwide survey was conducted to investigate the current status of pediatric gastroesophageal reflux disease (GERD) in Japan, with special reference to the characteristics of intractable GERD.
Methods
Data were collected using a questionnaire from facilities specializing in the treatment of pediatric GERD in Japan. Intractable GERD was defined as follows: I, no symptomatic improvement after 8 weeks of optimal medical treatment (OMT) plus fundoplication; II, no symptomatic improvement after 8 weeks of OMT and with no indications for fundoplication; and III, no symptomatic improvement after surgery without OMT.
Results
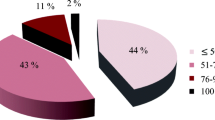
We collected data from 3,463 pediatric patients with GERD from 91 institutions, and 81 satisfied the definition of intractable GERD. Additional clinical information was obtained from 56 patients, and 41 represented cases of definite intractable GERD. The main underlying disorders included neurological impairment (NI), esophageal atresia (EA), and congenital heart disease (CHD), which altogether accounted for 85% of patients. Of the 41 patients, 33 received fundoplication, and the remaining 8 received medical treatment alone because surgery was considered unsuitable.
Conclusions
The nationwide survey revealed that pediatric intractable GERD is rare in Japan. Three main underlying disorders—NI, EA, and CHD—were implicated in the majority of cases of intractable GERD.

Similar content being viewed by others
References
Nelson SP, Chen EH, Syniar GM, Christoffel KK. Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med. 1997;151:569–72.
Hassall E, Kerr W, El-Serag HB. Characteristics of children receiving proton pump inhibitors continuously for up to 11 years duration. J Pediatr. 2007;150(262–7):7.e1.
Rosen R, Vandenplas Y, Singendonk M, Cabana M, DiLorenzo C, Gottrand F, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the north american society for pediatric gastroenterology, hepatology, and nutrition and the european society for pediatric gastroenterology, hepatology, and nutrition. J Pediatr Gastroenterol Nutr. 2018;66:516–54.
Iwakiri K, Kinoshita Y, Habu Y, Oshima T, Manabe N, Fujiwara Y, et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol. 2016;51:751–67.
Homepage of Statistics Bureau, Ministry of Internal Affairs and Communications. 1996. https://www.stat.go.jp/data/jinsui/topics/topi1091.html. Accessed 30 Apr 2020
Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–7.
Kinoshita Y, Adachi K, Hongo M, Haruma K. Systematic review of the epidemiology of gastroesophageal reflux disease in Japan. J Gastroenterol. 2011;46:1092–103.
Ruigómez A, Wallander MA, Lundborg P, Johansson S, Rodriguez LA. Gastroesophageal reflux disease in children and adolescents in primary care. Scand J Gastroenterol. 2010;45:139–46.
Short HL, Travers C, McCracken C, Wulkan ML, Clifton MS, Raval MV. Increased morbidity and mortality in cardiac patients undergoing fundoplication. Pediatr Surg Int. 2017;33:559–67.
Carpenter JL, Soeken TA, Correa AJ, Zamora IJ, Fallon SC, Kissler MJ, et al. Feeding gastrostomy in children with complex heart disease: when is a fundoplication indicated? Pediatr Surg Int. 2016;32:285–9.
Krishnan U, Mousa H, Dall’Oglio L, Homaira N, Rosen R, Faure C, et al. Espghan-Naspghan guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with esophageal atresia-tracheoesophageal fistula. J Pediatr Gastroenterol Nutr. 2016;63:550–70.
Foker JE, Kendall Krosch TC, Catton K, Munro F, Khan KM. Long-gap esophageal atresia treated by growth induction: the biological potential and early follow-up results. Semin Pediatr Surg. 2009;18:23–9.
Zangen T, Ciarla C, Zangen S, Di Lorenzo C, Flores AF, Cocjin J, et al. Gastrointestinal motility and sensory abnormalities may contribute to food refusal in medically fragile toddlers. J Pediatr Gastroenterol Nutr. 2003;37:287–93.
Acknowledgements
This study was supported by a grant 2017–2019 from the Ministry of Health, Labour Sciences Research Grants for Research on intractable disease (H29-Nanchi-Ippan-015) to Professor Tomoaki Taguchi. The authors thank the 97 certified institutions and the 67 associated facilities of the Japanese Society of Pediatric Surgeons and the 48 affiliated facilities of the representatives of the Japanese Society for Pediatric Gastroenterology, Hepatology and Nutrition that participated in this survey.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by SF, MY, and HK. Data collection and analysis were performed by SF, DM, and NH. The first draft of the manuscript was written by SF; all authors reviewed the manuscript for intellectual content. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The anonymity of all patients was guaranteed. This study was approved by the ethical committee for clinical research at Kurume University, Japan, (approval No. 18215). Furthermore, the study was conducted in accordance with the Ethical Guidelines for Clinical Research published by the Ministry of Health, Labour and Welfare on July 30, 2003.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fukahori, S., Yagi, M., Kawahara, H. et al. Current status of intractable pediatric gastroesophageal reflux disease in Japan: a nationwide survey. Surg Today 52, 1153–1159 (2022). https://doi.org/10.1007/s00595-021-02444-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02444-w