Abstract
Purpose
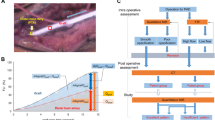
Near-infrared angiography (NIR) is used for on-site graft assessment during coronary artery bypass grafting. This study evaluated the results of a quantitative NIR assessment using a new high-resolution NIR device (h-NIR) for graft assessment.
Methods
Forty-three patients were enrolled in our study. Internal thoracic artery (ITA) grafts anastomosed to the left anterior descending artery and examined intraoperatively using h-NIR were included. The ITA grafts were divided into 2 groups for a comparative analysis: patent grafts (P group; n = 37) and failed grafts (F group; n = 6). The graft flow was evaluated by a “quantitative NIR assessment”, and the fluorescence luminance intensity (FLI) was measured. Direct observation of the graft and anastomosis with h-NIR was also performed.
Results
The FLI was higher in the P group than in the F group. The receiver operating characteristic analysis revealed the following cut-off values for FLIs depending on imaging duration: 21.1% at 1 s, 35.5% at 2 s, 58.4% at 3 s, and 83.3% at 4 s. The sensitivity and specificity for detecting graft failure were 83.3% and 69.8–80.6%, respectively. Furthermore, h-NIR was also able to visualize arterial dissection in ITA grafts.
Conclusions
A quantitative NIR assessment with an h-NIR device can improve the detectability of anastomotic stenosis, and h-NIR successfully detected arterial dissection of grafts.




Similar content being viewed by others
References
Balacumaraswami L, Taggart DP. Intraoperative imaging techniques to assess coronary artery bypass graft patency. Ann Thorac Surg. 2007;83(6):2251–7.
Taggart DP, Choudhary B, Anastasiadis K, Abu-Omar Y, Balacumaraswami L, Pigott DW. Preliminary experience with a novel intraoperative fluorescence imaging technique to evaluate the patency of bypass grafts in total arterial revascularization. Ann Thorac Surg. 2003;75(3):870–3.
Balacumaraswami L, Abu-Omar Y, Choudhary B, Pigott D, Taggart DP. A comparison of transit-time flowmetry and intraoperative fluorescence imaging for assessing coronary artery bypass graft patency. J Thorac Cardiovasc Surg. 2005;130(2):315–20.
Hatada A, Okamura Y, Kaneko M, Hisaoka T, Yamamoto S, Hiramatsu T, et al. Comparison of the waveforms of transit-time flowmetry and intraoperative fluorescence imaging for assessing coronary artery bypass graft patency. Gen Thorac Cardiovasc Surg. 2011;59(1):14–8.
Desai ND, Miwa S, Kodama D, Koyama T, Cohen G, Pelletier MP, et al. A randomized comparison of intraoperative indocyanine green angiography and transit-time flow measurement to detect technical errors in coronary bypass grafts. J Thorac Cardiovasc Surg. 2006;132(3):585–94.
Yamamoto M, Sasaguri S, Sato T. Assessing intraoperative blood flow in cardiovascular surgery. Surg Today. 2011;41(11):1467–74.
Yamamoto M, Orihashi K, Nishimori H, Handa T, Kondo N, Fukutomi T, et al. Efficacy of intraoperative HyperEye medical system angiography for coronary artery bypass grafting. Surg Today. 2015;45(8):966–72.
Desai ND, Miwa S, Kodama D, Cohen G, Christakis GT, Goldman BS, et al. Improving the quality of coronary bypass surgery with intraoperative angiography: validation of a new technique. J Am Coll Cardiol. 2005;46(8):1521–5.
Yamamoto M, Nishimori H, Handa T, Fukutomi T, Kihara K, Tashiro M, et al. Quantitative assessment technique of HyperEye medical system angiography for coronary artery bypass grafting. Surg Today. 2017;47(2):210–7.
Yamamoto M, Orihashi K, Nishimori H, Wariishi S, Fukutomi T, Kondo N, et al. Indocyanine green angiography for intra-operative assessment in vascular surgery. Eur J Vasc Endovasc Surg. 2012;43(4):426–32.
Seki Y, Kajikawa A, Yamamoto T, Takeuchi T, Terashima T, Kurogi N. Real-time indocyanine green videolymphography navigation for lymphaticovenular anastomosis. Plast Reconstr Surg Glob Open. 2019;7(5):e2253.
Campeau L. Letter: grading of angina pectoris. Circulation. 1976;54(3):522–3.
Mohr FW, Morice MC, Kappetein AP, Feldman TE, Stahle E, Colombo A, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381(9867):629–38.
Farooq V, van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381(9867):639–50.
JCS Joint Working Group. Guidelines for the clinical application of bypass grafts and the surgical techniques (JCS 2011) published in 2012–digest version. Circ J. 2013;77(6):1608–41.
Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;28(3):616–26.
FitzGibbon GM, Burton JR, Leach AJ. Coronary bypass graft fate: angiographic grading of 1400 consecutive grafts early after operation and of 1132 after one year. Circulation. 1978;57(6):1070–4.
Harskamp RE, Williams JB, Hill RC, de Winter RJ, Alexander JH, Lopes RD. Saphenous vein graft failure and clinical outcomes: toward a surrogate end point in patients following coronary artery bypass surgery? Am Heart J. 2013;165(5):639–43.
Handa T, Katare RG, Sasaguri S, Sato T. Preliminary experience for the evaluation of the intraoperative graft patency with real color charge-coupled device camera system: an advanced device for simultaneous capturing of color and near-infrared images during coronary artery bypass graft. Interact Cardiovasc Thorac Surg. 2009;9(2):150–4.
Handa T, Orihashi K, Nishimori H, Fukutomi T, Yamamoto M, Kondo N, et al. Maximal blood flow acceleration analysis in the early diastolic phase for in situ internal thoracic artery bypass grafts: a new transit-time flow measurement predictor of graft failure following coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2015;20(4):449–57.
D’Ancona G, Bartolozzi F, Bogers AJ, Pilato M, Parrinello M, Kappetein AP. Intraoperative graft patency verification in coronary artery surgery: modern diagnostic tools. J Cardiothorac Vasc Anesth. 2009;23(2):232–8.
Yamamoto M, Nishimori H, Fukutomi T, Handa T, Kihara K, Tashiro M, et al. Influence of vessel stenosis on indocyanine green fluorescence intensity assessed by near-infrared fluorescence angiography. Surg Today. 2017;47(7):877–82.
Yamamoto M, Ninomiya H, Miyashita K, Tashiro M, Orihashi K, Inoue K, et al. Influence of residual coronary flow on bypass graft flow for graft assessment using near-infrared fluorescence angiography. Surg Today. 2020;50(1):76–83.
Murai T, Lee T, Yonetsu T, Iwai T, Takagi T, Hishikari K, et al. Variability of microcirculatory resistance index and its relationship with fractional flow reserve in patients with intermediate coronary artery lesions. Circ J. 2013;77(7):1769–76.
Koyama K, Yoneyama K, Tsukahara M, Kuwata S, Mitarai T, Kamijima R, et al. A rare case of spontaneous dissection in a left internal mammary artery bypass graft in acute coronary syndrome. JACC Cardiovasc Interv. 2015;8(7):996–7.
Shintani Y, Iino K, Yamamoto Y, Kato H, Takemura H, Kiwata T. Analysis of computational fluid dynamics and particle image velocimetry models of distal-end side-to-side and end-to-side anastomoses for coronary artery bypass grafting in a pulsatile flow. Circ J. 2017;82(1):110–7.
Acknowledgements
We would like to thank the following clinical engineers for their technical support with the manipulation of the NIR device: Tomotaka Takeshima, Kazuhiro Imakubo, and Yoshinori Nomura. We also salute the co-medical staff and surgeons affiliated with the Department of Surgery 2, who performed the surgeries.
Funding
This work was supported by the Japan Society for the Promotion of Science KAKENHI [Grant Number 20437718] and Fujita Memorial Fund for Medical Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 Near-infrared fluorescence angiographic image of case 1. There was 90% stenosis at the anastomotic site between the LITA and LAD, but the FLI of the LITA was increased. FLI, fluorescence luminance intensity; LITA, left internal thoracic artery; LAD, left anterior descending; SV, saphenous vein; RCA, right coronary artery; LCX, left circumflex artery (MPG 21514 KB)
595_2021_2357_MOESM2_ESM.tif
Supplementary file2 Correlation diagram comparing the fluorescence luminance intensity (FLI) and mean graft flow (MGF) (a) 1 s after graft enhancement, (b) 2 s after graft enhancement, (c) 3 s after graft enhancement, and (d) 4 s after graft enhancement. (TIF 193 KB)
Supplementary file3 Near-infrared fluorescence angiographic image. The FLI of LITA graft enhancement. Note that a fluorescence-lucent area suggesting graft dissection was observed in the LITA (arrow). FLI, fluorescence luminance intensity; LITA, left internal thoracic artery (MPG 21120 KB)
Rights and permissions
About this article
Cite this article
Yamamoto, M., Ninomiya, H., Handa, T. et al. The impact of the quantitative assessment procedure for coronary artery bypass graft evaluations using high-resolution near-infrared fluorescence angiography. Surg Today 52, 485–493 (2022). https://doi.org/10.1007/s00595-021-02357-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02357-8