Abstract
Purpose
To compare the outcomes of laparoscopic radical antegrade modular pancreatosplenectomy (L-RAMPS) with those of open RAMPS (O-RAMPS) in patients with pancreatic ductal adenocarcinoma (PDAC).
Methods
We reviewed, retrospectively, the medical records of 50 patients who underwent RAMPS for PDAC without resection of major vessels and adjacent organs between 2007 and 2019, and analyzed the relationship between the operative method and surgical and oncological outcomes.
Results
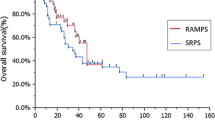
Nineteen of the 50 patients underwent L-RAMPS and 31 patients underwent O-RAMPS. L-RAMPS was associated with significantly less blood loss (P = 0.034) but a longer operative time (P = 0.001) than O-RAMPS. There were no significant differences in patient characteristics, tumor factors, or postoperative course; or in the rates of recurrence-free survival (P = 0.084) or overall survival (P = 0.402) between the L-RAMPS and O-RAMPS groups.
Conclusion
L-RAMPS for PDAC resulted in less blood loss but a longer operative time than O-RAMPS. Although L-RAMPS may be feasible, the operative time needs to be reduced by standardizing the procedure.


Similar content being viewed by others
References
Raimondi S, Maisonneuve P, Lowenfels AB. Epidemiology of pancreatic cancer: an overview. Nat Rev Gastroenterol Hepatol. 2009;6:699–708.
Björnsson B, Larsson AL, Hjalmarsson C, Gasslander T, Sandström P. Comparison of the duration of hospital stay after laparoscopic or open distal pancreatectomy: randomized controlled trial. Br J Surg. 2020;107:1281–8.
Matsumoto I, Kamei K, Satoi S, Murase T, Matsumoto M, Kawaguchi K, et al. Laparoscopic versus open distal pancreatectomy for benign and low-grade malignant lesions of the pancreas: a single-center comparative study. Surg Today. 2019;49:394–400.
Ohtsuka T, Ban D, Nakamura Y, Nagakawa Y, Tanabe M, Gotoh Y, et al. Difficulty scoring system in laparoscopic distal pancreatectomy. J Hepatobiliary Pancreat Sci. 2018;25:489–97.
Stauffer JA, Coppola A, Mody K, Asbun HJ. Laparoscopic versus open distal pancreatectomy for pancreatic adenocarcinoma. World J Surg. 2016;40:1477–84.
Chen K, Tong Q, Yan JF, Huang CJ, Pan Y, Zhang RC, et al. Laparoscopic versus open distal pancreatectomy for pancreatic ductal adenocarcinoma: a single-center propensity score matching study. Updates Surg. 2020;72:387–97.
Miyasaka Y, Ohtsuka T, Nakamura M. Minimally invasive surgery for pancreatic cancer. Surg Today. 2021;51:194–203.
Miao Y, Lu Z, Yeo CJ, Vollmer CM Jr, Fernandez-Del Castillo C, Ghaneh P, et al. Management of the pancreatic transection plane after left (distal) pancreatectomy: expert consensus guidelines by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2020;168:72–84.
Strasberg SM, Drebin JA, Linehan D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003;133:521–7.
Zhang H, Li Y, Liao Q, Xing C, Ding C, Zhang T, et al. Comparison of minimal invasive versus open radical antegrade modular pancreatosplenectomy (RAMPS) for pancreatic ductal adenocarcinoma: a single center retrospective study. Surg Endosc. 2020. https://doi.org/10.1007/s00464-020-07938-1.
Ome Y, Hashida K, Yokota M, Nagahisa Y, Michio O, Kawamoto K. Laparoscopic radical antegrade modular pancreatosplenectomy for left-sided pancreatic cancer using the ligament of Treitz approach. Surg Endosc. 2017;31:4836–7.
Sobin LH, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumors. 7th ed. New York: Wiley; 2011.
Bassi C, Marchegiani G, Dervinis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPF) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–91.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8.
Strasberg SM, Linehan DC, Hawkins WG. Radical antegrade modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg. 2007;204:244–9.
Abe T, Ohuchida K, Miyasaka Y, Ohtsuka T, Oda Y, Nakamura M. Comparison of surgical outcomes between radical antegrade modular pancreatosplenectomy (RAMPS) and standard retrograde pancreatosplenectomy (SPRS) for left-sided pancreatic cancer. World J Surg. 2016;40:2267–75.
Chun YS. Role of radical antegrade modular pancreatosplenectomy (RAMPS) and pancreatic cancer. Ann Surg Oncol. 2018;25:46–50.
Shimada K, Sakamoto Y, Sano T, Kosuge T. Prognostic factors after distal pancreatectomy with extended lymphadenectomy for invasive pancreatic adenocarcinoma of the body and tail. Surgery. 2006;139:288–95.
Kawabata Y, Hayashi H, Kaji S, Fujii Y, Nishi T, Tajima Y. Laparoscopic versus open radical antegrade modular pancreatosplenectomy with artery-first approach in pancreatic cancer. Langenbecks Arch Surg. 2020;405:647–56.
Yang DJ, Xiong JJ, Lu HM, Wei Y, Zhang L, Lu S, et al. The oncological safety in minimally invasive versus open distal pancreatectomy for pancreatic ductal adenocarcinoma: a systematic review and meta-analysis. Sci Rep. 2019;9:1159.
van Hilst J, de Rooij T, Klompmaker S, Rawashdeh M, Aleotti F, Al-Sarireh B, et al. Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a pan-European propensity score matched study. Ann Surg. 2019;269:10–7.
de Rooij T, Cipriani F, Rawashdeh M, van Dieren S, Barbaro S, Abuawwad M, et al. Single-surgeon learning curve in 111 laparoscopic distal pancreatectomies: does operative time tell the whole story? J Am Coll Surg. 2017;224:826–32.
Nakamura Y, Matsushita A, Katsuno A, Sumiyoshi H, Yoshioka M, Shimizu T, et al. Laparoscopic distal pancreatectomy: educating surgeons about advanced laparoscopic surgery. Asian J Endosc Surg. 2014;7:295–300.
Hua Y, Javed AA, Burkhart RA, Makary MA, Weiss MJ, Wolfgang CL, et al. Preoperative risk factors for conversion and learning curve of minimally invasive distal pancreatectomy. Surgery. 2017;162:1040–7.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirashita, T., Iwashita, Y., Fujinaga, A. et al. Surgical and oncological outcomes of laparoscopic versus open radical antegrade modular pancreatosplenectomy for pancreatic ductal adenocarcinoma. Surg Today 52, 224–230 (2022). https://doi.org/10.1007/s00595-021-02326-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02326-1