Abstract
Purpose
Predicting increased blood loss based on anatomical intervascular relationships is essential in major hepatectomy.
Methods
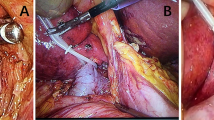
We assessed 63 consecutive patients undergoing anatomical hepatectomy exposing the hepatic vein (HV) trunk at two institutes. Correlations between anatomical alterations of the hepatic inferior vena cava (IVC), HV, hepatic IVC, or right atrium (RA) and the blood loss per standard weight (BLSW) or blood transfusion (n = 18) were analyzed. The results of IVC partial clamping (PC) were additionally examined.
Results
The BLSW in type V-up anatomical morphology was significantly higher than that in straight type (p < 0.05). The parameters associated with an increased BLSW (> 13.5 mL/kg) were tumor size (> 4 cm), prothrombin activity (< 87%), CVP (> 7 mmHg), area of suprahepatic IVC (< 360 mm2), IVC-RA gap (> 28 mm), longitudinal angle of IVC (< 160°), and axial angle of the MHV (< 55°). A multivariate analysis revealed that a high IVC-RA gap was a significant independent risk factor (odds ratio; 4.32, p < 0.05). Among 25 patients undergoing IVC-PC, only three showed a remarkable decrease in hepatic venous bleeding. No other statistically significant differences in the surgical records were observed in most cases.
Conclusion
The IVC-RA gap might be a promising novel predictive parameter reflecting increased blood loss leading to blood transfusion in anatomical hepatectomy.


Similar content being viewed by others
References
Moris D, Tsilimigras DI, Kostakis ID, Ntanasis-Stathopoulos I, Shah KN, Felekouras E, et al. Anatomic versus non-anatomic resection for hepatocellular carcinoma: a systematic review and meta-analysis. Eur J Surg Oncol. 2018;44:927–38.
Shindoh J, Tzeng CW, Aloia TA, Curley SA, Huang SY, Mahvash A, et al. Safety and efficacy of portal vein embolization before planned major or extended hepatectomy: an institutional experience of 358 patients. J Gastrointest Surg. 2014;18:45–51.
Walcott-Sapp S, Billingsley KG. Preoperative optimization for major hepatic resection. Langenbecks Arch Surg. 2018;403:23–35.
Kokudo N, Takemura N, Ito K, Mihara F. The history of liver surgery: achievements over the past 50 years. Ann Gastroenterol Surg. 2020;4:109–17.
Fuchs J, Warmann SW, Szavay P, Kirschner HJ, Schäfer JF, Hennemuth A, et al. Three-dimensional visualization and virtual simulation of resections in pediatric solid tumors. J Pediatr Surg. 2005;40:364–70.
Nanashima A, Sumida Y, Abo T, Tanaka K, Takeshita H, Hidaka S, et al. Principle of perioperative management for hepatic resection and education for young surgeons. Hepato-Gastroenterology. 2008;55:587–91.
Geller DA, Tsung A, Maheshwari V, Rutstein LA, Fung JJ, Marsh JW. Hepatic resection in 170 patients using saline-cooled radiofrequency coagulation. HPB (Oxford). 2005;7:208–13.
Coppa J, Citterio D, Cotsoglou C, Germini A, Piccioni F, Sposito C, et al. Transhepatic anterior approach to the inferior vena cava in large retroperitoneal tumors resected en bloc with the right liver lobe. Surgery. 2013;154:1061–8.
Donati M, Stang A, Stavrou GA, Basile F, Oldhafer KJ. Extending resectability of hilar cholangiocarcinomas: how can it be assessed and improved? Future Oncol. 2019;15:193–205.
Kamiyama T, Kakisaka T, Orimo T. Current role of intraoperative ultrasonography in hepatectomy. Surg Today. 2021. https://doi.org/10.1007/s00595-020-02219-9.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
Schiergens TS, Stielow C, Schreiber S, Hornuss C, Jauch KW, Rentsch M, et al. Liver resection in the elderly: significance of comorbidities and blood loss. J Gastrointest Surg. 2014;18:1161–70.
Latchana N, Hirpara DH, Hallet J, Karanicolas PJ. Red blood cell transfusion in liver resection. Langenbecks Arch Surg. 2019;404:1–9.
Houben P, Hinz U, Knebel P, Diener MK, Mehrabi A, Schemmer P. Randomized controlled trial on Pringle maneuver to reduce blood loss during stapler hepatectomy—PriMal StHep. BMC Surg. 2019;19:60.
Nanashima A, Ariizumi SI, Yamamoto M. Right anatomical hepatectomy: pioneers, evolution, and the future. Surg Today. 2020;50:97–105.
Okuno A, Kimura F, Nakagawa K, Shimizu H, Yoshidome H, Ohtsuka M, et al. Effects of partial hepatic venous congestion on hepatic hemodynamics and histology. Hepato-Gastroenterology. 2010;57:127–33.
Garcea G, Maddern GJ. Liver failure after major hepatic resection. J Hepatobiliary Pancreat Surg. 2009;16:145–55.
Rahbari NN, Koch M, Mehrabi A, Weidmann K, Motschall E, Kahlert C, et al. Portal triad clamping versus vascular exclusion for vascular control during hepatic resection: a systematic review and meta-analysis. J Gastrointest Surg. 2009;13:558–68.
Imamura T, Yamamoto Y, Sugiura T, Okamura Y, Ito T, Ashida R, et al. Infrahepatic inferior vena cava semi-clamping can reduce blood loss during hepatic resection but still requires monitoring to avoid acute kidney injury. World J Surg. 2019;43:2038–47.
Hemming AW, Mekeel KL, Zendejas I, Kim RD, Sicklick JK, Reed AI. Resection of the liver and inferior vena cava for hepatic malignancy. J Am Coll Surg. 2013;217:115–24.
Zatloukal J, Pradl R, Kletecka J, Skalicky T, Liska V, Benes J. Comparison of absolute fluid restriction versus relative volume redistribution strategy in low central venous pressure anesthesia in liver resection surgery: a randomized controlled trial. Minerva Anestesiol. 2017;83:1051–60.
Sakamoto K, Ogawa K, Matsui T, Utsunomiya T, Honjo M, Ueno Y, et al. Vertical interval between hepatic segment of inferior vena cava and right atrium predicts intraoperative blood loss during hemi-hepatectomy. J Hepatobiliary Pancreat Sci. 2020;27:90–100.
Nanashima A, Tobinaga S, Abo T, Nonaka T, Sawai T, Nagayasu T. Usefulness of the combination procedure of crash clamping and vessel sealing for hepatic resection. J Surg Oncol. 2010;102:179–83.
Hamada T, Nanashima A, Yano K, Sumida Y, Hiyoshi M, Imamura N, et al. Significance of a soft-coagulation system with monopolar electrode for hepatectomy: a retrospective two-institution study by propensity analysis. Int J Surg. 2017;45:149–55.
Takasaki T, Kobayashi S, Suzuki S, Muto H, Marada M, Yamana Y, et al. Predetermining postoperative hepatic function for hepatectomies. Int Surg. 1980;65:309.
Kubota K, Makuuchi M, Kusaka K, Kobayashi T, Miki K, Hasegawa K, et al. Measurement of liver volume and hepatic functional reserve as a guide to decision-making in resection surgery for hepatic tumors. Hepatology. 1997;26:1176.
Nanashima A, Tobinaga S, Abo T, Sumida Y, Araki M, Hayashi H, et al. Relationship of hepatic functional parameters with changes of functional liver volume using Technetium-99m galactosyl serum albumin scintigraphy in patients undergoing preoperative portal vein embolization: a follow-up report. J Surg Res. 2010;164:e235–42.
Herz S, Puhl G, Spies C, Jörres D, Neuhaus P, von Heymann C. Perioperative anesthesia management of extended partial liver resection. Pathophysiology of hepatic diseases and functional signs of hepatic failure. Anaesthesist. 2011;60:103–17.
Nanashima A, Hiyoshi A, Imamura N, Yano K, Hamada T, Wada T, et al. Validation set analysis to predict postoperative outcomes by Technetium-99m galactosyl serum albumin scintigraphy for hepatectomy. Nucl Med Commun. 2020;41:320–6.
Arora Satyam, Marwaha Neelam, Dhawan Hari Krishan, Rao KLN. Dedicated donor unit transfusions reduces donor exposure in pediatric surgery patients. Asian J Transfus Sci. 2017;11:124–30.
van Gulik TM, de Graaf W, Dinant S, Busch OR, Gouma DJ. Vascular occlusion techniques during liver resection. Dig Surg. 2007;24:274–81.
Hughes MJ, Ventham NT, Harrison EM, Wigmore SJ. Central venous pressure and liver resection: a systematic review and meta-analysis. HPB (Oxford). 2015;17:863–71.
Yoneda G, Katagiri S, Yamamoto M. Reverse Trendelenburg position is a safer technique for lowering central venous pressure without decreasing blood pressure than clamping of the inferior vena cava below the liver. J Hepatobiliary Pancreat Sci. 2015;22:463–536.
Zhu P, Lau WY, Chen YF, Zhang BX, Huang ZY, Zhang ZW, et al. Randomized clinical trial comparing infrahepatic inferior vena cava clamping with low central venous pressure in complex liver resections involving the Pringle manoeuvre. Br J Surg. 2012;99:781–8.
Imamura T, Yamamoto Y, Sugiura T, Okamura Y, Ito T, Ashida R, et al. Infrahepatic inferior vena cava semi-clamping can reduce blood loss during hepatic resection but still requires monitoring to avoid acute kidney injury. World J Surg. 2019;43:2038–47.
Fan ST. Precise hepatectomy guided by the middle hepatic vein. Hepatobiliary Pancreat Dis Int. 2007;6:430–4.
Nanashima A, Nagayasu T. Development and clinical usefulness of the liver hanging maneuver in various anatomical hepatectomy procedures. Surg Today. 2016;46:398–404.
Nanashima A, Sumida Y, Abo T, Nagayasu T, Sawai T. Usefulness and application of the liver hanging maneuver for anatomical liver resections. World J Surg. 2008;32:2070–6.
Nanashima A, Abo T, Arai J, Takagi K, Matsumoto H, Takeshita H, et al. Usefulness of vessel-sealing devices combined with crush clamping method for hepatectomy: a retrospective cohort study. Int J Surg. 2013;11:891–7.
Nanashima A, Tobinaga S, Abo T, Nonaka T, Takeshita H, Hidaka S, et al. Reducing the incidence of post-hepatectomy hepatic complications by preoperatively applying parameters predictive of liver function. J HBPS. 2010;17:871–8.
Nanashima A, Sakamoto A, Sakamoto I, Hayashi H, Abo T, Wakata K, et al. Usefulness of evaluating hepatic elasticity using artificial acoustic radiation force ultrasonography before hepatectomy. Hepatol Res. 2014;44:1308–19.
Liu XJ, Zhang JF, Sui HJ, Yu SB, Gong J, Liu J, et al. A comparison of hepatic segmental anatomy as revealed by cross-sections and MPR CT imaging. Clin Anat. 2013;26:486–92.
Wada H, Eguchi H, Nagano H, Kubo S, Nakai T, Kaibori M, et al. Perioperative allogenic blood transfusion is a poor prognostic factor after hepatocellular carcinoma surgery: a multi-center analysis. Surg Today. 2018;48:73–9.
Mehrabi A, Mood ZA, Roshanaei N, Fonouni H, Müller SA, Schmied BM, et al. Mesohepatectomy as an option for the treatment of central liver tumors. J Am Coll Surg. 2008;207:499–509.
Acknowledgements
The principal author sincerely appreciates Professor Naoaki Ichihara for giving instructions regarding statistical limitations during the revision process.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nanashima, A., Tanoue, Y., Sakae, T. et al. Relationship between hepatic venous anatomy and hepatic venous blood loss during hepatectomy. Surg Today 51, 1953–1968 (2021). https://doi.org/10.1007/s00595-021-02314-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02314-5