Abstract
Purpose
To investigate the relationship between three-dimensional computed tomography (3D-CT) findings and pathological invasiveness in lung adenocarcinoma.
Methods
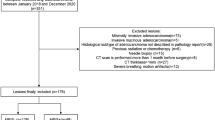
We retrospectively evaluated 95 patients who underwent surgical resection of lung adenocarcinoma of ≤ 20 mm. The diameters, volumes, and CT values of tumor consolidation were analyzed. We defined the modified CT value by setting air as 0 and water as 1000 and assumed a correlation with pathological invasiveness. Pre-invasive lesions and minimally invasive adenocarcinomas were classified as non-invasive adenocarcinoma. We compared the clinico-radiological features with pathological invasiveness. Receiver operator characteristic (ROC) curves and recurrence-free survival curves were constructed.
Results
Twenty-six non-invasive adenocarcinomas and 69 invasive adenocarcinomas were evaluated. The multivariate analysis revealed that the consolidation volume and the integration of modified CT values were the most important predictors of pathological invasion. The area under the ROC curve and the cut-off values of the consolidation volume were 0.868 and 75 mm3, respectively. The area under the ROC curve and the cut-off values of the integration of modified CT values were 0.871 and 80,000, respectively. There was no recurrence in cases with values below the cut-off across all parameters.
Conclusion
The consolidation volume and integration of modified CT values were shown to be highly predictive of pathological invasiveness.




Similar content being viewed by others
References
Matsuda T, Machii R. Morphological distribution of lung cancer from cancer incidence in five continents Vol. X. Jpn J Clin Oncol. 2015;45:404.
Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6:244–85.
Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg. 1995;60:615–22 (discussion 22-3).
Ikeda N, Endo S, Fukuchi E, Nakajima J, Yokoi K, Chida M, et al. Current status of surgery for clinical stage IA lung cancer in Japan: analysis of the national clinical database. Surg Today. 2020;50:1644–51.
Travis WD, Asamura H, Bankier AA, Beasley MB, Detterbeck F, Flieder DB, et al. The IASLC lung cancer staging project: proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM Classification of Lung Cancer. J Thorac Oncol. 2016; 11: 1204–23.
Whitson BA, Groth SS, Andrade RS, Maddaus MA, Habermann EB, D’Cunha J. Survival after lobectomy versus segmentectomy for stage I non-small cell lung cancer: a population-based analysis. Ann Thorac Surg. 2011;92:1943–50.
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, et al. Prediction of pathologic node-negative clinical stage IA lung adenocarcinoma for optimal candidates undergoing sublobar resection. J Thorac Cardiovasc Surg. 2012;144:1365–71.
Suzuki K, Koike T, Asakawa T, Kusumoto M, Asamura H, Nagai K, et al. A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol. 2011;6:751–6.
Yanagawa M, Kusumoto M, Johkoh T, Noguchi M, Minami Y, Sakai F, et al. Radiologic-pathologic correlation of solid portions on thin-section CT images in lung adenocarcinoma: a multicenter study. Clin Lung Cancer. 2018;19:e303–12.
Aokage K, Yoshida J, Ishii G, Matsumura Y, Haruki T, Hishida T, et al. Identification of early t1b lung adenocarcinoma based on thin-section computed tomography findings. J Thorac Oncol. 2013;8:1289–94.
Asamura H, Hishida T, Suzuki K, Koike T, Nakamura K, Kusumoto M, et al. Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg. 2013;146:24–30.
Huang TW, Lin KH, Huang HK, Chen YI, Ko KH, Chang CK, et al. The role of the ground-glass opacity ratio in resected lung adenocarcinoma. Eur J Cardiothorac Surg. 2018;54:229–34.
Matsunaga T, Suzuki K, Takamochi K, Oh S. What is the radiological definition of part-solid tumour in lung cancer? Eur J Cardiothorac Surg. 2017;51:242–7.
Haraguchi N, Satoh H, Kikuchi N, Kagohashi K, Ishikawa H, Ohtsuka M. Prognostic value of tumor disappearance rate on computed tomography in advanced-stage lung adenocarcinoma. Clin Lung Cancer. 2007;8:327–30.
Shimizu K, Yamada K, Saito H, Noda K, Nakayama H, Kameda Y, et al. Surgically curable peripheral lung carcinoma: correlation of thin-section CT findings with histologic prognostic factors and survival. Chest. 2005;127:871–8.
Kim D, Kim HK, Kim SH, Lee HY, Cho JH, Choi YS, et al. Prognostic significance of histologic classification and tumor disappearance rate by computed tomography in lung cancer. J Thorac Dis. 2018;10:388–97.
Lee HY, Lee SW, Lee KS, Jeong JY, Choi JY, Kwon OJ, et al. Role of CT and PET imaging in predicting tumor recurrence and survival in patients with lung adenocarcinoma: a comparison with the international association for the study of lung cancer/American Thoracic Society/European Respiratory Society Classification of Lung Adenocarcinoma. J Thorac Oncol. 2015;10:1785–94.
Kitami A, Kamio Y, Hayashi S, Suzuki K, Uematsu S, Gen R, et al. One-dimensional mean computed tomography value evaluation of ground-glass opacity on high-resolution images. Gen Thorac Cardiovasc Surg. 2012;60:425–30.
Tamura M, Shimizu Y, Yamamoto T, Yoshikawa J, Hashizume Y. Predictive value of one-dimensional mean computed tomography value of ground-glass opacity on high-resolution images for the possibility of future change. J Thorac Oncol. 2014;9:469–72.
Kitazawa S, Saeki Y, Kobayashi N, Kikuchi S, Goto Y, Sato Y. Three-dimensional mean CT attenuation value of pure and part-solid ground-glass lung nodules may predict invasiveness in early adenocarcinoma. Clin Radiol. 2019;74:944–9.
Suzuki K, Asamura H, Kusumoto M, Kondo H, Tsuchiya R. “Early” peripheral lung cancer: prognostic significance of ground glass opacity on thin-section computed tomographic scan. Ann Thorac Surg. 2002;74:1635–9.
Yim J, Zhu LC, Chiriboga L, Watson HN, Goldberg JD, Moreira AL. Histologic features are important prognostic indicators in early stages lung adenocarcinomas. Mod Pathol. 2007;20:233–41.
Maeshima AM, Tochigi N, Yoshida A, Asamura H, Tsuta K, Tsuda H. Histological scoring for small lung adenocarcinomas 2 cm or less in diameter: a reliable prognostic indicator. J Thorac Oncol. 2010;5:333–9.
Furumoto H, Shimada Y, Imai K, Maehara S, Maeda J, Hagiwara M, et al. Prognostic impact of the integration of volumetric quantification of the solid part of the tumor on 3DCT and FDG-PET imaging in clinical stage IA adenocarcinoma of the lung. Lung Cancer. 2018;121:91–6.
Takenaka T, Yamazaki K, Miura N, Mori R, Takeo S. The prognostic impact of tumor volume in patients with clinical stage ia non-small cell lung cancer. J Thorac Oncol. 2016;11:1074–80.
Berghmans T, Dusart M, Paesmans M, Hossein-Foucher C, Buvat I, Castaigne C, et al. Primary tumor standardized uptake value (SUVmax) measured on fluorodeoxyglucose positron emission tomography (FDG-PET) is of prognostic value for survival in non-small cell lung cancer (NSCLC): a systematic review and meta-analysis (MA) by the European Lung Cancer Working Party for the IASLC Lung Cancer Staging Project. J Thorac Oncol. 2008;3:6–12.
Huang TW, Hsieh CM, Chang H, Cheng YL, Tzao C, Huang WS, et al. Standard uptake value of positron emission tomography in clinical stage I lung cancer: clinical application and pathological correlation. Eur J Cardiothorac Surg. 2012;41:869–73.
Carrillo SA, Daniel VC, Hall N, Hitchcock CL, Ross P Jr, Kassis ES. Fusion positron emission/computed tomography underestimates the presence of hilar nodal metastases in patients with resected non-small cell lung cancer. Ann Thorac Surg. 2012;93:1621–4.
Sawabata N, Kanzaki R, Sakamoto T, Kusumoto H, Kimura T, Nojiri T, et al. Clinical predictor of pre- or minimally invasive pulmonary adenocarcinoma: possibility of sub-classification of clinical T1a. Eur J Cardiothorac Surg. 2014;45:256–61.
Keyes JW Jr. SUV: standard uptake or silly useless value? J Nucl Med. 1995;36:1836–9.
Acknowledgements
The authors thank Kazushi Maruo of Department of Biostatistics, University of Tsukuba, for consultation on statistical methods and Thomas D. Mayers of the Medical English Communications Center, University of Tsukuba, for revision of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors contributed to the final manuscript, and none of the authors had any conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saeki, Y., Kitazawa, S., Yanagihara, T. et al. Consolidation volume and integration of computed tomography values on three-dimensional computed tomography may predict pathological invasiveness in early lung adenocarcinoma. Surg Today 51, 1320–1327 (2021). https://doi.org/10.1007/s00595-021-02231-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02231-7