Abstract
Purpose
Trimodality therapy, comprised of induction chemoradiotherapy (iCRT) followed by surgery, is a highly invasive treatment option for locally advanced non-small cell lung cancers (LA-NSCLCs; defined as a heterogenous disease). We conducted this study to investigate the prognostic nutritional index (PNI) of LA-NSCLC patients undergoing trimodality therapy, which has not been studied in detail before.
Methods
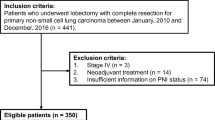
The subjects of this retrospective study were 127 patients who underwent trimodality therapy between 1999 and 2016. We measured the PNI at three points: before iCRT (pre-iCRT), before the operation, and after the operation.
Results
PNIs decreased significantly as treatment progressed. Patients with clinical T3/4 (cT3/4) disease had a significantly lower PNI than those with cT1/2 disease, but the extent of lymph-node metastasis did not affect the PNI at any point. Using the cut-off values of receiver-operating curve analyses, multivariable analyses revealed that a high PNI pre-iCRT correlated significantly with a better survival of LA-NSCLC patients, especially those with cT3/4 disease (hazard ratio 3.84; 95% confidential interval 1.34–12.5, P = 0.012).
Conclusions
Measuring the PNI before trimodality therapy is important for predicting the clinical outcome of patients with LA-NSCLC, with differing predictive ability according to the disease extent. Perioperative intensive nutritional intervention must be considered for patients who undergo trimodality therapy for LA-NSCLC.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Albain KS, Swann RS, Rusch VW, Turrisi AT 3rd, Shepherd FA, Smith C, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet. 2009;374(9687):379–86.
Toyooka S, Kiura K, Takemoto M, Oto T, Takigawa N, Fujiwara T, et al. Long-term outcome of induction chemoradiotherapy with docetaxel and cisplatin followed by surgery for non-small-cell lung cancer with mediastinal lymph node metastasis. Interact Cardiovasc Thorac Surg. 2012;14(5):565–9.
Kiss N. Nutrition support and dietary interventions for patients with lung cancer: current insights. Lung Cancer (Auckl). 2016;7:1–9.
Andreyev HJ, Norman AR, Oates J, Cunningham D. Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies? Eur J Cancer. 1998;34(4):503–9.
Pressoir M, Desne S, Berchery D, Rossignol G, Poiree B, Meslier M, et al. Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer. 2010;102(6):966–71.
Segura A, Pardo J, Jara C, Zugazabeitia L, Carulla J, de Las PR, et al. An epidemiological evaluation of the prevalence of malnutrition in Spanish patients with locally advanced or metastatic cancer. Clin Nutr. 2005;24(5):801–14.
Mariani L, Lo Vullo S, Bozzetti F, Group SW. Weight loss in cancer patients: a plea for a better awareness of the issue. Suppor Care Cancer. 2012;20(2):301–9.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai zasshi. 1984;85(9):1001–5.
Shimizu K, Okita R, Saisho S, Maeda A, Nojima Y, Nakata M. Preoperative neutrophil/lymphocyte ratio and prognostic nutritional index predict survival in patients with non-small cell lung cancer. World J Surg Oncol. 2015;13:291.
Kuroda D, Sawayama H, Kurashige J, Iwatsuki M, Eto T, Tokunaga R, et al. Controlling Nutritional Status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer. 2018;21(2):204–12.
Miyazaki T, Yamasaki N, Tsuchiya T, Matsumoto K, Kunizaki M, Taniguchi D, et al. Inflammation-based scoring is a useful prognostic predictor of pulmonary resection for elderly patients with clinical stage I non-small-cell lung cancer. Eur J Cardiothorac Surg. 2015;47(4):e140–e145145.
Hofbauer SL, Pantuck AJ, de Martino M, Lucca I, Haitel A, Shariat SF, et al. The preoperative prognostic nutritional index is an independent predictor of survival in patients with renal cell carcinoma. Urol Oncol. 2015;33(2):68.e1–.e7.
Yang Y, Gao P, Chen X, Song Y, Shi J, Zhao J, et al. Prognostic significance of preoperative prognostic nutritional index in colorectal cancer: results from a retrospective cohort study and a meta-analysis. Oncotarget. 2016;7(36):58543–52.
Mori S, Usami N, Fukumoto K, Mizuno T, Kuroda H, Sakakura N, et al. The significance of the prognostic nutritional index in patients with completely resected non-small cell lung cancer. PLoS ONE. 2015;10(9):e0136897.
Sheng J, Yang YP, Ma YX, Qin T, Hu ZH, Hong SD, et al. Low prognostic nutritional index correlates with worse survival in patients with advanced NSCLC following EGFR-TKIs. PLoS ONE. 2016;11(1):e0147226.
Nakao M, Muramatsu H, Kagawa Y, Suzuki Y, Sakai Y, Kurokawa R, et al. Immunological status may predict response to nivolumab in non-small cell lung cancer without driver mutations. Anticancer Res. 2017;37(7):3781–6.
Ramnath N, Dilling TJ, Harris LJ, Kim AW, Michaud GC, Balekian AA, et al. Treatment of stage III non-small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e314S–e340.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, et al. The IASLC lung cancer staging project: proposals for revision of the TNM Stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39–51.
Katayama H, Ueoka H, Kiura K, Tabata M, Kozuki T, Tanimoto M, et al. Preoperative concurrent chemoradiotherapy with cisplatin and docetaxel in patients with locally advanced non-small-cell lung cancer. Br J Cancer. 2004;90(5):979–84.
Qiu C, Qu X, Shen H, Zheng C, Zhu L, Meng L, et al. Evaluation of prognostic nutritional index in patients undergoing radical surgery with nonsmall cell lung cancer. Nutr Cancer. 2015;67(5):741–7.
Shoji F, Morodomi Y, Akamine T, Takamori S, Katsura M, Takada K, et al. Predictive impact for postoperative recurrence using the preoperative prognostic nutritional index in pathological stage I non-small cell lung cancer. Lung Cancer. 2016;98:15–211.
Martin TA, Ye L, Sanders AJ, Lane J, Jiang WG. Cancer invasion and metastasis: molecular and cellular perspective. In: Jandail R, editor. Metastatic cancer: clinical and biological perspectives. Austin: Landes Bioscience; 2013. p. 135–68.
Popper HH. Progression and metastasis of lung cancer. Cancer Metastasis Rev. 2016;35(1):75–91.
Jiang WG, Sanders AJ, Katoh M, Ungefroren H, Gieseler F, Prince M, et al. Tissue invasion and metastasis: molecular, biological and clinical perspectives. Semin Cancer Biol. 2015;35(Suppl):S244–S275275.
Mittal A, Bhatnagar S, Kumar A, Lach-Trifilieff E, Wauters S, Li H, et al. The TWEAK-Fn14 system is a critical regulator of denervation-induced skeletal muscle atrophy in mice. J Cell Biol. 2010;188(6):833–49.
Chen KL, Jung P, Kulkoyluoglu-Cotul E, Liguori C, Lumibao J, Mazewski C, et al. Impact of diet and nutrition on cancer hallmarks. J Cancer Prev Curr Res. 2017;7(4):240.
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11–48.
Paccagnella A, Morassutti I, Rosti G. Nutritional intervention for improving treatment tolerance in cancer patients. Curr Opin Oncol. 2011;23(4):322–30.
Acknowledgements
We would like to thank Drs. Akihiro Miura, Shunsaku Miyauchi, Kota Araki, Yuta Takahashi, Eisuke Kurihara, Yusuke Ogoshi, Kei Namba, Takahiro Yoshioka, Hidejiro Torigoe, and Hiroki Sato (Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences) for their help with the collection of data from the medical records. This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to disclose in relation to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
595_2020_2067_MOESM1_ESM.tif
Supplementary file1 Prognostic role of PNI before surgery on clinical outcome. The receiver operating curves (ROCs) were generated for all patients (n = 127, a) and for the patients with cT3/4 disease (n = 72, c). The Kaplan-Meier curves of overall survival (OS) and relapse-free survival (RFS) for all the patients (b) and for the patients with cT3/4 disease(d), respectively. The cutoff values of PNI before trimodality therapy for each population were defined by each representative ROC analysis. AUC, area under curve (TIF 21303 kb)
595_2020_2067_MOESM2_ESM.tif
Supplementary file2 Prognostic role of the ratio of PNI before surgery to PNI before trimodality therapy on clinical outcome. The Kaplan-Meier curves of overall survival (OS) and relapse-free survival (RFS) for all patients (a) and for the patients with cT3/4 disease (b), respectively. A ratio of less than 1.0 means the pre-iCRT PNI value was higher than the pre-op PNI value (TIF 21172 kb)
Rights and permissions
About this article
Cite this article
Soh, J., Suzawa, K., Shien, K. et al. Prognostic nutrition index affects the prognosis of patients undergoing trimodality therapy for locally advanced non-small cell lung cancer. Surg Today 50, 1610–1618 (2020). https://doi.org/10.1007/s00595-020-02067-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-02067-7