Abstract
Purpose
Lysophosphatidylcholine (LPC), which is generated from phosphatidylcholine (PC) and metabolized by autotaxin (ATX), modulates immune responses via its anti-inflammatory property. We investigated the association between LPC and postoperative complications (POCs) after colorectal cancer surgery (CRC).
Methods
The subjects of this study were 43 patients who underwent surgery for CRC. Peripheral blood samples were collected preoperatively and immediately after surgery, and on postoperative days (PODs) 1, 3, 5, and 7. Patients were divided into a No-POC group (n = 33) and a POC group (n = 10). Blood LPC, IL-6, PC, and ATX levels were measured by specific enzymatic assays or ELISA.
Results
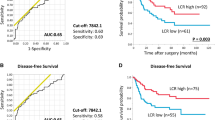
The postoperative to preoperative LPC ratios were lowest on POD 1 in both groups. The POC group had significantly lower LPC ratios throughout the perioperative period than the No-POC group. The LPC ratios were inversely correlated with IL-6. The predictive impact of LPC ratios on POCs was demonstrated by ROC analysis (cut-off 51.2%, AUC 0.798) and multivariate analysis (OR 15.1, P = 0.01). The postoperative PC ratios decreased more after surgery in the POC group. ATX levels did not change significantly in either group.
Conclusions
Decreased postoperative LPC is associated with increased postoperative inflammatory response and POCs. The decreased PC supply to the circulation is a mechanism of the postoperative LPC decrease.




Similar content being viewed by others
References
Projected cancer statistics, 2017 https://ganjoho.jp/en/public/statistics/short_pred.html.
Oliphant R, Nicholson GA, Horgan PG, McMillan DC, Morrison DS, West of Scotland Colorectal Cancer Managed Clinical N. The impact of surgical specialisation on survival following elective colon cancer surgery. Int J Colorectal Dis. 2014;29:1143–50.
Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81.
Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K, et al. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg. 2005;140:278–83 (discussion 284).
Sjo OH, Larsen S, Lunde OC, Nesbakken A. Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis. 2009;11:733–9.
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg. 2015;261:497–505.
Brown SR, Mathew R, Keding A, Marshall HC, Brown JM, Jayne DG. The impact of postoperative complications on long-term quality of life after curative colorectal cancer surgery. Ann Surg. 2014;259:916–23.
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011;253:890–9.
Richards CH, Platt JJ, Anderson JH, McKee RF, Horgan PG, McMillan DC. The impact of perioperative risk, tumor pathology and surgical complications on disease recurrence following potentially curative resection of colorectal cancer. Ann Surg. 2011;254:83–9.
Bulger EM, Maier RV. Lipid mediators in the pathophysiology of critical illness. Crit Care Med. 2000;28:N27–36.
Kabarowski JH, Xu Y, Witte ON. Lysophosphatidylcholine as a ligand for immunoregulation. Biochem Pharmacol. 2002;64:161–7.
Kume N, Gimbrone MA Jr.. Lysophosphatidylcholine transcriptionally induces growth factor gene expression in cultured human endothelial cells. J Clin Investig. 1994;93:907–11.
Sevastou I, Kaffe E, Mouratis MA, Aidinis V. Lysoglycerophospholipids in chronic inflammatory disorders: the PLA(2)/LPC and ATX/LPA axes. Biochim Biophys Acta. 2013;1831:42–60.
Kabarowski JH, Zhu K, Le LQ, Witte ON, Xu Y. Lysophosphatidylcholine as a ligand for the immunoregulatory receptor G2A. Science. 2001;293:702–5.
Le LQ, Kabarowski JH, Weng Z, Satterthwaite AB, Harvill ET, Jensen ER, et al. Mice lacking the orphan G protein-coupled receptor G2A develop a late-onset autoimmune syndrome. Immunity. 2001;14:561–71.
Park DW, Kwak DS, Park YY, Chang Y, Huh JW, Lim CM, et al. Impact of serial measurements of lysophosphatidylcholine on 28-day mortality prediction in patients admitted to the intensive care unit with severe sepsis or septic shock. J Crit Care. 2014;29:882 e885-811.
Cho WH, Park T, Park YY, Huh JW, Lim CM, Koh Y, et al. Clinical significance of enzymatic lysophosphatidylcholine (LPC) assay data in patients with sepsis. Eur J Clin Microbiol Infect Dis. 2012;31:1805–10.
Drobnik W, Liebisch G, Audebert FX, Frohlich D, Gluck T, Vogel P, et al. Plasma ceramide and lysophosphatidylcholine inversely correlate with mortality in sepsis patients. J Lipid Res. 2003;44:754–61.
Yan JJ, Jung JS, Lee JE, Lee J, Huh SO, Kim HS, et al. Therapeutic effects of lysophosphatidylcholine in experimental sepsis. Nat Med. 2004;10:161–7.
McSorley ST, Khor BY, MacKay GJ, Horgan PG, McMillan DC. Examination of a CRP first approach for the detection of postoperative complications in patients undergoing surgery for colorectal cancer: a pragmatic study. Medicine (Baltimore). 2017;96:e6133.
McSorley ST, Ramanathan ML, Horgan PG, McMillan DC. Postoperative C-reactive protein measurement predicts the severity of complications following surgery for colorectal cancer. Int J Colorectal Dis. 2015;30:913–7.
Rettig TC, Verwijmeren L, Dijkstra IM, Boerma D, van de Garde EM, Noordzij PG. Postoperative interleukin-6 level and early detection of complications after elective major abdominal surgery. Ann Surg. 2016;263:1207–12.
Watt DG, McSorley ST, Park JH, Horgan PG, McMillan DC. A postoperative systemic inflammation score predicts short- and long-term outcomes in patients undergoing surgery for colorectal cancer. Ann Surg Oncol. 2017;24:1100–9.
Blajchman MA. Immunomodulation and blood transfusion. Am J Ther. 2002;9:389–95.
Chimienti G, Aquilino F, Rotelli MT, Russo F, Lupo L, Pepe G. Lipoprotein(a), lipids and proinflammatory cytokines in patients undergoing major abdominal surgery. Br J Surg. 2006;93:347–53.
Gilliland HE, Armstrong MA, Carabine U, McMurray TJ. The choice of anesthetic maintenance technique influences the antiinflammatory cytokine response to abdominal surgery. Anesth Analg. 1997;85:1394–8.
Veenhof AA, Sietses C, von Blomberg BM, van Hoogstraten IM, vd Pas MH, Meijerink WJ, et al. The surgical stress response and postoperative immune function after laparoscopic or conventional total mesorectal excision in rectal cancer: a randomized trial. Int J Colorectal Dis. 2011;26:53–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Sugiyama S, Kugiyama K, Ogata N, Doi H, Ota Y, Ohgushi M, et al. Biphasic regulation of transcription factor nuclear factor-kappaB activity in human endothelial cells by lysophosphatidylcholine through protein kinase C-mediated pathway. Arterioscler Thromb Vasc Biol. 1998;18:568–76.
Carneiro AB, Iaciura BM, Nohara LL, Lopes CD, Veas EM, Mariano VS, et al. Lysophosphatidylcholine triggers TLR2- and TLR4-mediated signaling pathways but counteracts LPS-induced NO synthesis in peritoneal macrophages by inhibiting NF-kappaB translocation and MAPK/ERK phosphorylation. PLoS One. 2013;8:e76233.
Wang H, Czura CJ, Tracey KJ. Lipid unites disparate syndromes of sepsis. Nat Med. 2004;10:124–5.
Chen G, Li J, Qiang X, Czura CJ, Ochani M, Ochani K, Ulloa L, et al. Suppression of HMGB1 release by stearoyl lysophosphatidylcholine:an additional mechanism for its therapeutic effects in experimental sepsis. J Lipid Res. 2005;46:623–7.
Kabarowski JH. G2A and LPC: regulatory functions in immunity. Prostaglandins Other Lipid Mediat. 2009;89:73–81.
Menger MD, Vollmar B. Surgical trauma: hyperinflammation versus immunosuppression? Langenbecks Arch Surg. 2004;389:475–84.
Roumen RM, Hendriks T, van der Ven-Jongekrijg J, Nieuwenhuijzen GA, Sauerwein RW, van der Meer JW, et al. Cytokine patterns in patients after major vascular surgery, hemorrhagic shock, and severe blunt trauma. Relation with subsequent adult respiratory distress syndrome and multiple organ failure. Ann Surg. 1993;218:769–76.
Mokart D, Merlin M, Sannini A, Brun JP, Delpero JR, Houvenaeghel G, et al. Procalcitonin, interleukin 6 and systemic inflammatory response syndrome (SIRS): early markers of postoperative sepsis after major surgery. Br J Anaesth. 2005;94:767–73.
Korner H, Nielsen HJ, Soreide JA, Nedrebo BS, Soreide K, Knapp JC. Diagnostic accuracy of C-reactive protein for intraabdominal infections after colorectal resections. J Gastrointest Surg. 2009;13:1599–606.
Platt JJ, Ramanathan ML, Crosbie RA, Anderson JH, McKee RF, Horgan PG, et al. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol. 2012;19:4168–77.
Warschkow R, Steffen T, Beutner U, Muller SA, Schmied BM, Tarantino I. Diagnostic accuracy of C-reactive protein and white blood cell counts in the early detection of inflammatory complications after open resection of colorectal cancer: a retrospective study of 1187 patients. Int J Colorectal Dis. 2012;27:1377.
Kishimoto T, Soda Y, Matsuyama Y, Mizuno K. An enzymatic assay for lysophosphatidylcholine concentration in human serum and plasma. Clin Biochem. 2002;35:411–6.
Acknowledgements
This study was supported financially by a Grant-in-Aid for Scientific Research from The Ministry of Education, Culture, Sports, Science and Technology of Japan (15K10037: Matsuda A).
Author information
Authors and Affiliations
Contributions
All authors are in agreement with the content of the manuscript. Authors’ contributions are as follows: study concept and design, AM and MY; acquisition of data, AM and NS; analysis and interpretation of data, AM, MY, SM, TY and TM; drafting of the manuscript, AM; study supervision, MM and EU.
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Matsuda, A., Yamada, M., Matsumoto, S. et al. Lysophosphatidylcholine as a predictor of postoperative complications after colorectal cancer surgery. Surg Today 48, 936–943 (2018). https://doi.org/10.1007/s00595-018-1675-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1675-2