Abstract
Aims
To explore whether breastfeeding affects postpartum insulin requirements, HbA1c levels, and pregnancy weight retention in women with Type 1 Diabetes Mellitus (T1DM).
Methods
This prospective study included 66 women with T1DM. The women were divided into two groups based on whether they were breastfeeding (BF) at 6 months postpartum (BFyes, n = 32) or not (BFno, n = 34). Mean daily insulin requirement (MDIR), HbA1c levels, and pregnancy weight retention at 5 time-points from discharge to 12 months postpartum were compared.
Results
MDIR increased by 35% from 35.7 IU at discharge to 48.1 IU at 12 months postpartum (p < 0.001). MDIR in BFyes and BFno were comparable, however in BFyes, MDIR were continuously lower compared to BFno. Postpartum HbA1c increased rapidly from 6.8% at 1 month to 7.4% at 3 months postpartum and settled at 7.5% at 12 months postpartum. The increase in HbA1c during the first 3 months postpartum was most pronounced in BFno (p < 0.001). Although neither were statistically significant, from 3 months postpartum HbA1c levels were highest in the BFno and BFno had a higher pregnancy weight retention compared to BFyes (p = 0.31).
Conclusion
In women with T1DM, breastfeeding did not significantly affect postpartum insulin requirements, HbA1c levels or pregnancy weight retention in the first year after delivery.



Similar content being viewed by others
References
Bruun S, Wedderkopp N, Mølgaard C et al (2016) Using text messaging to obtain weekly data on infant feeding in a Danish birth cohort resulted in high participation rates. Acta Paediatr Int J Paediatr 105:648–654. https://doi.org/10.1111/APA.13382
Kronborg H, Foverskov E (2014) Væth M (2014) Predictors for early introduction of solid food among Danish mothers and infants: an observational study. BMC Pediatr 141(14):1–10. https://doi.org/10.1186/1471-2431-14-243
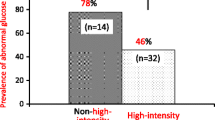
O’Reilly MW, Avalos G, Dennedy MC et al (2011) Atlantic DIP: High prevalence of abnormal glucose tolerance post partum is reduced by breast-feeding in women with prior gestational diabetes mellitus. Eur J Endocrinol 165:953–959. https://doi.org/10.1530/EJE-11-0663
Gunderson EP, Hedderson MM, Chiang V et al (2012) Lactation intensity and postpartum maternal glucose tolerance and insulin resistance in women with recent GDM: the SWIFT cohort. Diabetes Care 35:50–56. https://doi.org/10.2337/dc11-1409
Yasuhi I, Soda T, Yamashita H et al (2017) The effect of high-intensity breastfeeding on postpartum glucose tolerance in women with recent gestational diabetes. Int Breastfeed J 12:32. https://doi.org/10.1186/s13006-017-0123-z
Borgoño CA, Retnakaran R (2012) Higher breastfeeding intensity associated with improved postpartum glucose metabolism in women with recent gestational diabetes. Evid Based Med 17(6):e7
Aune D, Norat T, Romundstad P, Vatten LJ (2014) Breastfeeding and the maternal risk of type 2 diabetes: a systematic review and dose–response meta-analysis of cohort studies. Nutr Metab Cardiovasc Dis 24:107–115. https://doi.org/10.1016/J.NUMECD.2013.10.028
Crume TL, Ogden L, Maligie M et al (2011) Long-term impact of neonatal breastfeeding on childhood adiposity and fat distribution among children exposed to diabetes in utero. Diabetes Care 34:641–645. https://doi.org/10.2337/dc10-1716
Dugas C, Perron J, Kearney M et al (2017) postnatal prevention of childhood obesity in offspring prenatally exposed to gestational diabetes mellitus: Where are we now? Obes Facts. https://doi.org/10.1159/000477407
Pereira PF, Alfenas RDCG, Araújo RMA (2014) Does breastfeeding influence the risk of developing diabetes mellitus in children? A review of current evidence. J Pediatr (Rio J) 90:7–15. https://doi.org/10.1016/j.jped.2013.02.024
Stage E, Nørgård H, Damm P, Mathiesen E (2006) Long-term breast-feeding in women with type 1 diabetes. Diabetes Care 29:771–774. https://doi.org/10.2337/DIACARE.29.04.06.DC05-1103
Finkelstein SA, Keely E, Feig DS et al (2013) Breastfeeding in women with diabetes: lower rates despite greater rewards. A Population Based Study Diabet Med 30:1094–1101. https://doi.org/10.1111/dme.12238
Schoen S, Sichert-Hellert W, Hummel S et al (2008) Breastfeeding duration in families with type 1 diabetes compared to non-affected families: results from BABYDIAB and DONALD studies in Germany. Breastfeed Med 3:171–175. https://doi.org/10.1089/bfm.2007.0027
Sorkio S, Cuthbertson D, Bärlund S et al (2010) Breastfeeding patterns of mothers with type 1 diabetes: results from an infant feeding trial. Diabetes Metab Res Rev 26:206. https://doi.org/10.1002/DMRR.1074
Cundy T, Morgan J, O’Beirne C et al (2013) Obstetric interventions for women with type 1 or type 2 diabetes. Int J Gynecol Obstet 123:50–53. https://doi.org/10.1016/j.ijgo.2013.04.022
Persson M, Norman M, Hanson U (2009) Obstetric and perinatal outcomes in type 1 diabetic pregnancies. Diabetes Care 32:2005–2009. https://doi.org/10.2337/DC09-0656
Janney CA, Zhang D, Sowers M (1997) Lactation and weight retention. Am J Clin Nutr 66:1116–1124. https://doi.org/10.1093/ajcn/66.5.1116
Tørris C, Bjørnnes AK (2020) Duration of lactation and maternal risk of metabolic syndrome: a systematic review and meta-analysis. Nutrients 12:1–18. https://doi.org/10.3390/NU12092718
Dewey KG, Heinig MJ, Nommsen LA (1993) Maternal weight-loss patterns during prolonged lactation. Am J Clin Nutr 58:162–166. https://doi.org/10.1093/AJCN/58.2.162
Vinter CA, Jensen DM, Ovesen P et al (2014) Postpartum weight retention and breastfeeding among obese women from the randomized controlled lifestyle in pregnancy (LiP) trial. Acta Obstet Gynecol Scand 93:794–801. https://doi.org/10.1111/AOGS.12429
Ronnberg AK, Hanson U, Ostlund I, Nilsson K (2016) Effects on postpartum weight retention after antenatal lifestyle intervention – a secondary analysis of a randomized controlled trial. Acta Obstet Gynecol Scand 95:999–1007. https://doi.org/10.1111/AOGS.12910
Cyganek K, Hebda-Szydlo A, Skupien J et al (2013) Postpregnancy glycemic control and weight changes in type 1 diabetic women. Diabetes Care 36:1083–1087. https://doi.org/10.2337/DC12-1340
Ringholm L, Roskjær AB, Engberg S et al (2019) Breastfeeding at night is rarely followed by hypoglycaemia in women with type 1 diabetes using carbohydrate counting and flexible insulin therapy. Diabetologia 62:387–398
Herskin CW, Stage E, Barfred C et al (2015) Low prevalence of long-term breastfeeding among women with type 2 diabetes. J Matern Neonatal Med 29:1–6. https://doi.org/10.3109/14767058.2015.1092138
Endres LK, Straub H, McKinney C et al (2015) Postpartumweight retention risk factors and relationship to obesity at 1 year. Obstet Gynecol 125:144–152. https://doi.org/10.1097/AOG.0000000000000565
Iversen DS, Kesmodel US, Ovesen PG (2018) Associations between parity and maternal BMI in a population-based cohort study. Acta Obstet Gynecol Scand 97:694–700. https://doi.org/10.1111/AOGS.13321
Skajaa GO, Fuglsang J, Kampmann U, Ovesen G (2018) Parity increases insulin requirements in pregnant women with type 1 diabetes. J Clin Endocrinol Metab 103:2302–2308. https://doi.org/10.1210/jc.2018-00094
Hauff LE, Leonard SA, Rasmussen KM (2014) Associations of maternal obesity and psychosocial factors with breastfeeding intention, initiation, and duration. Am J Clin Nutr 99:524. https://doi.org/10.3945/AJCN.113.071191
Castillo H, Santos IS, Matijasevich A (2016) Maternal pre-pregnancy BMI, gestational weight gain and breastfeeding. Eur J Clin Nutr 70:431. https://doi.org/10.1038/EJCN.2015.232
Ketterl TG, Dundas NJ, Roncaioli SA et al (2018) Association of pre-pregnancy bmi and postpartum weight retention before second pregnancy, Washington State, 2003–2013. Matern Child Health J 22:1339–1344. https://doi.org/10.1007/S10995-018-2514-1
Acknowledgements
The authors would like to thank all the participants and nurse Dorte Svenstrup for collecting data from all the participants. The authors also thank Biostatistical Advisory Service at the Faculty of Health, Aarhus University, for helping with all statistical analysis.
Funding
U. Kampmann and PG. Ovesen have received research grants from the Novo Nordisk Foundation. GO. Skajaa and J. Fuglsang have no financial disclosures. The funding sources had no role in the study design, inclusion process, data analysis, or statistical considerations or in the writing of this report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Ulla Kampmann and author Per G. Ovesen have received research support from the Novo Nordisk Foundation. Author Gitte Ø. Skajaa and author Jens Fuglsang declare that they have no financial interests. The funding sources had no role in the study design, inclusion process, data analysis, or statistical considerations or in the writing of this paper.
Ethical Standard Statement
The study was conducted in accordance with the Helsinki Declaration and approved by the Regional Ethical Committee (No. 1-10-72-258-14).
Informed consent
Verbal and written consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Pregnancy and Diabetes, managed by Antonio Secchi and Marina Scavini.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Skajaa, G.Ø., Kampmann, U., Ovesen, P.G. et al. Breastfeeding and insulin requirements in women with Type 1 diabetes mellitus in the first year postpartum. Acta Diabetol 60, 899–906 (2023). https://doi.org/10.1007/s00592-023-02068-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02068-1