Abstract
Aim
Admission hyperglycemia and glucose variability were associated with mortality in critically ill patients, but data on trauma patients are to date scarce and heterogeneous.
Methods
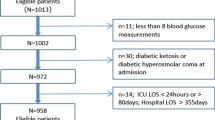
We assessed the prognostic role of ICU death of admission and peak glycemia and glucose variability (indicated by the standard deviation of mean glucose levels and the coefficient of variation of glucose) in 252 patients consecutively admitted for trauma in our ICU (January 1, 2016–December 31, 2018).
Results
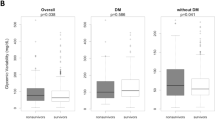
The in-ICU mortality rate was 17% (43/252). When compared to patients who died during ICU stay, survivors were younger (p = 0.001), more frequently males (p = 0.002), with a lower incidence of hypertension (p = 0.023). Higher values of SAPS II, SOFA and ISS were observed in nonsurvivors (p < 0.001, p < 0.001, p < 0.001, respectively). Survivors exhibited significantly lower values of admission glycemia (p = 0.001), peak glycemia (p = 0.002) and mean glucose values measured during the first 24 h since ICU admission (p = 0.001). Glucose variability was significantly higher in nonsurvivors, as indicated by higher values of SD and CV (p = 0.001 and p = 0.001, respectively). At multivariate regression analysis, admission glycemia (Model 1), peak glycemia (Model 2) and glucose variability (Model 3 and 4) were independent predictors for in-ICU mortality.
Conclusions
Our findings indicate that not only admission glycemia but also peak glycemia and glucose variability show a correlation with in-ICU mortality in trauma patients.
Similar content being viewed by others
References
Dungan KM, Braithwaite SS, Preiser JC (2009) Stress hyperglycaemia. Lancet 373:1798–1807
Gunst J, De Bruyn A, Van den Berghe G (2019) Glucose control in the ICU. Curr Opin Anaesthesiol 32(2):156–162
Olariu E, Pooley N, Danel A, Miret M, Preiser JC (2018) A systematic scoping review on the consequences of stress-related hyperglycaemia. PLoS ONE 13(4):e0194952
Hermanides J, Plummer MP, Finnis M, Deane AM, Coles JP, Menon DK (2018) Glycaemic control targets after traumatic brain injury: a systematic review and meta-analysis. Crit Care 22(1):11
Eslami S, Taherzadeh Z, Schultz MJ, Abu-Hanna A (2011) Glucose variability measures and their effect on mortality: a systematic review. Intensive Care Med 37(4):583–593
Meyfroidt G (2015) Blood glucose amplitude in critically ill patients. Minerva Anesthesiol 81(9):1010–1018
Bonizzoli M, Zagli G, Lazzeri C, Degl’Innocenti S, Gensini G, Peris A (2012) Early insulin resistance in severe trauma without head injury as outcome predictor? A prospective, monocentric pilot study. Scand J Trauma Resusc Emerg Med 20:69
Lazzeri C, Valente S, Chiostri M, Attanà P, Picariello C, Gensini GF (2012) Predictors for in-hospital peak glycemia in STEMI patients without previously known diabetes. Int J Cardiol 155(3):459–461
Lazzeri C, Valente S, Chiostri M, Attanà P, Picariello C, Gensini GF (2012) The prognostic role of in-hospital peak glycemia in stemi patients with and without diabetes. Acta Diabetol 49(5):379–386
Lazzeri C, Valente S, Chiostri M, Picariello C, Gensini GF (2010) In-hospital peak glycemia and prognosis in STEMI patients without previously known diabetes. Eur J Cardiovasc Prev Rehabil 17(4):419–423
Lazzeri C, Valente S, Chiostri M et al (2014) In-hospital peak glycemia in non-diabetic patients with heart failure complicating acute coronary syndrome. Int J Cardiol 176(1):260–262
Krinsley JS (2009) Glycemic variability and mortality in critically ill patients: the impact of diabetes. J Diabetes Sci Technol 3:1292–1301
Egi M, Bellomo R, Stachowski E, French CJ, Hart G (2006) Variability of blood glucose concentration and short-term mortality of critically ill patients. Anesthesiology 105:244–252
Lazzeri C, Valente S, Chiostri M, Attanà P, Gensini GF (2015) Early glucose variability in cardiogenic shock following acute myocardial infarction: a pilot study. Ther Adv Cardiovasc Dis. 9(4):127–132
Yendamuri S, Fulda GJ, Tinkoff GH (2003) Admission hyperglycemia as a prognostic indicator in trauma. J Trauma 55(1):33–38
Kreutziger J, Schlaepfer J, Wenzel V, Constantinescu MA (2009) The role of admission blood glucose in outcome prediction of surviving patients with multiple injuries. J Trauma 67(4):704–708
Laird AM, Miller PR, Kilgo PD, Meredith JW, Chang MC (2004) Relationship of early hyperglycemia to mortality in trauma patients. J Trauma 56(5):1058–1062
Kreutziger J, Schmid S, Umlauf N et al (2018) Association between blood glucose and cardiac rhythms during pre-hospital care of trauma patients—a retrospective analysis. Scand J Trauma Resusc Emerg Med 26(1):58
Winkelmann M, Butz AL, Clausen JD et al (2019) Admission blood glucose as a predictor of shock and mortality in multiply injured patients. SICOT J 5:17
Lazzeri C, Tarquini R, Giunta F, Gensini GF (2009) Glucose dysmetabolism and prognosis in critical illness. Intern Emerg Med 4(2):147–156
Preiser JC, Ichai C, Orban JC, Groeneveld AB (2014) Metabolic response to the stress of critical illness. Br J Anaesth 113(6):945–954
Shere-Wolfe RF, Galvagno SM Jr, Grissom TE (2012) Critical care considerations in the management of the trauma patient following initial resuscitation. Scand J Trauma Resusc Emerg Med 20:68
Eriksson EA, Christianson DA, Vanderkolk WE, Bonnell BW, Hoogeboom JE, Ott MM (2011) Tight blood glucose control in trauma patients: Who really benefits? J Emerg Trauma Shock 4:359–364
Collier B, Diaz J Jr, Forbes R et al (2005) The impact of a normoglycemic management protocol on clinical outcomes in the trauma intensive care unit. JPEN J Parenter Enteral Nutr 29:353–358
Ali NA, O’Brien JM Jr, Dungan K et al (2008) Glucose variability and mortality in patients with sepsis. Crit Care Med 36(8):2316–2321
Waeschle RM, Moerer O, Hilgers R, Herrmann P, Neumann P, Quintel M (2008) The impact of the severity of sepsis on the risk of hypoglycaemia and glycaemic variability. Crit Care 12(5):R129
Hirshberg E, Larsen G, Van Duker H (2008) Alterations in glucose homeostasis in the pediatric intensive care unit: hyperglycemia and glucose variability are associated with increased mortality and morbidity. Pediatr Crit Care Med 9(4):361–366
Dossett LA, Cao H, Mowery NT, Dortch MJ, Morris JM Jr, May AK (2008) Blood glucose variability is associated with mortality in the surgical intensive care unit. Am Surg 74(8):679–685
Funding
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
The study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Ethical approval
The Internal Review Board approved the study
Informed consent
Informed consent for study participation and data publication was obtained from patients or their family members
Additional information
Managed By: Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lazzeri, C., Bonizzoli, M., Cianchi, G. et al. The prognostic role of peak glycemia and glucose variability in trauma: a single-center investigation. Acta Diabetol 57, 931–935 (2020). https://doi.org/10.1007/s00592-020-01493-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-020-01493-w