Abstract
Purpose
Supracondylar humerus (SCH) fractures account for approximately 30% of injuries for those younger than 7 years of age (Cheng et al. in J Pediatr Orthop 19:344–350, 1999). Recent studies examining the association of patient age and SCH fracture outcomes have provided conflicting findings. The purpose of this study is to investigate SCH fracture outcomes in children at different ages of skeletal development.
Methods
Retrospective review of a Level I pediatric trauma center between 2010 and 2014 was conducted. 190 patients with SCH fractures, age < 14 years, fracture type Gartland III or IV (AO/OTA 13-M 3.1 III and IV) were included. Patients were sorted into age groups: < 2 years, 4–6 years, and > 8 years. Patients were treated with either a closed or open reduction with percutaneous fixation. Clinical outcomes including postoperative elbow range of motion, nerve palsy, compartment syndrome, infection, and cubitus varus were assessed.
Results
Patients in younger age groups were more likely to obtain postoperative full elbow flexion (< 2 years = 77%; 4–6 years = 66%; > 8 years = 43%) and full elbow extension (< 2 years = 96%; 4–6 years = 88%; > 8 years = 64%). Age was a significant predictor of nerve palsy on admission, mean operative time (< 2 years = 21.8 min; 4–6 years = 43.0 min; > 8 years = 80.7 min), and mean fluoroscopy time (< 2 years = 22.9 s; 4–6 years = 59.5 s; > 8 years = 171.9 s). There were no differences in rates of open reduction, compartment syndrome, pin tract infection, cubitus varus, or reoperation among groups.
Conclusion
Increasing age is associated with increased elbow stiffness after percutaneous fixation of Gartland Type III and Type IV SCH fractures. Older patients with SCH fractures may benefit from formal rehabilitation.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Supracondylar humerus (SCH) fractures are some of the most common injuries in the pediatric population. They account for up to 30% of all fractures in children younger than 7 years old and more than 10,000 emergency department visits annually [1, 2]. While the need for surgery can be controversial for some Gartland type II SCH fractures, most pediatric orthopedic surgeons agree that type III and IV fractures are treated with either closed or open reduction and percutaneous pinning [3]. Immediate short-term concerns include limb threatening complications such as compartment syndrome and disruption of blood supply to the distal upper extremity. At least 10% of type III SCH fractures present with signs of vascular compromise [4, 5]. Additionally, long-term complications such as cubitus varus and restricted elbow range of motion (ROM) can significantly impact function. SCH fractures occur most commonly in children between ages 2 and 7 but can happen in children of any age [2]. Few previous studies have examined the association between patient age and complication rate.
Relevant studies that have been published have provided conflicting findings. In a 2012 retrospective review of 1297 pediatric patients with operative SCH fractures, Fletcher et al. reported patients older than 8 years of age had higher rates of pin tract infection and postoperative stiffness than younger patients [6]. In 2018 Robertson et al. published a review of 31,167 isolated SCH fractures in the National Trauma Data Bank which found older age to be a risk factor for compartment syndrome (OR 1.1; 95% CI 1.0–1.2; p < 0.0092) [7]. Contrary to these findings, Mitchelson et al. found that age did not have an effect on complication rates in their retrospective review of 382 SCH fractures [8]. The purpose of this study is to further investigate the effect of age on outcomes of supracondylar humerus fractures.
Materials and methods
A retrospective review was conducted on patients with SCH fractures who were treated at a single level I pediatric trauma center from 2010 to 2014. Patients aged < 14 years with a Gartland type III or IV SCH fracture (AO/OTA 13-M 3.1 III and IV) [9] who underwent closed or open reduction and percutaneous pinning were included. Medical charts and radiographs were reviewed for demographic information, clinical symptoms, operative report, and complications. Data were collected on presence of a nerve palsy on admission, fracture type, open versus closed reduction, total operative time, fluoroscopy time, reoperation, range of motion at final follow-up, and complications including cubitus varus, compartment syndrome, and pin tract infection. Patients were categorized into age-based groups: < 2 years, 4–6 years, and > 8 years to create 3 distinct study groups and minimize type II error. Differences in characteristics and outcomes were compared across groups.
Statistical analysis
Statistical analysis was performed using STATA software (version 14.0.371; StataCorp, LLC). Descriptive statistics were used to outline demographic characteristics, complication rates, and incidence of reoperation. Univariate analysis was performed to compare complication rates, rates of reoperation, need for open versus closed reduction, total operative and fluoroscopy time, and rate of return of full elbow flexion and extension at final follow-up. Differences in demographics, operative time, and fluoroscopy were analyzed using analysis of variance, and complications were analyzed using chi-square tests. Significance was defined by a p value < 0.05, and all tests were two-tailed. Pairwise comparisons were also made using a Bonferroni adjusted significance level of 0.017.
Results
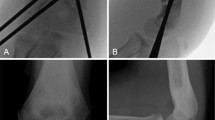
One-hundred and ninety patients with 190 SCH fractures met inclusion criteria (Fig. 1). Mean age was 5.8 ± 2.7 (range 0.2–13) years and mean follow-up 3.6 ± 4.7 (range 0.5–42) months. Fracture type was assigned based on the postoperative diagnosis of the operative report. Time-to-surgery was defined as the interval between the time of injury and the surgery start time. Demographics were similar among all three age groups as shown in Table 1. The population included 138 (73%) type III SCH fractures and 52 (27%) type IV fractures. There were 26 patients < 2 years old, 111 4–6 years old, and 53 > 8 years old. Duration of pinning and casting were slightly longer in the oldest compared with the middle age group (p < 0.004).
Clinical outcomes by age group are presented in Table 2. Age was a significant predictor of nerve palsy on admission. Patients were most likely to present with a nerve palsy in the middle age group and least likely in the youngest age group (< 2 years = 0%; 4–6 years = 25.2%; > 8 years = 20.8%; p = 0.006). Increased age was also associated with an increase in mean operative time (< 2 yo = 21.8 min; 4–6 yo = 43.0 min; > 8 yo = 80.7 min; p < 0.001) and mean fluoroscopy time (< 2 yo = 22.9 s; 4–6 yo = 59.5 s; > 8 yo = 171.9 s; p < 0.001). Elbow stiffness was also more likely to occur in older patients. Full elbow flexion was recorded at final follow-up in 20 (77%) patients < 2 years of age, 73 (66%) in the 4–6 year group, and 23 (43%) in the > 8 year group (p = 0.005). Full elbow extension was recorded at final follow-up in 25 (96%) patients in the < 2 year group, 98 (88%) in the 4–6 year group and 34 (64%) in the > 8 year group (p < 0.001). Multivariable analysis indicated that stiffness was more likely in older patients even after adjusting for length of follow-up.
Older patients were more likely to undergo open reduction, but this difference did not reach statistical significance (< 2 years = 0%; 4–6 years = 8.1%; > 8 years = 13.2%; p = 0.149). Age also did not correlate with the incidence of complications including compartment syndrome (p = 0.60), pin tract infection (p = 0.19), cubitus varus (p > 0.999), or reoperation (p = 0.87).
Discussion
This study identified increasing patient age as a predictor of elbow stiffness following operative fixation of SCH fractures. Our findings are consistent with those of Fletcher et al. who reported increased postoperative stiffness in older patients with SCH fractures [6]. The authors also found that older patients were much more likely to have experienced higher energy mechanisms of injury such as falls from height, motor vehicle accidents, or falls from moving objects such as bicycles. This, combined with a higher incidence of open fractures in their study, suggests that older patients may suffer more complications, such as limited postoperative ROM, because they experience worse injuries. These findings may account for some of the differences noted here since older patients may have higher mechanisms of injury and therefore likely have more soft tissue injury [10,11,12]. Correspondingly, we found that duration of casting and duration of pinning were slightly longer in the older age group compared to the middle age group. At our institution it is standard practice for patients to be casted for 3–4 weeks and at that time have their pins pulled with no additional immobilization. Therefore, this difference was not of clinical significance given that all age groups had duration of casting and pinning within the standard practice timeframe. Furthermore, it is important to note that we observed no difference in the incidence of type IV injuries in each age group (30.8% vs. 21.6% vs. 37.7%, p = 0.073).
Morrey et al. defined functional ROM of the elbow for adults to be 30°–130° [13]. Eleven patients in our study had a ROM at final follow-up that fell outside of this functional range. Most of these patients, 72.7% (8/11), were in the oldest age group (> 8 years old). The remainder were from the middle age group (4–6 years old). No patients in the youngest age group in this study had functionally limiting elbow ROM. According to Sardelli et al., modern functional ROM of the elbow may actually be even greater, considering the extensive use of cell phones and computers that Morrey et al. did not include as activities of daily living when they published it in 1981 [14].
Some studies suggest that stiffness following operative fixation of SCH fractures may not be lasting. Zionts et al. described the evolution of return of elbow range of motion following closed reduction percutaneous pinning (CRPP) for SCH fractures [15]. The pattern described by the authors began with sudden but incomplete return of ROM followed by gradual return to full ROM. In their study elbow ROM was 72% of that of the contralateral elbow at 6 weeks postoperatively, 86% at 12 weeks, 94% at 26 weeks, and 98% at 1 year. They also found that improvements in ROM could happen up to 1 year postoperatively. Spencer et al. corroborated these findings of large initial improvements in elbow ROM and later gradual improvements [16]. Our mean overall follow-up of 3.2 months may not have been long enough to capture all eventual improvements in ROM. However, we demonstrate that up to at least 12 weeks postoperatively older patients with SCH fractures may be at greater risk of debilitating elbow stiffness when compared to other age groups.
Although these studies may dispel concerns over permanent elbow stiffness, further investigation is needed to determine the role of postoperative therapy in restoring full elbow ROM [10]. Schmale et al. found no impact of physical therapy on elbow ROM at any time point up to 15 weeks postoperatively, however this study focused solely on closed treatment of SCH fractures [17]. These findings argue against having a low threshold for initiating therapy in older patients to combat anticipated stiffness. While our study did not follow patients out long-term, our findings suggest that older patients might benefit from an earlier referral for physical therapy when compared with younger patients.
Fletcher et al. reported that their older patient cohort was four times more likely to be referred to occupational therapy, which carries significant costs. Even among those with insurance, there is a large variation in the amount of out-of-pocket costs associated with occupational therapy [6]. Co-pays, missed work, and transportation for physical therapy can also be burdensome [18]. In their 2017 analysis of both the direct and indirect costs of treating distal radius fractures, Swart et al. found occupational therapy to be the fifth highest cost associated with operative treatment, after implants and ahead of recovery room, inpatient, and emergency department costs [19]. High costs of therapy can decrease compliance with regimens and increase disability [18].
Additionally, there are financial costs associated with a long period of elbow stiffness that must be considered. The psychological and societal effects of the cosmetic appearance of a stiff elbow must also be considered. Although postoperative therapy may not produce a long-term difference in elbow ROM, it presents the potential to reduce these psychosocial stresses. Further study is needed to assess the utility of postoperative therapy by age.
We analyzed differences in operative time and fluoroscopy time, specifically using fluoroscopy time as a surrogate for difficulty of reduction [20]. Age was a significant predictor of mean operative time (< 2 yo = 21.8 min; 4–6 yo = 43.0 min; > 8 yo = 80.7 min; p < 0.001) and mean fluoroscopy time (< 2 yo = 22.9 s; 4–6 yo = 59.5 s; > 8 yo = 171.9 s; p < 0.001) (Table 2). Older patients may have fractures that are more difficult to reduce because they have higher energy mechanisms of injury. This may cause increased displacement, soft tissue injury, and swelling. Increasing total operative and fluoroscopic time with age is important to note for the purposes of managing the expectations of the operative team, anesthesiologist, and patient’s family perioperatively.
Overall, our findings can be applied to create a better framework for informing patients and parents on what to expect both intraoperatively and postoperatively following supracondylar humerus fractures.
References
Cheng JC, Ng BK, Ying SY, Lam PK (1999) A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop 19(3):344–350
Holt JB, Glass NA, Shah AS (2018) Understanding the epidemiology of pediatric supracondylar humeral fractures in the United States: identifying opportunities for intervention. J Pediatr Orthop 38(5):e245–e251. https://doi.org/10.1097/bpo.0000000000001154
Omid R, Choi PD, Skaggs DL (2008) Supracondylar humeral fractures in children. J Bone Jt Surg Am 90(5):1121–1132. https://doi.org/10.2106/jbjs.g.01354
Pirone AM, Graham HK, Krajbich JI (1988) Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Jt Surg Am 70(5):641–650
Shaw BA, Kasser JR, Emans JB, Rand FF (1990) Management of vascular injuries in displaced supracondylar humerus fractures without arteriography. J Orthop Trauma 4(1):25–29
Fletcher ND, Schiller JR, Garg S et al (2012) Increased severity of type III supracondylar humerus fractures in the preteen population. J Pediatr Orthop 32(6):567–572. https://doi.org/10.1097/BPO.0b013e31824b542d
Robertson AK, Snow E, Browne TS, Brownell S, Inneh I, Hill JF (2018) Who gets compartment syndrome?: A retrospective analysis of the national and local incidence of compartment syndrome in patients with supracondylar humerus fractures. J Pediatr Orthop 38(5):e252–e256. https://doi.org/10.1097/bpo.0000000000001144
Mitchelson AJ, Illingworth KD, Robinson BS et al (2013) Patient demographics and risk factors in pediatric distal humeral supracondylar fractures. Orthopedics 36(6):e700–e706. https://doi.org/10.3928/01477447-20130523-12
AO pediatric comprehensive classification of long bone fractures (PCCF). J Orthop Trauma 32(Suppl 1):S117−S140 https://doi.org/10.1097/BOT.0000000000001065
Keppler P, Salem K, Schwarting B, Kinzl L (2005) The effectiveness of physiotherapy after operative treatment of supracondylar humeral fractures in children. J Pediatr Orthop 25(3):314–316
Henrikson B (1966) Supracondylar fracture of the humerus in children. A late review of end-results with special reference to the cause of deformity, disability and complications. Acta Chir Scand Suppl 369:1–72
Nacht JL, Ecker ML, Chung SM, Lotke PA, Das M (1983) Supracondylar fractures of the humerus in children treated by closed reduction and percutaneous pinning. Clin Orthop Relat Res 177:203–209
Morrey BF, Askew LJ, Chao EY (1981) A biomechanical study of normal functional elbow motion. J Bone Jt Surg Am 63(6):872–877
Sardelli M, Tashjian RZ, MacWilliams BA (2011) Functional elbow range of motion for contemporary tasks. J Bone Jt Surg Am 93(5):471–477. https://doi.org/10.2106/jbjs.i.01633
Zionts LE, Woodson CJ, Manjra N, Zalavras C (2009) Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clin Orthop Relat Res 467(8):2007–2010. https://doi.org/10.1007/s11999-009-0724-y
Spencer HT, Wong M, Fong YJ, Penman A, Silva M (2010) Prospective longitudinal evaluation of elbow motion following pediatric supracondylar humeral fractures. J Bone Jt Surg Am 92(4):904–910. https://doi.org/10.2106/jbjs.i.00736
Schmale GA, Mazor S, Mercer LD, Bompadre V (2014) Lack of benefit of physical therapy on function following supracondylar humeral fracture: a randomized controlled trial. J Bone Jt Surg Am 96(11):944–950. https://doi.org/10.2106/jbjs.l.01696
Pergolotti M, Lavery J, Reeve BB, Dusetzina SB (2018) Therapy caps and variation in cost of outpatient occupational therapy by provider, insurance status, and geographic region. Am J Occup Ther 72(2):7202205050p1-7202205050p9. https://doi.org/10.5014/ajot.2018.023796
Swart E, Tulipan J, Rosenwasser MP (2017) How should the treatment costs of distal radius fractures be measured? Am J orthop 46(1):E54-e59
Prabhakar P, Ho CA (2019) Delaying surgery in type III supracondylar humerus fractures does not lead to longer surgical times or more difficult reduction. J Orthop Trauma 33(8):e285–e290. https://doi.org/10.1097/bot.0000000000001491
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium.
Author information
Authors and Affiliations
Contributions
Conceptualization contributed by Erin Meisel, Rachel Y. Goldstein; methodology contributed by Mary Kate Erdman, Erin Meisel, Rachel Y. Goldstein; data collection contributed by Kavish Gupta, Ali Siddiqui, Mathew Schur; manuscript preparation contributed by Kavish Gupta, Mary Kate Erdman; manuscript review contributed by Kavish Gupta, Mary Kate Erdman, Ali Siddiqui, Mathew Schur, Erin Meisel, Rachel Y. Goldstein.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study has been carried out with approval from the Institutional Review Board at Children’s Hospital Los Angeles. This study abides by the ethical principles established in the WMA Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gupta, K., Erdman, M.K., Siddiqui, A. et al. Age is a predictor of elbow stiffness after type III or IV supracondylar humerus fractures. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-04031-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-04031-4