Abstract
Purpose
Time to surgery from admission is one of the few variables known to influence outcome after a hip fracture. We reviewed our hip fracture database to determine correlation between delays to surgery and mortality in our elderly hip fracture population.
Methods
Data on all hip fracture patients admitted to a large district hospital were prospectively collected between January 1989 and August 2021. Time of the injury, time of admission and time of surgery were recorded. Patients over 60 years old with a hip fracture requiring operative management were included. Patients with pathological fractures, those managed conservatively, and patients delayed for medical reasons were excluded. Surgical timing categories were divided into; under 12 h, 12–24 h, 24–72 h and over 72 h.
Results
Time from admission to surgery was recorded for 10,659 patients, of these time of fall was available for 10,346 patients. Mean age was 82.2 years (sd 8.39) for the cohort and 30 day mortality was 6.20%.
Odds of 30-day mortality was 1.43 (CI 1.057–1.988, p = 0.025) for delay to surgery from admission of over 12 h compared to under 12 h. Odds ratios for 30-day mortality were not significant at any other time threshold. The odds of 30-day mortality for delay to surgery from time of fall were 1.550 (CI 1.026–2.459, p = 0.048) at the 12 h threshold.
Conclusion
This is the largest prospective study to date in elderly patients with hip fractures demonstrating a statistically significant increase in 30-day mortality with a delay to surgery over 12 h.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over 70,000 patients are admitted to hospitals in England and Wales with hip fractures each year[1]. These injuries lead to high rates of morbidity and mortality amongst the elderly with rates of 30-day mortality of 6.6% prior to the 2020 covid-19 pandemic [1]. Many different factors have been proposed to impact on mortality, such as age and co-morbidities; however, the time delay to surgery remains one of the few variables that can be altered.
Various studies have reported differing time thresholds for significant improvements in mortality[2,3,4,5,6,7,8,9,10,11,12,13,14,15], with some finding no significant difference [16,17,18,19,20,21]. These studies use varying time cutoffs for analysing delay and mortality, and negative results were predominantly from smaller cohorts.
Whilst current UK guidelines recommend intervention within 36 h [22] evidence from our local cohort has previously shown benefit from operating earlier [23].
The aim of this study was to determine, using our final dataset, whether reducing the delay from admission to surgery continues to improve survivorship in our elderly hip fracture population and determine whether reducing delay from fall to surgery confers a similar survival benefit.
Patients and methods
Data on all hip fracture patients admitted to a large district hospital between January 1989 to August 2021 were prospectively collected on a hip fracture database using a standardised proforma. Data collected included: age, gender, place of residence prior to admission, American Society of Anaesthesiologist (ASA) score, mini mental test score (MTS) [24], the time of the injury, time of admission and the time of surgery. Mobility was also scored prospectively at the time of admission using a scale from 0 to 9 points as shown in Table 1.
Patients were included in this study if they were over 60 years old and had sustained a hip fracture requiring operative management. Those patients with pathological fractures, those managed conservatively and patients who were delayed for medical reasons were excluded. Patients were then divided into time categories where time from admission to surgery was under 12 h, 12–24 h, 24–72 h and over 72 h. Separate analysis for time of fall to surgery was performed on the subgroup where time of injury was also available. All patients were followed up with telephone consultation at 12 months and survival was confirmed with either the patient or next of kin. Where patients were not reachable, mortality was confirmed via hospital databases or recorded as missing data.
Count data were summarised as absolute numbers and proportions, continuous data as means and standard deviations. Patient characteristics grouped by time to surgery were compared using Analysis of Variance for the continuous variables and Pearson chi-squared test for the categorical variables. The threshold for statistical significance was set at p = 0.05. Multivariate binary logistic regression analysis was performed looking at the odds of 30-day mortality before each delay to surgery threshold versus delay beyond this threshold. All variables in the multivariable logistic regression model were entered without exclusions for collinearity [26]. Data were analysed using R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
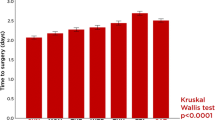
A total of 12,223 patients were admitted with hip fractures during the study period. Data were available for 10,659 patients after applying exclusion criteria, of which time of fall was available for 10,346 patients (Fig. 1). Mean age for the cohort was 82.2 years (sd 8.39) and 8,023 (75.3%) were female. Mean time from admission to surgery was 27.0 h (sd 28.3) and mean ASA grade 2.71 (sd 0.70). Mean 30-day mortality was 6.2% for the cohort, ranging from 4.8% for those operated in under 12 h from admission to 8.6% for those operated beyond 72 h (Table 2).
Odds of 30-day mortality was 1.43 (CI 1.057–1.988, p = 0.025) for delay to surgery from admission of over 12 h compared to under 12 h (Table 3). Odd ratios for 30-day mortality were not significant at any other time threshold. Age, gender, ASA, MTS, mobility score and fracture type remained significant on multivariate analysis (Fig. 2).
Similar demographics were demonstrated for the subgroup where time of fall was available (Table 4). The same variables remained significant on multivariate analysis (Fig. 3). The odds of 30-day mortality for delay to surgery from time of fall were 1.550 (CI 1.026–2.459, p = 0.048) at the 12 h threshold (Table 5). This was also not significant at any other time threshold (Table 6).
Discussion
National mortality rates for elderly patients with hip fractures have varied considerably in recent years [1], partly as a result of widespread covid-19 infection[27,28,29,30] and changes in health service provision during the pandemic. Mortality at our hospital has shown similar yearly variations with a broadly decreasing trend prior to the pandemic. Many factors have influenced this including improvements in peri-operative care and enhanced rehabilitation post-operatively; however, timing of surgery remains a key modifiable factor. This study demonstrates clear benefit from prompt surgical intervention in elderly patients with hip fractures, ideally within 12 h and benefits from a large cohort, minimal loss to follow-up and prospectively collected data. In addition to this, patients delayed for medical reasons were excluded and patient variables known to be correlated with mortality were accounted for with multivariate analysis.
Other studies have suggested differing time thresholds for intervention to reduce mortality; however, conflicting results from these can be explained by small cohorts, heterogenous time categories or incomplete analysis of confounders. More recently, the Hip ATTACK study randomised 2970 patients to early vs standard care; the largest randomised control trial on surgical timing to date and found no difference in mortality rates at 90 days [18].
Best practice tariffs are paid to trusts where surgery is performed within 36 h and NICE guidelines currently recommend surgery on the day of or day after admission. This was based on “pragmatic, organisational and human considerations” after their 2011 evidence review found no specific interval threshold below which reducing delays had no benefit [22]. Outcomes for 30-day mortality in their review were based on evidence from three studies [2, 3, 21].
We also demonstrated similar rates of 30-day mortality when assessed by time of fall rather than admission. Patients with undiagnosed hip fractures may well cope at home for a period of time, suggesting higher functional capacity or minimal initial displacement of fracture, only presenting when their condition deteriorates. Our data suggest patients who are otherwise well should be prioritised by time of admission and the time of fall should not routinely affect decision making. It is also possible that patients present late with long lies due to not being found following a fall and then deteriorate as a result. These would likely have been delayed for medical reasons and therefore excluded from this study or otherwise adjusted for with higher ASA grade.
Covid-19 infection will have also affected mortality rates, particularly during peak infection periods with early variants. Test results for Covid-19 were not included within this study but again these patients will most likely be adjusted for within ASA grade or, if unwell, excluded for delay due to medical reasons.
Whilst our data show the lowest mortality in those operated on within 12 h of admission, we acknowledge that this is dependent on fortuitous arrival time and sufficient theatre capacity. Theatres are not typically staffed to accommodate hip fracture patients overnight for pragmatic reasons, and evidence is conflicting on the impact of out of hours operating on mortality [31,32,33,34]. Patients of similar clinical urgency may be prioritised, and it is unlikely the majority of patients could be treated within this timeframe at most hospitals.
Timing of surgery may also have been affected by patients’ clinical condition on presentation or co-morbidities. According to hospital policy at the site where data were collected, surgeries were conducted in the order of presentation to the Emergency Department (ED), unless a patient's medical condition necessitates a delay for optimisation. Patients were excluded from our study where medical delay was documented, reducing large variations in timing due to medical condition. However, we cannot rule out the possibility of insufficient documentation or minor changes, such as the order of patients within an operating list, that could affect the data.
Despite these limitations, our large cohort and detailed accounting for confounding factors show optimising timing of care is crucial to minimising early death as a result of hip fracture.
Future directions
Our ageing population, whilst driving rising hip fracture incidence, also increases the burden of fragility fractures of the hip. Understanding the impact of delays on these conditions is crucial to guide how best to allocate resources. Our single centre study benefits from consistent data collection and similar peri-operative care across the cohort, but expanding this to a multi-centre study would enhance understanding of this topic. Such expansion would enable a shorter study timeline and diminish the influence of temporal shifts in health policy and practice. Additionally, exploring variations in clinical practice, including differences in clinical skill, departmental resources, and rehabilitation quality across multiple sites, could unveil novel insights. National registries, routine data linkage and artificial intelligence have shown potential to address some of the logistical challenges of collecting large datasets. It is our hope that future studies could benefit from these technological advances in data management to improve the evidence base informing health policy and clinical practice.
Conclusion
Delay to surgery of over 12 h from admission is associated with a statistically significant increase in 30-day mortality in elderly patients with hip fractures.
References
Royal College of Physicians (2021) Improving understanding—the national hip fracture database report on 2021, 2022:1–21
Bottle A, Aylin P (2006) Mortality associated with delay in operation after hip fracture: observational study. Br Med J 332:947–950. https://doi.org/10.1136/bmj.38790.468519.55
Weller I, Wai EK, Jaglal S, Kreder HJ (2005) The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Jt Surg Ser B 87:361–366. https://doi.org/10.1302/0301-620X.87B3.15300
Siegmeth AW, Gurusamy K, Parker MJ (2005) Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Jt Surg Ser B 87:1123–1126. https://doi.org/10.1302/0301-620X.87B8.16357
Castellanos SC, Marco FL, Domínguez EB, Gálvez EMV, Pérez BM (2022) Does delaying surgery for “healthy” hip fracture patients have increased complications and mortality? Injury 53:3209–3213. https://doi.org/10.1016/j.injury.2022.06.035
Rozenfeld M, Bodas M, Shani M, Radomislensky I, Murad H, Comaneshter D et al (2021) National study: most elderly patients benefit from earlier hip fracture surgery despite co-morbidity. Injury 52:905–909. https://doi.org/10.1016/j.injury.2020.10.060
Nilsen SM, Asheim A, Carlsen F, Anthun KS, Johnsen LG, Vatten LJ et al (2021) High volumes of recent surgical admissions, time to surgery, and 60-day mortality a cohort study of 60,000 Norwegian hip fracture patients. Bone Jt J 103:264–270. https://doi.org/10.1302/0301-620X.103B2.BJJ-2020-1581.R1
Öztürk B, Johnsen SP, Röck ND, Pedersen L, Pedersen AB (2019) Impact of comorbidity on the association between surgery delay and mortality in hip fracture patients: a Danish nationwide cohort study. Injury 50:424–431. https://doi.org/10.1016/j.injury.2018.12.032
Leer-Salvesen S, Engesæter LB, Dybvik E, Furnes O, Kristensen TB, Gjertsen JE (2019) Does time from fracture to surgery affect mortality and intraoperative medical complications for hip fracture patients? An observational study of 73 557 patients reported to the Norwegian hip fracture register. Bone Jt J 101:1129–1137. https://doi.org/10.1302/0301-620X.101B9.BJJ-2019-0295.R1
Beaupre LA, Khong H, Smith C, Kang S, Evens L, Jaiswal PK et al (2019) The impact of time to surgery after hip fracture on mortality at 30- and 90-days: does a single benchmark apply to all? Injury 50:950–955. https://doi.org/10.1016/j.injury.2019.03.031
Bokshan SL, Marcaccio SE, Blood TD, Hayda RA (2018) Factors influencing survival following hip fracture among octogenarians and nonagenarians in the United States. Injury 49:685–690. https://doi.org/10.1016/j.injury.2018.02.004
Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens AB et al (2017) Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA J Am Med Assoc 318:1994–2003. https://doi.org/10.1001/jama.2017.17606
Morrissey N, Iliopoulos E, Osmani AW, Newman K (2017) Neck of femur fractures in the elderly: does every hour to surgery count? Injury 48:1155–1158. https://doi.org/10.1016/j.injury.2017.03.007
Nyholm AM, Gromov K, Palm H, Brix M, Kallemose T, Troelsen A (2015) Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture. J Bone Joint Surg 97:1333–1339. https://doi.org/10.2106/jbjs.o.00029
Lizaur-Utrilla A, Martinez-Mendez D, Collados-Maestre I, Miralles-Muñoz FA, Marco-Gomez L, Lopez-Prats FA (2016) Early surgery within 2 days for hip fracture is not reliable as healthcare quality indicator. Injury 47:1530–1535. https://doi.org/10.1016/j.injury.2016.04.040
van Rijckevorsel VAJIM, de Jong L, Verhofstad MHJ, Roukema GR, van Beek F, van Buijtenen JM et al (2022) Influence of time to surgery on clinical outcomes in elderly hip fracture patients an assessment of surgical postponement due to non-medical reasons. Bone Jt J 104:1369–1378. https://doi.org/10.1302/0301-620X.104B12.BJJ-2022-0172.R2
Schoeneberg C, Aigner R, Pass B, Volland R, Eschbach D, Peiris SE et al (2021) Effect of time-to-surgery on in-house mortality during orthogeriatric treatment following hip fracture: a retrospective analysis of prospectively collected data from 16,236 patients of the alters trauma register DGU®. Injury 52:554–561. https://doi.org/10.1016/j.injury.2020.09.007
Borges FK, Bhandari M, Guerra-Farfan E, Patel A, Sigamani A, Umer M et al (2020) Accelerated surgery versus standard care in hip fracture (hip attack): an international, randomised, controlled trial. Lancet 395:698–708. https://doi.org/10.1016/S0140-6736(20)30058-1
Sasabuchi Y, Matsui H, Lefor AK, Fushimi K, Yasunaga H (2018) Timing of surgery for hip fractures in the elderly: a retrospective cohort study. Injury 49:1848–1854. https://doi.org/10.1016/j.injury.2018.07.026
Kempenaers K, Van Calster B, Vandoren C, Sermon A, Metsemakers WJ, Vanderschot P et al (2018) Are the current guidelines for surgical delay in hip fractures too rigid? A single center assessment of mortality and economics. Injury 49:1169–1175. https://doi.org/10.1016/j.injury.2018.03.032
Al-Ani AN, Samuelsson B, Tidermark J, Norling Å, Ekström W, Cederholm T et al (2008) Early operation on patients with a hip fracture improved the ability to return to independent living: a prospective study of 850 patients. J Bone Jt Surg 90:1436–1442. https://doi.org/10.2106/JBJS.G.00890
National Clinical Guideline Centre (2011) CG124: the management of hip fracture in adults produced by the national clinical guideline centre. Health Technol Assess (Rockv), pp 68–81
Bretherton CP, Parker MJ (2015) Early surgery for patients with a fracture of the hip decreases 30-day mortality. Bone Jt J 97:104–108. https://doi.org/10.1302/0301-620x.97b1.35041
Qureshi KN, Hodkinson HM (1974) Evaluation of a ten-question mental test in the institutionalized elderly. Age Ageing. https://doi.org/10.1093/ageing/3.3.152
Parker MJ, Palmer CR (1993) A new mobility score for predicting mortality after hip fracture. J Bone Jt Surg Ser B 75:797–798. https://doi.org/10.1302/0301-620x.75b5.8376443
Heinze G, Dunkler D (2017) Five myths about variable selection. Transpl Int 30:6–10. https://doi.org/10.1111/tri.12895
Isla A, Landy D, Teasdall R, Mittwede P, Albano A, Tornetta P et al (2022) Postoperative mortality in the COVID-positive hip fracture patient, a systematic review and meta-analysis. Eur J Orthop Surg Traumatol 33:927–935. https://doi.org/10.1007/s00590-022-03228-9
Levitt EB, Patch DA, Mabry S, Terrero A, Jaeger B, Haendel MA et al (2022) Association between COVID-19 and mortality in hip fracture surgery in the national COVID cohort collaborative (N3C): a retrospective cohort study. JAAOS Global Res Rev. https://doi.org/10.5435/JAAOSGlobal-D-21-00282
Holleyman RJ, Khan SK, Charlett A, Inman DS, Johansen A, Brown C et al (2022) The impact of COVID-19 on mortality after hip fracture. Bone Joint J 104:1156–1167. https://doi.org/10.1302/0301-620X.104B10.BJJ-2022-0082.R1
Narang A, Chan G, Aframian A, Ali Z, Carr A, Goodier H et al (2021) Thirty-day mortality following surgical management of hip fractures during the COVID-19 pandemic: findings from a prospective multi-centre UK study. Int Orthop 45:23–31. https://doi.org/10.1007/s00264-020-04739-y
Kim RG, An VVG, Petchell JF (2021) Hip fracture surgery performed out-of-hours–a systematic review and meta-analysis. Injury 52:664–670. https://doi.org/10.1016/j.injury.2021.02.049
Pincus D, Desai SJ, Wasserstein D, Ravi B, Paterson JM, Henry P et al (2017) Outcomes of after-hours hip fracture surgery. J Bone Jt Surg Am 99:914–922. https://doi.org/10.2106/JBJS.16.00788
Petersen JD, Siersma VD, Wehberg S, Nielsen CT, Viberg B, Waldorff FB (2020) Clinical management of hip fractures in elderly patients with dementia and postoperative 30-day mortality: a population-based cohort study. Brain Behav 10:1–10. https://doi.org/10.1002/brb3.1823
Forssten MP, Mohammad Ismail A, Borg T, Cao Y, Wretenberg P, Bass GA et al (2022) The consequences of out-of-hours hip fracture surgery: insights from a retrospective nationwide study. Eur J Trauma Emerg Surg 48:709–719. https://doi.org/10.1007/s00068-021-01804-y
Author information
Authors and Affiliations
Contributions
Madeline Warren was contributed to data curation, writing—original draft, writing—review and editing, visualisation, project administration. Chris Bretherton was contributed to methodology, software, formal analysis, writing—review and editing, visualisation. Martyn Parker was contributed to conceptualization, methodology, investigation, writing—review and editing, supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All human data were collected as part of an ongoing audit database for all hip fracture patients admitted to our institution and aggregated anonymously for the purposes of this study. There was no direct involvement of human or animal subjects, and formal ethical approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Warren, M., Bretherton, C. & Parker, M. Delay to surgery beyond 12 hours is associated with increased hip fracture mortality. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-03997-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-03997-5