Abstract
Background
Minimally invasive percutaneous screw fixation for pelvic ring and acetabular fractures has become increasingly popular due to its numerous benefits. However, the precise placement of the screw remains a critical challenge, necessitating a modification of the current techniques. This paper introduces a refined technique employing a modified guidewire to enhance the precision and efficiency of percutaneous fixation in pelvic and acetabular fractures.
Methods
This study details the surgical techniques implemented for correcting guidewire misdirection in percutaneous screw fixation and includes a retrospective analysis of patients treated with this modified approach over a three-year period.
Results
In this study, 25 patients with pelvic ring and acetabular fractures underwent percutaneous screw fixation. The cohort, predominantly male (23 out of 25), had an average age of 38 years. The majority of injuries were due to traffic accidents (18 out of 25). Types of injuries included pelvic ring (6 cases), acetabular fractures (8 cases), and combined injuries (11 cases). Various screw types, including antegrade and retrograde anterior column screws, retrograde posterior column screws, and lateral compression screws, were used, tailored to each case. Over an average follow-up of 18 months, there were no additional procedures or complications, such as neurovascular injury or hardware failure, indicating successful outcomes in all cases.
Conclusions
This study introduces a simple yet effective method to address guidewire misdirection during percutaneous fixation for pelvic and acetabular fractures, offering enhanced precision and potentially better patient outcomes. Further research with a larger patient cohort is required for a more comprehensive understanding of its efficacy compared to traditional methods.
Level of evidence
IV. Therapeutic Study (Surgical technique and Cases-series).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Minimally invasive percutaneous screw fixation represents a critical advancement in orthopedic surgery for managing pelvic ring and acetabular fractures, offering significant advantages over traditional approaches [1]. This method, gaining prominence since its introduction by Routt et al. [2], provides several advantages over traditional open reduction and internal fixation, such as less soft-tissue trauma, reduced intraoperative blood loss, lower infection risks, early pain relief, and the possibility of early weight-bearing ambulation [3, 4].
Despite its benefits, including lessened soft-tissue damage and expedited postoperative recovery, the technique demands high precision due to the complex anatomy of the pelvis and proximity to critical neurovascular structures [5]. Achieving success with percutaneous interventions requires not only an intimate knowledge of pelvic anatomy and skill in radiographic imaging but also the ability to execute screw placement with extreme accuracy [4, 6, 7]. Elmhiregh et al. [8] demonstrated the critical role of careful radiographic assessment in avoiding intra-articular screw placement during acetabular surgery, a recognized complication with significant clinical repercussions. The authors also emphasized the efficacy of utilizing specific radiographic views for the detection of potential joint space violations, thereby underlining the importance of precise imaging in both surgical planning and postoperative evaluations [8]. While the literature provides extensive guidance on the paths and radiographic views necessary for correct screw placement, the task remains highly technical. The narrow osseous corridors challenge even the most skilled surgeons, often necessitating repeated attempts and trajectory adjustments to navigate the guidewire safely [9, 10].
This paper introduces a technique refinement designed to mitigate the challenges of guidewire misdirection. The focus is not only on the experiential reportage, but also on the significant findings derived from employing this technique. We detail how this method minimizes the need for multiple guidewire adjustments, thereby enhancing procedural precision and potentially reducing operative time and patient exposure to radiation. These improvements could have a substantial impact on patient outcomes and the standard of care in the management of pelvic and acetabular fractures.
Our objective is to share a practical solution that addresses a critical technical hurdle in percutaneous fixation, offering a path toward safer and more efficient surgical interventions.
Methods
A retrospective study was conducted on patients treated with percutaneous screw fixation for pelvic ring and acetabular fractures using a modified guidewire technique between August 2020 and August 2023 at a Level I trauma center. This study received approval from the institutional review board of our institution. The surgical procedures were consistently carried out by the same team of highly skilled surgeons. The classification of the pelvic ring injuries was done following the system proposed by Young and his team [9], while the Letournel and Judet system was employed for the classification of acetabular fractures [10].
Surgical technique
Preoperative considerations
The initial and critical step of this technique involves a thorough review of preoperative imaging. For pelvic ring injuries, our protocol includes a standardized imaging approach, routinely performed in all cases. This approach includes obtaining conventional anteroposterior (AP), inlet, and outlet radiographs of the pelvis. Additionally, iliac oblique and obturator oblique radiographs are obtained for detailed preoperative planning in cases of acetabular fractures. Furthermore, each patient undergoes meticulous computed tomography (CT) scanning with 2-mm slices. This comprehensive imaging is essential for understanding the complete extent of the injury, including fracture location, orientation, displacement patterns, comminution, anatomical variations, and available space for screw placement. These imaging modalities serve as crucial prerequisites for the successful application of the modified guidewire technique presented in this study.
Setup considerations
Patients with pelvic ring and acetabular fractures are positioned supine on a radiolucent table. The arms are abducted on an arm-board to avoid any interference with the C-arm during the inlet view. 2D fluoroscopy using a C-arm is utilized to confirm adequate reduction and monitor the safety and accuracy of the initial guide wire passage. Prior to the surgical procedure, the abdomen and the injured lower extremity are prepped and draped to ensure a sterile field. For interventions involving retrograde posterior column screw placement, we ensure that there is adequate access to the distal aspect of the ischial tuberosity and that the hip can be fully flexed to 90° and abducted without interference.
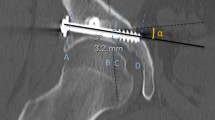
Guidewire insertion
This technique begins with the standard skin preparation and draping, followed by fluoroscopically identifying the optimal entry point. A 1-cm skin incision is made to expose the entry site, and then a non-threaded 3.5 mm guidewire is used to establish the initial trajectory under fluoroscopic guidance. The sharp end of the guidewire is manually bent, approximately 1 cm from its tip, at an angle of about 20–30° using pliers (Fig. 1). The guidewire is then gently tapped into the bone from the entry point using a hammer. In case of misdirection of the intraosseous trajectory, the guidewire is gently withdrawn and then rotated under biplanar fluoroscopic guidance until the bent tip is oriented in the intended correction direction. A T-handle is utilized for guidewire rotation. Instead of power tools, a mallet is used to delicately insert and advance the guidewire within the bone corridor to ensure superior control without cortical violation. Upon reaching the exit point site with the guidewire, fluoroscopic images are performed to validate the safety of the osseous corridor. If the confirmatory image meets satisfaction, a 4.5-mm cannulated drill is placed over the wire and advanced into the osseous fixation pathway. The screw length is determined using a similar length straight guidewire positioned alongside the modified guidewire at the entry point, with measurements taken extraosseously using a subtraction technique. Once the screw length is determined, a 6.5-mm cannulated screw is used for acetabular column fixation and properly seated with fluoroscopic verification. (Fig. 2). The guidewire is then removed and retrieved through the same skin incision.
Sequence of intraoperative fluoroscopic pelvic iliac oblique images demonstrating the initial misdirection of the guidewire with bent tip during percutaneous retrograde screw fixation of an acetabular posterior column. The guidewire was carefully retracted and rotated to correct the misaligned trajectory
Percutaneous fracture reduction
The technique is also effectively utilized in cases of mild displacement or translation at the fracture site. The guidewire with a bent tip is carefully advanced closer to the fracture site and utilized as a joystick to aid in fracture reduction. If more forceful manipulation is required, a 4.5-mm cannulated drill is advanced over the straight section of the guidewire. Subsequently, the cannulated drill is removed, and a protective cannulated drill sleeve is inserted over the guidewire to facilitate manual manipulation of the fracture. Once reduction is achieved, the bent guidewire is advanced beyond the fracture site, engaging the other end under biplanetary fluoroscopic guidance. Correct placement is confirmed using orthogonal fluoroscopic views, and the cannulated drill is advanced until the desired depth is achieved. (Fig. 3).
Sequence of intraoperative fluoroscopic pelvic inlet images demonstrating the intramedullary insertion of a 3.5 mm guidewire into the superior pubic ramus. The guidewire was advanced carefully toward the fracture site, followed by the insertion of a protective cannulated drill sleeve over the guidewire to aid in manual manipulation of the fracture
Postoperative care
Postoperative care involves active encouragement for patients to commence early ambulation as part of their recovery process. The timing and manner of weight-bearing, whether using a walker or crutches, are determined based on individual factors such as the fracture pattern and the quality of reduction achieved. Typically, patients remain hospitalized for a duration of 2 to 3 days after the surgical procedure to effectively manage postoperative pain. Postoperative radiographic imaging of the pelvis is routinely conducted to evaluate the final reduction. In select cases, a CT scan may be warranted for further evaluation. (Fig. 4).
Results
Patient demographics and injury details
Between August 2020 and August 2023, we identified 25 patients with pelvic ring and acetabular fractures at a Level I trauma center who had complete medical records. The cohort was predominantly male, with 23 males and 2 females. The average age among these patients was 38 years, ranging from 21 to 54 years old. The most common cause of injury was traffic accidents, which accounted for the injuries in 18 patients, while falls were responsible for the injuries in the remaining 7 patients. The distribution of the types of injuries was as follows: 6 patients presented with pelvic ring injuries, 8 with acetabular fractures, and the remaining 11 had a combination of both types of injuries. A summary of the fracture types is provided in Table 1.
Treatment details
The treatment involved the use of various types of screws, which included anterior column screws (both antegrade and retrograde), retrograde posterior column screws, and LC2 screws (both antegrade and retrograde). It is worth noting that in certain cases, it was necessary to utilize a combination of different screw fixations (Table 2).
Outcomes
All the patients were subjected to regular follow-ups, with the average follow-up period being 18 months, ranging from a minimum of 3 months to a maximum of 36 months. At the time of the final follow-up, it was observed that none of the patients had the need for any additional procedures or revision surgery. Furthermore, there were no reported complications, such as neurovascular injury, wound infections, loss of initial reduction, nonunion, or hardware failure. This suggests that the treatment was successful and well-tolerated by all patients.
Discussion
Percutaneous fixation for pelvic and acetabular fractures is a critical tool for trauma surgeons, particularly for managing minimally displaced injuries [11]. Our study has shown that utilizing a modified guidewire technique significantly enhances the precision required for screw placement in these procedures [7]. The results revealed a perfect technical success rate without the need for postoperative interventions or occurrence of complications, suggesting a promising improvement in the standard percutaneous fixation protocol [12, 13].
Traditional methods for percutaneous reduction and fixation in pelvic and acetabular fractures primarily use standard guidewires [7, 11, 12]. While these are fundamentally effective, they occasionally encounter difficulties in unique fracture patterns and anatomical contexts [4]. Our technique, which employs a guidewire with a bent tip, skillfully addresses such misdirections. This not only provides a streamlined and invaluable method for critical corrections, saving vital operative time during percutaneous screw fixation but also facilitates medullary manipulation. This key feature allows for the realignment of displaced pelvic superior ramus and acetabulum column fractures before screw insertion. This modification provides enhanced tactile feedback, making it an alternative choice for surgeons seeking optimized real-time adjustments. While the existing techniques, which sometimes require multiple iterations and potentially heighten the risk of soft tissue damage, our described technique demonstrates a potential advantage in efficiency and precision [7]
The minimally invasive nature of this technique also implies smaller incisions, which generally results in less postoperative pain, reduced scarring, and quicker healing. Alzobi et al. [13] similarly endorsed percutaneous sacroiliac screw fixation, deeming it a safe surgical technique for unstable pelvic trauma, with low complication rates, although they reported a complication related to screw malposition at a rate of 6%. These findings align with the existing literature. Parker et al. in their study of acetabular column fixation, noted that blood loss was under 100 mL for each patient treated with percutaneous fixation [6]. Additionally, Bozzio et al. [14] reported a reduction in fracture displacement with percutaneous surgical treatment and observed good-to-excellent outcomes in patients.
The success of the outcomes greatly depends on precise patient selection. Tailoring the current technique to the fracture type, location, and severity, has been instrumental in maximizing its benefits over traditional open surgeries [15, 16]. This method effectively addressed pelvic ring fractures, notably lateral compression types (I, II, and III). Similarly, for acetabular fractures, it encompassed types from anterior or posterior column transverse and T-shape to combined varieties. While ideal for minimally displaced fractures, more complex cases sometimes required a combined approach of open and percutaneous techniques.
Despite its benefits, the technique presents certain challenges, particularly during the removal of the guidewire after insertion of the cannulated screw. The primary issue arises from the bent-tip part of the guidewire. To address this challenge, several options can be considered. Advancing the guidewire and removing it from the opposite site may be a good solution, but it is only useful in cases of retrograde pubic ramus screw placement. Another strategy involves avoiding hyper-bending of the guidewire tip during insertion. Our recommendation is to limit the degree of bending to 25–30 degrees, thus minimizing the risk of entanglement during removal. Alternatively, the use of a smaller caliber guidewire, such as size 2 or 2.5 mm, for 6.5 cannulated screws can mitigate this issue. However, it is important to note that a smaller guidewire may not serve as an effective reduction tool to correct minor displacements at the fracture site. Following cannulated drilling with a 4.5-mm drill over the guidewire, replacing the bent-tip guidewire with a similar or smaller size straight guidewire is another potential solution.
The main limitation of this technique lies in its infrequent necessity. It is typically required in specific cases, making its application less common. However, surgeons who are familiar with percutaneous fixation of pelvic and acetabular fractures can apply this technique with a relatively small learning curve. Moreover, it is important to note that not all acetabular fracture types are suitable for percutaneous fixation. At our institution, when faced with fractures unsuitable for this approach, we revert to the standard open techniques, using well-established extensile approaches. Weaknesses of this study include its retrospective nature. Additionally, standardized functional outcomes were not systematically collected during routine follow-up appointments with the patients. It is important to note that the purpose of this manuscript was to report on a practical and simple solution addressing the challenges of guidewire misdirection, thereby minimizing the need for multiple guidewire adjustments in patients with narrow and challenging osseous corridors in the pelvic ring or acetabulum. Our focus was not on evaluating the clinical or functional outcomes of a diverse group of pelvic ring injuries and acetabular fractures.
In summary, the utilization of a modified guidewire with a bent tip offers a versatile solution for trauma surgeons in enhancing the precision of percutaneous screw placement within pelvic and acetabular fractures. This technique not only facilitates minor yet crucial corrections to the initially misaligned screw trajectory but also proven effective in addressing specific fracture malalignments prior to percutaneous screw fixation. However, additional research involving a larger cohort is essential to conclusively ascertain the effectiveness of this construct compared to established alternatives.
Data availability
All date will be available on request.
References
Yoshihara H, Yoneoka D (2014) Demographic epidemiology of unstable pelvic fracture in the United States from 2000 to 2009: trends and in-hospital mortality. J Trauma Acute Care Surg 76(2):380–385. https://doi.org/10.1097/TA.0b013e3182ab0cde
Routt ML, Kregor PJ, Simonian PT, Mayo KA (1995) Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma 9(3):207–214. https://doi.org/10.1097/00005131-199506000-00005
Arbash M, Alzobi OZ, Salameh M, Alkhayarin M, Ahmed G (2024) Incidence, risk factors, and prognosis of sciatic nerve injury in acetabular fractures: a retrospective cross-sectional study. Int Orthop. https://doi.org/10.1007/s00264-024-06087-7
Caviglia H, Mejail A, Landro ME, Vatani N (2018) Percutaneous fixation of acetabular fractures. EFORT Open Rev 3(5):326–334. https://doi.org/10.1302/2058-5241.3.170054
Kazemi N, Archdeacon MT (2012) Immediate full weightbearing after percutaneous fixation of anterior column acetabulum fractures. J Orthop Trauma 26(2):73–79. https://doi.org/10.1097/BOT.0b013e318216b3e3
Yi C, Burns S, Hak DJ (2014) Intraoperative fluoroscopic evaluation of screw placement during pelvic and acetabular surgery. J Orthop Trauma 28(1):48–56. https://doi.org/10.1097/BOT.0b013e318288c0c3
Banaszek D, Starr AJ, Lefaivre KA (2019) Technical considerations and fluoroscopy in percutaneous fixation of the pelvis and acetabulum. J Am Acad Orthop Surg 27(24):899–908. https://doi.org/10.5435/JAAOS-D-18-00102
Elmhiregh A, Hantouly AT, Alzobi O, George B, Ahmadi M, Ahmed G (2023) The optimal fluoroscopic views to rule out intra-articular screw penetration during acetabular fracture fixation. Int Orthop. https://doi.org/10.1007/s00264-023-06002-6
Young JW, Burgess AR, Brumback RJ, Poka A (1986) Pelvic fractures: value of plain radiography in early assessment and management. Radiology 160(2):445–451. https://doi.org/10.1148/radiology.160.2.3726125
Letournel E, Judet R (1981) Fractures of the acetabulum. In R. A. Elson (Ed.), Berlin (Heidelburg): SpringerVerlag.
Starr AJ, Reinert CM, Jones AL (1998) Percutaneous fixation of the columns of the acetabulum: a new technique. J Orthop Trauma 12:51–58
Ochs BG, Gonser C, Shiozawa T, Badke A, Weise K, Rolauffs B, Stuby FM (2010) Computer-assisted periacetabular screw placement: comparison of different fluoroscopy-based navigation procedures with conventional technique. Injury 41(12):1297–1305. https://doi.org/10.1016/j.injury.2010.07.502
Alzobi OZ, Alborno Y, Toubasi A et al (2023) Complications of conventional percutaneous sacroiliac screw fixation of traumatic pelvic ring injuries: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol 33:3107–3117
Bozzio AE, Wydra FB, Mitchell JJ, Ackerson RM, Mauffrey C (2014) Percutaneous fixation of anterior and posterior column acetabular fractures. Orthopedics 37(10):675–678. https://doi.org/10.3928/01477447-20140924-04
Mudawi A, Moghamis IS, Alzobi O, Babikir E, Abdelsalam S, Samhadaneh MA (2022) Bilateral pelvic crescent fracture combined with left acetabular fracture: a case report. Int J Surg Case Rep 99:107701. https://doi.org/10.1016/j.ijscr.2022.107701
Hantouly AT, Salman LA, Toubasi AT, Alzobi O, Alborno Y, Kayali H et al (2023) Prone or lateral patient positioning in Kocher Langenbeck approach in acetabular fractures fixation: a systematic review and meta-analysis. J Musculoskelet Surg Res. https://doi.org/10.25259/JMSR_127_2023
Funding
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors, including Aiman Mudawi, Osama Alzobi, Jawad Nouraldeen Derbas, Ghalib Ahmed, and Maamoun Abousamhadaneh declare that they have no funding or commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethical approval
There is a statement of the Institutional Review Board for this work.
Consent to participate
Not applicable.
Consent for publication
All authors have approved the publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mudawi, A., Alzobi, O., Derbas, J.N. et al. Optimizing percutaneous reduction and fixation with guidewire modification in pelvic and acetabular fractures: surgical technique and case series. Eur J Orthop Surg Traumatol 34, 2107–2112 (2024). https://doi.org/10.1007/s00590-024-03905-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-024-03905-x