Abstract
Introduction
Pelvic ring fractures, particularly those involving the posterior pelvis, pose significant challenges due to their inherent instability. The posterior pelvic ring is critical in providing structural support and stability to the pelvis. This study evaluates the functional outcomes and health-related Quality of life (HRQOL) of patients who underwent internal fixation for unstable pelvic fractures. Various factors influencing the outcomes are also investigated.
Material and Methods
A single-center cross-sectional study was conducted on patients with unstable sacral fractures treated with posterior tension band plate or sacroiliac plating with or without symphyseal plating between 2016 and 2020. Patient demographics, injury mechanisms, associated injuries, surgical details, complications, and return-to-work data were collected. HRQOL was assessed using specific pelvic fracture instruments and general HRQOL questionnaires. Logistic regression analysis was performed to identify factors associated with lower SF-12 and SF-36 scores
Results
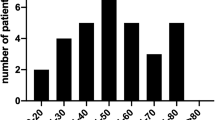
The study included 54 patients, predominantly males (55.6%), aged 18–70 years, with high-energy trauma mechanisms, such as road traffic accidents and occupational injuries. The majority of patients had lateral compression pelvic fractures. Overall, the functional outcomes were favorable, with excellent or good outcomes observed in 86.1% of cases. Patients with associated injuries, such as abdominal, chest, or head injuries, were likelier to have lower SF-12 physical component scores. Sexual satisfaction scores remained stable for most patients post-surgery.
Discussion
This study highlights the favorable functional outcomes and HRQOL for patients undergoing fixation for unstable pelvic ring fractures. Younger, working-age males were the most commonly affected demographic. Associated injuries significantly affected physical HRQOL scores. Despite high-energy trauma, patients generally reported satisfactory sexual function post-surgery



Similar content being viewed by others
References
Khurana B, Sheehan SE, Sodickson AD, Weaver MJ (2014) Pelvic ring fractures: what the orthopaedic surgeon wants to know. Radiographics 34(5):1317–1333
Tornetta P, Matta JM (1996) The outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res 329:186–193
Lu Y, He Y, Li W, Yang Z, Peng R, Yu L (2020) Comparison of biomechanical performance of five different treatment approaches for fixing posterior pelvic ring injury. J Healthc Eng 2020:11–15
Mardanpour K, Rahbar M (2013) The outcome of surgically treated traumatic unstable pelvic fractures by open reduction and internal fixation. J Inj Violence Res 5(2):87–93
Zhang R, Yin Y, Li S, Hou Z, Jin L, Zhang Y (2018) Percutaneous sacroiliac screw versus anterior plating for sacroiliac joint disruption: a retrospective cohort study. Int J Surg [Internet] 50:11–16. https://doi.org/10.1016/j.ijsu.2017.12.017
Kokubo Y, Oki H, Sugita D, Takeno K, Miyazaki T, Negoro K et al (2017) Functional outcome of patients with unstable pelvic ring fracture: comparison of short- and long-term prognostic factors. J Orthop Surg 25(1):1–6
Khaleel VM, Pushpasekaran N, Prabhu N, Pandiyan A, Koshy GM (2019) Posterior tension band plate osteosynthesis for unstable sacral fractures: a preliminary study. J Clin Orthop Trauma [Internet] 10:S106–S111. https://doi.org/10.1016/j.jcot.2019.05.017
Matta JM, Tornetta P (1996) Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res 329:129–140
Krappinger D, Larndorfer R, Struve P, Rosenberger R, Arora R, Blauth M (2007) Minimally invasive transiliac plate osteosynthesis for type C injuries of the pelvic ring: a clinical and radiological follow-up. J Orthop Trauma 21(9):595–602
Cole J, Blum D, Ansel L (1996) Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res 329:160–179
Borg T, Berg P, Fugl-Meyer K, Larsson S (2010) Health-related quality of life and life satisfaction in patients following surgically treated pelvic ring fractures. A prospective observational study with two years follow-up. Injury 41(4):400–404
Dienstknecht T, Pfeifer R, Horst K, Sellei RM, Berner A, Zelle BA et al (2013) The long-term clinical outcome after pelvic ring injuries. Bone Joint J 95:548–553
Prieto-Alhambra D, Avilés F, Judge A, Van Staa T, Nogués X, Arden N et al (2012) Burden of pelvis fracture: a population-based study of incidence, hospitalization and mortality. Osteoporos Int 23(12):2797–2803
Andrich S, Haastert B, Neuhaus E, Neidert K, Arend W, Ohmann C et al (2015) Epidemiology of pelvic fractures in Germany: considerably high incidence rates among older people. PLoS ONE 10(9):e0139078
Giannoudis PV, Grotz MRW, Tzioupis C et al (2007) Prevalence of pelvic fractures, associated injuries, and mortality: the United Kingdom perspective. J Trauma Inj Infect Crit Care 63(4):875e883
Palmcrantz J, Hardcastle TC, Naidoo SR, Muckart DJJ, Ahlm K, Eriksson A (2012) Pelvic fractures at a new level 1 trauma centre: who dies from pelvic trauma? The Inkosi Albert Luthuli central hospital experience. Orthop Surg 4(4):216e221
Yoon Y, Ma D, Lee S, Oh J, Song H (2021) Posterior pelvic ring injury of straddle fractures: incidence, fixation methods, and clinical outcomes. Asian J Surg 44(1):59–65
Harvey-Kelly KF, Kanakaris NK, Obakponovwe O, West RM, Giannoudis PV (2014) Quality of life and sexual function after traumatic pelvic fracture. J Orthop Trauma 28:28–35
Brouwers L, Lansink K, de Jongh M (2018) Quality of life after pelvic ring fractures: a cross-sectional study. Injury 49(4):812–818
Odutola A, Sabri O, Halliday R, Chesser T, Ward A (2012) High rates of sexual and urinary dysfunction after surgically treated displaced pelvic ring injuries. Clin Orthop Relat Res 470(8):2173–2184
Bott A, Nicol G, Odutola A, Halliday R, Acharya M, Ward A et al (2022) Long-term patients reported sexual and urological dysfunction in males after operatively treated pelvic ring injuries. Do generic outcome measures identify genitourinary health problems? Injury 53(6):2139–2144
Funding
The author declares that they have no funding statement.
Author information
Authors and Affiliations
Contributions
All the above-mentioned authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elhence, A., Netaji, J., Yadav, S.K. et al. Functional outcome and analysis of factors affecting health-related quality of life of surgically managed pelvic ring fractures: a cross-sectional study. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-03869-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-03869-y