Abstract
Aim
Polymers and metals, such as polyethylene (PE) and cobalt chrome (CoCr), are common materials used in thumb-based joint implants, also known as CMC (Carpometacarpal) arthroplasty. The purpose of this review was to investigate the reported failure modes related to wear debris from these type of materials in CMC implants. The impact of wear debris on clinical outcomes of CMC implants was also examined. Potential adverse wear conditions and inflammatory particle characteristics were also considered.
Method
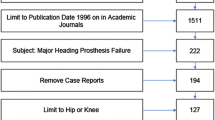
A literature search was performed using PRISMA guidelines and 55 studies were reviewed including 49 cohort studies and 6 case studies. Of the 55 studies, 38/55 (69%) focused on metal-on-polyethylene devices, followed by metal-on-metal (35%), and metal-on-bone (4%).
Results
The summarized data was used to determine the frequency of failure modes potentially related to wear debris from metals and/or polymers. The most commonly reported incidents potentially relating to debris were implant loosening (7.1%), osteolysis (1.2%) and metallosis (0.6%). Interestingly the reported mechanisms behind osteolysis and loosening greatly varied. Inflammatory reactions, while rare, were generally attributed to metallic debris from metal-on-metal devices.
Mechanisms of adverse wear conditions included implant malpositioning, over-tensioning, high loading for active patients, third-body debris, and polyethylene wear-through. No specific examination of debris particle characterization was found, pointing to a gap in the literature.
Conclusion
This review underscores the types of failure modes associated with wear debris in CMC implants. It was found that failure rates and adverse wear conditions of CMC implants of any design are low and the exact relationship between wear debris and implant incidences, such as osteolysis and loosening remains uncertain. The authors note that further research and specific characterization is required to understand the relationship between debris and implant failure.




Similar content being viewed by others
References
Armstrong A, Hunter J, Davis T (1994) The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg 19(3):340–341. https://doi.org/10.1016/0266-7681(94)90085-X
Berger AJ, Meals RA (2015) Management of osteoarthrosis of the thumb joints. J Hand Surg 40(4):843–850. https://doi.org/10.1016/j.jhsa.2014.11.026
Huang K, Hollevoet N, Giddins G (2015) Thumb carpometacarpal joint total arthroplasty: a systematic review. J Hand Surg 40(4):338–350. https://doi.org/10.1177/1753193414563243
Srnec JJ, Wagner ER, Rizzo M (2017) Implant arthroplasty for proximal interphalangeal, metacarpophalangeal, and trapeziometacarpal joint degeneration. J Hand Surg Am 42(10):817–825. https://doi.org/10.1016/j.jhsa.2017.07.030
Remy S, Detrembleur C, Libouton X, Bonnelance M, Barbier O (2020) Trapeziometacarpal prosthesis: an updated systematic review. Hand Surg Rehabil 39(6):492–501. https://doi.org/10.1016/j.hansur.2020.08.005
Bæk Hansen T (2021) Joint replacement for trapeziometacarpal osteoarthritis: implants and outcomes. J Hand Surg 46(2):115–119. https://doi.org/10.1177/1753193420917582
Holme TJ, Karbowiak M, Clements J, Sharma R, Craik J, Ellahee N (2021) Thumb CMCJ prosthetic total joint replacement: a systematic review. EFORT Open Rev 6(5):316–330. https://doi.org/10.1302/2058-5241.6.200152
Satteson ES, Langford MA, Li Z (2015) The management of complications of small joint arthrodesis and arthroplasty. Hand Clin 31(2):243–266. https://doi.org/10.1016/j.hcl.2015.01.002
Vitale MA, Taylor F, Ross M, Moran SL (2013) Trapezium prosthetic arthroplasty (silicone, Artelon, metal, and pyrocarbon). Hand Clin 29(1):37–55. https://doi.org/10.1016/j.hcl.2012.08.020
Moher D, Liberati A, Tetzlaff J, Altman DG, P. Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Eecken SV, Vanhove W, Hollevoet N (2012) Trapeziometacarpal joint replacement with the Arpe prosthesis. Acta Orthop Belg 78(6):724–9
De Smet A et al (2020) Ten-year outcomes of the Arpe prosthesis for the treatment of osteoarthritis of the trapeziometacarpal joint. Acta Orthop Belg 86(1):131–136
Goubau JF, Goorens CK, Van Hoonacker P, Berghs B, Kerckhove D, Scheerlinck T (2013) Clinical and radiological outcomes of the Ivory arthroplasty for trapeziometacarpal joint osteoarthritis with a minimum of 5 years of follow-up: a prospective single-centre cohort study. J Hand Surg Eur 38(8):866–874. https://doi.org/10.1177/1753193413488494
Vissers G, Goorens CK, Vanmierlo B, Bonte F, Mermuys K, Fils JF, Goubau JF (2019) Ivory arthroplasty for trapeziometacarpal osteoarthritis: 10-year follow-up. J Hand Surg Eur 44(2):138–145. https://doi.org/10.1177/1753193418797890
Andrzejewski A, Ledoux P (2019) Maïa(®) trapeziometacarpal joint arthroplasty: survival and clinical outcomes at 5 years’ follow-up. Hand Surg Rehabil 38(3):169–173. https://doi.org/10.1016/j.hansur.2019.03.004
Badia A, Sambandam SN (2006) Total joint arthroplasty in the treatment of advanced stages of thumb carpometacarpal joint osteoarthritis. J Hand Surg Am 31(10):1605–14. https://doi.org/10.1016/j.jhsa.2006.08.008
Bricout M, Rezzouk J (2016) Complications and failures of the trapeziometacarpal Maia(®) prosthesis: a series of 156 cases. Hand Surg Rehabil 35(3):190–198. https://doi.org/10.1016/j.hansur.2016.02.005
Cebrian-Gomez R et al (2019) Outcomes of cementless joint prosthesis versus tendon interposition for trapeziometacarpal osteoarthritis: a prospective study. J Hand Surg Eur 44(2):151–158. https://doi.org/10.1177/1753193418787151
Chiche L, Lamarre H, Barbary S, Teissier J (2020) Scaphometacarpal arthroplasty: a report of ten cases of trapeziometacarpal prosthesis and trapeziectomy revision. J Hand Surg Eur 45(5):483–487. https://doi.org/10.1177/1753193419900470
Chug M et al (2014) Outcome of uncemented trapeziometacarpal prosthesis for treatment of thumb carpometacarpal joint arthritis. Indian J Orthop. 48(4):394–398. https://doi.org/10.4103/0019-5413.136270
Cootjans K, Vanhaecke J, Dezillie M, Barth J, Pottel H, Stockmans F (2017) Joint survival analysis and clinical outcome of total joint arthroplasties with the ARPE implant in the treatment of trapeziometacarpal osteoarthritis with a minimal follow-up of 5 years. J Hand Surg Am 42(8):630–638. https://doi.org/10.1016/j.jhsa.2017.05.007
De Smet L et al (2004) Total joint arthroplasty for osteoarthritis of the thumb basal joint. Acta Orthop Belg 70(1):19–24
Dehl M, Chelli M, Lippmann S, Benaissa S, Rotari V, Moughabghab M (2017) Results of 115 Rubis II reverse thumb carpometacarpal joint prostheses with a mean follow-up of 10 years. J Hand Surg Eur 42(6):592–598. https://doi.org/10.1177/1753193416687508
Dreant N, Poumellec MA (2019) Total thumb carpometacarpal joint arthroplasty: a retrospective functional study of 28 MOOVIS prostheses. Hand 14(1):59–65. https://doi.org/10.1177/1558944718797341
Dremstrup L, Thillemann JK, Kirkeby L, Larsen LP, Hansen TB, Stilling M (2021) Two-year results of the Moovis trapeziometacarpal joint arthroplasty with focus on early complications. J Hand Surg Eur 46(2):131–140. https://doi.org/10.1177/1753193420921307
Dumartinet-Gibaud R, Bigorre N, Raimbeau G, Jeudy J, Saint Cast Y (2020) Arpe total joint arthroplasty for trapeziometacarpal osteoarthritis: 80 thumbs in 63 patients with a minimum of 10 years follow-up. J Hand Surg Eur 45(5):465–469. https://doi.org/10.1177/1753193420909198
Froschauer SM, Holzbauer M, Hager D, Schnelzer R, Kwasny O, Duscher D (2020) Elektra prosthesis versus resection-suspension arthroplasty for thumb carpometacarpal osteoarthritis: a long-term cohort study. J Hand Surg Eur 45(5):452–457. https://doi.org/10.1177/1753193419873230
Froschauer SM et al (2021) TOUCH® prosthesis for thumb carpometacarpal joint osteoarthritis: a prospective case series. J Clin Med 10(18):4090. https://doi.org/10.3390/jcm10184090
Froschauer SM et al (2020) Total arthroplasty with Ivory(®) prosthesis versus resection-suspension arthroplasty: a retrospective cohort study on 82 carpometacarpal-I osteoarthritis patients over 4 years. Eur J Med Res 25(1):13. https://doi.org/10.1186/s40001-020-00411-8
Gómez-Garrido D et al (2019) Five year long term results of total joint arthroplasties in the treatment of trapeziometacarpal osteoarthritis. Acta Biomed 90(4):451–456
Gonzalez-Espino P et al (2021) Touch® double mobility arthroplasty for trapeziometacarpal osteoarthritis: outcomes for 92 prostheses. Hand Surg Rehabil. https://doi.org/10.1016/j.hansur.2021.08.005
Hansen TB, Snerum L (2008) Elektra trapeziometacarpal prosthesis for treatment of osteoarthrosis of the basal joint of the thumb. Scand J Plast Reconstr Surg Hand Surg 42(6):316–319. https://doi.org/10.1080/02844310802393974
Hansen TB, Dremstrup L, Stilling M (2013) Equally good fixation of cemented and uncemented cups in total trapeziometacarpal joint prostheses. A randomized clinical RSA study with 2-year follow-up. Acta Orthop 84(1):98–105
Hansen TB, Dremstrup L, Stilling M (2013) Patients with metal-on-metal articulation in trapeziometacarpal total joint arthroplasty may have elevated serum chrome and cobalt. J Hand Surg Eur 38(8):860–865. https://doi.org/10.1177/1753193413487685
Hernández-Cortés P, Pajares-López M, Robles-Molina MJ, Gómez-Sánchez R, Toledo-Romero MA, De Torres-Urrea J (2012) Two-year outcomes of Elektra prosthesis for trapeziometacarpal osteoarthritis: a longitudinal cohort study. J Hand Surg Eur 37(2):130–137. https://doi.org/10.1177/1753193411414505
Johnston P et al (2012) De la Caffinière thumb trapeziometacarpal joint arthroplasty: 16–26 year follow-up. J Hand Surg Eur 37(7):621–624. https://doi.org/10.1177/1753193411433226
Smith E, Mehta AJ, Statham BN (2009) Metal sensitivity to Elektra™ prostheses-two cases from a metal on metal implant for hand joint replacement. Contact dermatitis 60(5):298–298. https://doi.org/10.1111/j.1600-0536.2009.01535
Kirkeby L et al (2021) Revision rates of trapeziometacarpal total joint arthroplasty in relation to occupational hand force requirements. J Hand Surg Eur. https://doi.org/10.1177/1753193421996980
Klahn A, Nygaard M, Gvozdenovic R, Boeckstyns ME (2012) Elektra prosthesis for trapeziometacarpal osteoarthritis: a follow-up of 39 consecutive cases. J Hand Surg Eur 37(7):605–609. https://doi.org/10.1177/1753193412443501
Lemoine S et al (2009) Second generation GUEPAR total arthroplasty of the thumb basal joint: 50 months follow-up in 84 cases. Orthop Traumatol Surg Res 95(1):63–9. https://doi.org/10.1016/j.otsr.2008.06.001
Lussiez B, Falaise C, Ledoux P (2021) Dual mobility trapeziometacarpal prosthesis: a prospective study of 107 cases with a follow-up of more than 3 years. J Hand Surg Eur. https://doi.org/10.1177/17531934211024500
Martin-Ferrero M (2014) Ten-year long-term results of total joint arthroplasties with ARPE® implant in the treatment of trapeziometacarpal osteoarthritis. J Hand Surg Eur 39(8):826–32. https://doi.org/10.1177/1753193413516244
Martin-Ferrero M et al (2020) Trapeziometacarpal total joint arthroplasty for osteoarthritis: 199 patients with a minimum of 10 years follow-up. Journal of Hand Surgery (European Volume) 45(5):443–451. https://doi.org/10.1177/1753193419871660
Martin-Ferrero MA, Trigueros-Larrea JM, Martin-de la Cal E, Coco-Martin B, Simon-Perez C (2021) Long-term results of joint arthroplasty with total prosthesis for trapeziometacarpal osteoarthritis in patients over 65 years of age. Geriatrics, 6(3). https://doi.org/10.3390/geriatrics6030065
Martins A et al (2020) The Moovis® implant for trapeziometacarpal osteoarthritis: results after 2 to 6 years. J Hand Surg Eur 45(5):477–482. https://doi.org/10.1177/1753193420901435
Pritchett JW, Habryl LS (2012) A promising thumb Basal joint hemiarthroplasty for treatment of trapeziometacarpal osteoarthritis. Clin Orthop Relat Res 470(10):2756–63. https://doi.org/10.1007/s11999-012-2367-7
Regnard PJ (2006) Electra trapezio metacarpal prosthesis: results of the first 100 cases. J Hand Surg Br 31(6):621–628. https://doi.org/10.1016/J.JHSB.2006.05.019
Semere A, Vuillerme N, Corcella D, Forli A, Moutet F (2015) Results with the Roseland(®) HAC trapeziometacarpal prosthesis after more than 10 years. Chir Main 34(2):59–66. https://doi.org/10.1016/j.main.2015.01.004
Skyttä ET et al (2005) Use of the de la Caffinière prosthesis in rheumatoid trapeziometacarpal destruction. J Hand Surg Br 30(4):395–400. https://doi.org/10.1016/J.JHSB.2005.03.012
Spaans AJ, van Minnen LP, Weijns ME, Braakenburg A, van der Molen AB (2016) Retrospective study of a series of 20 ivory prostheses in the treatment of trapeziometacarpal osteoarthritis. J Wrist Surg 5(2):131–136. https://doi.org/10.1055/s-0036-1571283
Tchurukdichian A et al (2021) Outcomes of Double-Mobility Prosthesis in Trapeziometacarpal Joint Arthritis With a Minimal 3 Years of Follow-Up: an Advantage for Implant Stability. Hand (N Y) 16(3):368–374. https://doi.org/10.1177/1558944719855690
Tchurukdichian A et al (2020) Results of 110 IVORY® prostheses for trapeziometacarpal osteoarthritis with a minimum follow-up of 10 years. J Hand Surg Eur 45(5):458–464. https://doi.org/10.1177/1753193419899843
Thillemann JK, Thillemann TM, Munk B, Krøner K (2016) High revision rates with the metal-on-metal Motec carpometacarpal joint prosthesis. J Hand Surg Eur 41(3):322–327. https://doi.org/10.1177/1753193415595527
Toffoli A, Teissier J (2017) MAÏA trapeziometacarpal joint arthroplasty: clinical and radiological outcomes of 80 patients with more than 6 years of follow-up. J Hand Surg Am 42(10):838.e831-838.e838. https://doi.org/10.1016/j.jhsa.2017.06.008
Ulrich-Vinther M, Puggaard H, Lange B (2008) Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg Am 33(8):1369–1377. https://doi.org/10.1016/j.jhsa.2008.04.028
Vanmierlo B, Buitenweg J, Vanmierlo T, Van Royen K, Bonte F, Goubau J (2020) Ivory arthroplasty for trapeziometacarpal joint arthritis in men: analysis of clinical outcome and implant survival. Hand. https://doi.org/10.1177/1558944720930297
Zollinger PE et al (2008) Clinical outcome of cementless semi-constrained trapeziometacarpal arthroplasty, and possible effect of vitamin C on the occurrence of complex regional pain syndrome. Acta Orthop Belg 74(3):317–22
Phaltankar PM, Magnussen PA (2003) Hemiarthroplasty for trapeziometacarpal arthritis - a useful alternative? J Hand Surg Br 28(1):80–85. https://doi.org/10.1054/JHSB.2002.0861
Thorkildsen RD, Røkkum M (2019) Trapeziectomy with LRTI or joint replacement for CMC1 arthritis, a randomised controlled trial. J Plast Surg Hand Surg 53(6):361–369. https://doi.org/10.1080/2000656X.2019.1635490
Robles-Molina MJ et al (2017) Trapeziectomy With Ligament Reconstruction and Tendon Interposition Versus a Trapeziometacarpal Prosthesis for the Treatment of Thumb Basal Joint Osteoarthritis. Orthopedics 40(4):e681–e686. https://doi.org/10.3928/01477447-20170503-03
Bigorre N, Petit A, Gibaud-Dumartinet R, Saint-Cast Y, Raimbeau G (2021) Revision of Arpe® trapeziometacarpal prosthesis by isolated head and linear exchange in five patients. Hand Surg Rehabil 40(3):305–308. https://doi.org/10.1016/j.hansur.2020.12.009
Cootjans K et al (2019) Salvage revision arthroplasty after failed TMC joint prosthesis. Acta Orthop Belg 85(3):325–329
Frølich C, Hansen TB (2015) Complications related to metal-on-metal articulation in trapeziometacarpal joint total joint arthroplasty. J Funct Biomater 6(2):318–327. https://doi.org/10.3390/jfb6020318
Schmidt I (2014) Thumb CMC total exchange arthroplasty with the ARPE implant. Chir Main 33(4):295–298. https://doi.org/10.1016/j.main.2014.04.005
Thorkildsen RD, et al (2020) Early cup loosening after metal-on-metal total joint replacement of the trapeziometacarpal joint: a retrieval study. J Hand Surg Am 45(3):213–222. https://doi.org/10.1016/j.jhsa.2019.06.020
McGrory BJ, et al (2020) Standardizing terms for tribocorrosion-associated adverse local tissue reaction in total hip arthroplasty. Arthroplast Today 6(2):196–200. https://doi.org/10.1016/j.artd.2020.01.008
Bitar D, Parvizi J (2015) Biological response to prosthetic debris. World J Orthop 6(2):172. https://doi.org/10.5312/wjo.v6.i2.172
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Search statement #1
Search: (((UHMW* OR POLYETHYLENE OR “Metal ions” OR “metal ion” OR Particl* OR Particulate OR Debris OR Metallosis OR Pain OR “Adverse local tissue” OR ALTR OR ARMD OR “Adverse Reaction to Metal Debris” OR “Adverse reactions to metal debris” OR Revision OR loosening) AND (thumb OR CMC OR CMCJ OR trapeziometacarpal OR TMCJ OR carpometacarpal) AND (implant* OR Arthroplasty OR “Joint replacement” OR prosthesis) NOT (silicon).
Search Detail:
(((“uhmw*”[All Fields] OR (“polyethene”[All Fields] OR “polyethylenes”[MeSH Terms] OR “polyethylenes”[All Fields] OR “polyethylene”[All Fields] OR “polyethylene”[MeSH Terms] OR “polyethylen”[All Fields]) OR “Metal ions”[All Fields] OR “metal ion”[All Fields] OR “particl*”[All Fields] OR (“particulate”[All Fields] OR “particulates”[All Fields]) OR “Debris”[All Fields] OR “Metallosis”[All Fields] OR (“pain”[MeSH Terms] OR “pain”[All Fields]) OR “Adverse local tissue”[All Fields] OR “ALTR”[All Fields] OR “ARMD”[All Fields] OR “Adverse Reaction to Metal Debris”[All Fields] OR “Adverse reactions to metal debris”[All Fields] OR (“revise”[All Fields] OR “revised”[All Fields] OR “revisers”[All Fields] OR “revises”[All Fields] OR “revising”[All Fields] OR “revision”[All Fields] OR “revisions”[All Fields]) OR (“loosen”[All Fields] OR “loosened”[All Fields] OR “loosening”[All Fields] OR “loosenings”[All Fields] OR “loosens”[All Fields])) AND “english”[Language] AND ((“thumb”[MeSH Terms] OR “thumb”[All Fields] OR “thumbs”[All Fields] OR “thumb s”[All Fields] OR “CMC”[All Fields] OR “CMCJ”[All Fields] OR “trapeziometacarpal”[All Fields] OR “TMCJ”[All Fields] OR “carpometacarpal”[All Fields]) AND “english”[Language]) AND ((“implant*”[All Fields] OR (“arthroplasty”[MeSH Terms] OR “arthroplasty”[All Fields] OR “arthroplasties”[All Fields]) OR “Joint replacement”[All Fields] OR (“prostheses and implants”[MeSH Terms] OR (“prostheses”[All Fields] AND “implants”[All Fields]) OR “prostheses and implants”[All Fields] OR “prosthesis”[All Fields])) AND “english”[Language]) AND (2001/01/01:3000/12/12[Date—Publication] AND “english”[Language])) NOT ((“silicon”[MeSH Terms] OR “silicon”[All Fields] OR “silicon s”[All Fields] OR “silicons”[All Fields]) AND ((english[Filter]) AND(2001:2021[pdat])).
Search statement #2
SU,TI,AB(UHMW* OR POLYETHYLENE OR “Metal ions” OR “metal ion” OR Particl* OR Particulate OR Debris OR Metallosis OR Pain OR “Adverse local tissue” OR ALTR OR ARMD OR “Adverse Reaction to Metal Debris” OR “Adverse reactions to metal debris” OR Revision OR loosening).
AND SU,TI,AB((thumb) NEAR/3 (CMC* OR carpometacarpal)) OR trapeziometacarpal OR TMCJ).
AND SU,TI,AB(implant* OR Arthroplasty OR “Joint replacement” OR prosthesis).
AND (pd(> 20,010,101)).
AND at.exact(“Article” OR “Government & Official Document” OR “Case Study” OR “Technical Report” OR “Report” OR “Literature Review”).
AND la.exact(“English”).
Appendix 2
See Table
5.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mangan, F., Spece, H., Weiss, AP.C. et al. A review of wear debris in thumb base joint implants. Eur J Orthop Surg Traumatol 34, 251–269 (2024). https://doi.org/10.1007/s00590-023-03622-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03622-x