Abstract
Background
Periprosthetic joint infection (PJI) of the knee represents a severe complication after 1.5% to 2% of primary total knee replacement. Although two-stage revision was considered the gold-standard treatment for PJI of the knee, in the last decades, more studies reported the outcomes of one-stage revisions. This systematic review aims to assess reinfection rate, infection-free survival after reoperation for recurrent infection, and the microorganisms involved in both primary and recurrent infection.
Material and methods
A systematic review of all studies reporting the outcome of one-stage revision for PJI of the knee up to September 2022, according to PRISMA criteria and AMSTAR2 guidelines, was performed. Patient demographics, clinical, surgical, and postoperative data were recorded. PROSPERO ID: CRD42022362767.
Results
Eighteen studies with a total of 881 one-stage revisions for PJI of the knee were analyzed. A reinfection rate of 12.2% after an average follow-up of 57.6 months was reported. The most frequent causative microorganism were gram-positive bacteria (71.1%), gram-negative bacteria (7.1%), and polymicrobial infections (8%). The average postoperative knee society score was 81.5, and the average postoperative knee function score was 74.2. The infection-free survival after treatment for recurrent infection was 92.1%. The causative microorganisms at reinfections differed significantly from the primary infection (gram-positive 44.4%, gram-negative 11.1%).
Conclusion
Patients who underwent a one-stage revision for PJI of the knee showed a reinfection rate lower or comparable to other surgical treatments as two-stage or DAIR (debridement, antibiotics, and implant retention). Reoperation for reinfection demonstrates a lower success compared to one-stage revision. Moreover, microbiology differs between primary infection and recurrent infection.
Level of evidence Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee periprosthetic joint infection (PJI) is a severe complication that occurs in 1.5–2% of cases after primary total knee replacement (TKR) [1,2,3,4,5]. Although thorough diagnosis remains the cornerstone of PJI management, surgical planning and accurate adherence to treatment principles are essential [6]. Different surgical strategies may be adopted, such as debridement, antibiotics, implant retention (DAIR), and replacement arthroplasty in one or two stages. Furthermore, salvage options for patients with multiple treatment failures, including knee arthrodesis or above-knee amputation (AKA), should be considered [7, 8].
In recent decades, two-stage revision, based on all prosthetic implants’ removal and articular spacer implantation, has been considered the gold-standard treatment for knee PJI [9]. This procedure allows both local antibiotics administration in a concentration above the minimum effective concentration for approximately two weeks and adequate soft tissue tension during the interval period. First introduced in the early 1980s by John Insall, it should provide a higher eradication rate than other surgical solutions [10,11,12]. However, two-stage revision is associated with longer hospitalization, higher costs, and poor quality of life during the interval period [13]. Furthermore, there is no high-level evidence demonstrating that this technique has a higher success rate than the one-stage procedure [14].
One-stage revision has become increasingly popular recently and should be considered a viable option for chronic PJI treatment in a selected patient group [9]. This surgical procedure presents potential advantages such as reduced morbidity and mortality, hospital length and related costs, and improved quality of life while providing an optimal infection eradication rate [15]. Identifying a known sensitivities microorganism is mandatory; however, conditions like culture-negative PJI or the presence of systemic sepsis signs discourage one-stage revision indication [15, 16].
This systematic review aims to analyze the reinfection rate, survivorship after reoperation for recurrent infection, and the microorganisms involved in both index and recurrent infection in patients undergoing one-stage revision for knee PJI to assist orthopedics in daily practice PJI management.
Materials and methods
Research question
A systematic review of the current literature was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and a Measurement Tool to Assess Systematic Reviews (AMSTAR2) guidelines [17]. Medline, Cochrane Library, EMBASE, Scopus, and Web of Science databases were systematically reviewed until September 1, 2022. The following keywords were used in association with the Boolean AND/OR operator to identify relevant studies on one-stage revision TKA: “one-stage”; “single-stage”; “periprosthetic joint infection”; “PJI”; “total knee arthroplasty”; “TKA”; “total knee replacement”; “TKR.”
Inclusion and exclusion criteria
The inclusion criteria of the studies analyzed were “articles with patients treated with one-stage revision for treatment of knee PJI; with at least ten patients, a minimum follow-up of one year, reporting infection-free survival for one-stage revision; and studies written in English.” “Case reports, biochemical and in vitro studies, reviews, editorials, book chapters, or instructional courses were excluded from the systematic review.”
Methodological quality assessment
Each article’s levels of evidence (LoE) was recorded using the Oxford Centre for Evidence-Based Medicine criteria [18]. The methodological quality of the studies included was evaluated through the methodological index for non-randomized studies (MINORS) criteria [19,20,21]. The MINORS score ranges from 0 to 18 for non-comparative studies and 0 to 24 for comparative studies, with a higher score reflecting higher quality. The present systematic review was registered in PROSPERO, ID: CRD42022362767.
Search strategy and study screening
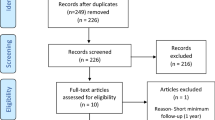
A total of 632 studies were identified through the databases used. After excluding duplicates, 343 studies were included, and after evaluation of the title and abstract, 21 studies were analyzed. After assessing the eligibility of the full-text articles according to the inclusion and exclusion criteria and screening the bibliography of each article to find additional relevant publications, 18 clinical studies were selected and included in this systematic review [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. The PRISMA flowchart with the research strategy is shown in Fig. 1 [17].
Data extraction
Two reviewers (GC and LB) collected data from the selected studies and inserted them into a standard template. The following study characteristics were extracted: author and year of publication, study characteristics and patient demographics, a summary of reinfection rate after one-stage revision, causative microorganism at the one-stage revision, causative microorganism at reinfection, differences in microbiology between one-stage revision and reinfection. When a study included total hip and knee results of one-stage revision, only data about TKA were collected. When a study included data on different surgical procedures such as DAIR or two-stage revision, only results about one-stage revision were collected.
Statistical analysis
Statistical analysis was performed with R software, version 4.0.5 (2020; R Core Team, Vienna, Austria). Descriptive statistical analysis was performed for all data extracted by the included studies. Mean values with a measure of variability as standard deviation (SD) or range (minimum–maximum) were calculated for continuous variables. The absolute number, frequency distribution, and Chi-square test were used to analyze categorical variables. A p value < 0.05 was considered statistically significant.
Results
Study characteristics
Eighteen clinical studies [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39] were included in the final analysis (Fig. 1) [17]. The LoE and MINORS values for each study are listed in Table 1. Initially, 991 one-stage revisions for knee PJI were included in the analysis. After excluding 104 (10.5%) one-stage revisions due to missing data and patients lost to follow-up, 887 one-stage revisions with a mean age of 67.9 ± 2.9 years were included in the final analysis. The mean follow-up was 57.6 ± 31.8 months. Seventeen studies [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32, 34,35,36,37,38,39] reported sex data, and 43.3% were men, and 56.7% were women. The demographic data of the included studies are listed in Table 1.
Reinfection after one-stage revision
All eighteen studies reported overall failure due to infection after one-stage revision [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. Reinfection after one-stage revision occurred in 108 cases (12.2%). Survivorship after the one-stage revision was 87.8% (779 patients were infection-free at the last follow-up). The mean time between one-stage revision and reinfection was 26.7 ± 14.4 months as reported by ten studies [22,23,24, 27, 32, 33, 35, 37,38,39]. Thirteen studies [22,23,24, 26,27,28,29,30, 32, 35, 37,38,39] reported the treatment performed for reinfection. A repeated one-stage revision was the most frequent intervention, followed by DAIR, long-term antibiotic therapy, knee arthrodesis, AKA, and two-stage revision. The survivorship after treatment for reinfection considering failure also patients who underwent AKA or knee arthrodesis was 92.1% (817 patients). Data on reinfection after one-stage revision, success, and failure rate of treatments for reinfections, and survivorship are listed in Table 2.
Clinical outcomes after one-stage revision
Seven studies reported the mean postoperative range of motion (ROM) [22, 24, 26, 29, 32, 33, 36]. Six studies reported the mean preoperative and postoperative knee society score (KSS) knee score [23, 24, 26, 28, 29, 36]. One study reported a mean preoperative KSS function score [24], whereas the mean postoperative KSS function score was reported by three studies [24, 26, 29]. Two studies reported the mean preoperative Oxford knee score (OKS) [27, 37], and six studies reported the mean postoperative OKS [24, 25, 27, 29, 33, 37]. Three studies reported the mean preoperative Hospital for Special Surgery (HSS) score [30, 32, 35], and three studies reported the mean postoperative HSS [30, 32, 35]. For all the clinical scores, there was a statistically significant improvement (p < 0.05) between the preoperative and postoperative mean scores (Table 3).
Microbiology
Sixteen studies reported data on the causative microorganism at the one-stage revision [22,23,24, 26,27,28,29,30,31,32,33, 35, 39]. Gram-positive bacteria caused infection in 71.1% of cases, gram-negative bacteria in 7.5% of cases, and a polymicrobial infection in 8% of cases. No bacterial growth was reported in 9% of cases. Fungal infection occurred in 0.8% of cases. Table 4 shows detailed information on the causative microorganisms at the time of the one-stage revision.
Thirteen studies reported data on the causative microorganism at reinfection [22, 23, 26,27,28, 30, 32, 33, 35,36,37,38,– 39]. The causative microorganisms were gram-positive in 44.4% of cases, gram-negative in 11.2%, and other microorganisms in 44.4%. Table 5 shows detailed information on the causative microorganisms at the time of the reinfection.
In the one-stage revisions, 67.8% “favorable” microorganisms and 32.2% “aggressive” microorganisms were identified. Methicillin-resistant Staphylococcus Aureus (MRSA), methicillin-resistant Staphylococcus Epidermidis (MRSE), Enterococcus species, Pseudomonas aeruginosa, Fungal, polymicrobial infection, and culture-negative PJI were considered “aggressive” microorganisms. Reinfection was caused by “favorable” microorganisms in 44.4% of cases and by an “aggressive” microorganism in 55.6% of cases. Gram-positive infections were significantly higher at one-stage revision than at reinfection (71.1% and 44.4%, respectively, p < 0.001). Among gram-positive infections, there was a significant difference for Staphylococcus Epidermidis (13.4% at one-stage revision and 4.8% at reinfection, p = 0.047) and coagulase-negative staphylococci (CoNS) (12.6% at one-stage revision and 3.2% at reinfection, p = 0.026). No statistical differences were found between one-stage revision and reinfection for the overall gram-negative infections (7.5% and 11.1%, respectively, p = 0.308). Analyzing the individual gram-negatives showed that infections caused by Pseudomonas Aeruginosa (1% at one-stage revision and 4.8% at reinfection, p = 0.008) and Escherichia Coli (1% at one-stage revision and 4.8% at reinfection, p = 0.008) were more frequent at reinfection with a statistically significant difference (Table 6).
Discussion
PJI represents one of the most challenging complications after TKR [1, 2]. For many years, the two-stage revision was considered the gold-standard procedure; however, recently, single-stage treatment has gained popularity [8, 9]. The main result of this study is that one-stage revision, in line with data reported by previous studies, provides an equivalent or slightly lower reinfection rate than two-stage revision [40, 41]. Furthermore, the success rate from reinfection reoperation was lower than the first revision surgery for an infection. Finally, it was demonstrated that causative microorganisms differ significantly between the first one-stage revision and infection recurrence.
Infection recurrence
The reinfection recurrence rate reported after the one-stage revision was 12.2% at a mean time of 26.7 months, ranging from 0 [28, 36] to 37.5% [38]. This result is comparable to the reinfection rate described in the literature with two-stage revision, which varied between 10 and 30% [40]. Rossman et al. [38] reported the highest reinfection rate among the studies included in this systematic review. The authors observed reinfection in 15 of 40 enterococcal-related PJIs. Castellani et al. [31] reported similar data with a reinfection rate of 50% in enterococcal-related PJIs in patients treated with one- or two-stage revision. Citak et al. [42] highlighted enterococci, being difficult-to-treat antibiotic-resistant pathogens, as an independent risk factor for reinfection in PJI, regardless of the surgical treatment performed. Antibiotic-resistant bacteria were one of the main topics of the second international meeting on PJI, whose guidelines did not recommend one-stage revision in case of systemic signs of infection, an infection caused by a resistant microorganism, culture-negative infection, and insufficient soft tissue coverage [43]. The higher revision rates described in some of the studies included in this systematic review [32, 38, 42] may be explained by a one-stage revision approach even in the presence of the above-mentioned risk factors [43].
Reoperations
In this systematic review, treatments performed for infection recurrence (71 PJIs) were examined. No infection at final follow-up was found in 92.1% of patients. A further one-stage revision was the most frequent treatment for reinfection. It was performed on 26 patients with a success rate of 76.9%. DAIR was reported in 16 cases, with a success rate of 93.8%. Lower results were observed in the 11 patients treated exclusively with suppressive antibiotic therapy and the two patients who underwent two-stage revision, with success rates of 45.5% and 50%, respectively. “Salvage procedures” were performed in 16 cases; eight patients underwent knee arthrodesis, while AKA was necessary in eight cases.
Microbiology
This study highlighted that the causative microorganisms at one-stage revision and reinfection were significantly different (Table 5). The incidence of gram-positive bacteria, especially Staphylococcus epidermidis and CoNS, decreased significantly from 71.1% at one-stage revision to 44.4% at reinfection. Gram-negative bacteria were more frequently in reinfection (11.1%) than in one-stage revision (7.5%), but not at a statistically significant rate, except for Pseudomonas Aeruginosa and Escherichia Coli, which both increased from 1 to 4.8%, respectively. Finally, polymicrobial, culture-negative, or fungal infections, often considered challenging PJI, had a statistically higher reinfection rate (Table 6). The results presented in this systematic review follow the data reported in the literature on the increased reinfection rate after surgical treatment of knee PJI caused by “aggressive” microorganisms [43,44,45]. Specifically, this study observed that infections caused by “aggressive” species had a statistically significant higher incidence of reinfection after one-stage revision [43,44,45].
PJI caused by resistant staphylococci, MRSA and MRSE, is considered a major therapeutic challenge with a high rate of recurrent infection. Mittal et al., in their series of 37 patients, reported reinfection in 24% of patients [46]. Salgado et al., in their retrospective study, observed a 50% reinfection rate in MRSA-related infections [47]. In this systematic review, PJI was caused by resistant staphylococci in 12.7% of patients. MRSA caused recurrent infection in four cases (6.3%) and MRSE in one case (1.6%). Generally, PJI caused by resistant staphylococci is treated with a two-stage revision, considering the higher chances of eradication of the infection due to the debridement of the first stage and the high concentration of local antibiotic released by the antibiotic from the cement spacer [48]. Although some authors have considered resistant staphylococcal infections a contraindication to single-stage revision [28, 36], the results of this paper suggest that one-stage revision could be performed with favorable results even in PJIs caused by resistant staphylococci. In this systematic review, only one study reported a complete series of patients affected by MRSA PJI [23]. All patients underwent a one-stage revision followed by intra-articular injection of antibiotic (500 mg Vancomycin) once or twice daily for six weeks without postoperative intravenous antibiotics. The authors reported a 94.4 percent success rate (17 of 18 patients). In the only case of failure, the patient underwent reoperation after five months with a large fragment of necrotic bone removal [23].
Several authors have considered fungal infection a contraindication for one-stage revision suggesting two-stage revision as a gold-standard procedure [49,50,51]. In a recent systematic review of the literature [49] that collected data from 45 fungal knees PJIs, it was demonstrated that the causative microorganism responsible for about 80 percent of the infections was the Candida species. About 50 percent of the patients had risk factors such as advanced immunodepression, prolonged antibiotic use, autoimmune disease, or drug abuse. After a mean follow-up of 37.4 months, the authors reported recurrent bacterial infections in five cases. Instead, six patients required AKA. In another six cases, no established information on therapeutic outcomes was reported [49]. In this systematic review, seven patients with fungal PJI underwent one-stage revision with a failure rate of 42.8%. Fungal PJI should always be suspected in case of infection recurrence. This paper reported fungal PJI in five cases after a one-stage revision procedure.
Polymicrobial infections have been considered an independent risk factor for infection recurrence following several surgical treatments for PJI [16, 52, 53]. Razii et al. reported that polymicrobial infections were associated with increased reinfection [37]. Similarly, Massin et al. observed a higher recurrent infection rate in patients with polymicrobial infections caused by gram-negative bacteria [29]. Two of the studies included in this systematic review reported a higher risk of reinfection in polymicrobial infections [27, 37]. Several authors agreed that polymicrobial infection is a contraindication for one-stage revision, suggesting that other surgical treatments, such as two-stage revisions, are more suitable for this clinical condition [28, 33, 39].
Limitations
This systematic review has some limitations that need to be analyzed. First, only English studies were considered, which may exclude any relevant studies published in other languages. Second, the LoE of the included papers is poor, and there are no studies with LoE I or II. Third, there is significant variability among studies regarding PROMs and outcome measures evaluated. Finally, the different papers have various inclusion criteria for patients eligible for one-stage revision, and the patients’ populations are difficult to compare.
Conclusions
This systematic review reported that, in selected patients, the incidence of recurrent infection after one-stage revision is comparable to or lower than that of other surgical treatments such as two-stage revision and DAIR. Reoperation for recurrent infection demonstrated a lower success rate than the first one-stage procedure. In addition, microbiology is significantly different between one-stage revision and reinfection. Higher rates of “aggressive” microorganisms have been observed in the latter. Finally, several risk factors should be evaluated before performing a one-stage revision. In this systematic review, it was reported that in the presence of previous septic events and aggressive and polymicrobial infections, the risk of reinfection is higher, and other surgical strategies, such as two-stage revisions, should be considered.
Data availability
Dataset analyzed in this study is available from the corresponding author on reasonable request.
References
Lamagni T (2014) Epidemiology and burden of prosthetic joint infections. J Antimicrob Chemother 69(Suppl 1):i5-10
Kim HS, Park JW, Moon SY, Lee YK, Ha YC, Koo KH (2020) Current and future burden of periprosthetic joint infection from national claim database. J Korean Med Sci 35(49):e410
McMaster Arthroplasty Collaborative (MAC) (2022) Incidence and predictors of prosthetic joint infection following primary total knee arthroplasty: a 15-year population-based cohort study. J Arthroplasty 37(2):367-372.e1
Giustra F, Bistolfi A, Bosco F, Fresia N, Sabatini L, Berchialla P et al (2022) Highly cross-linked polyethylene versus conventional polyethylene in primary total knee arthroplasty: comparable clinical and radiological results at a 10-year follow-up. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07226-6
Giustra F, Bosco F, Cacciola G, Risitano S, Capella M, Bistolfi A et al (2022) No significant differences in clinical and radiographic outcomes between PCL retained or sacrificed kinematic aligned medial pivot total knee arthroplasty in varus knee. J Clin Med 11(21):6569
Aggarwal VK, Rasouli MR, Parvizi J (2013) Periprosthetic joint infection: Current concept. Indian J Orthop 47(1):10–17
Gomez MM, Tan TL, Manrique J, Deirmengian GK, Parvizi J (2015) The fate of spacers in the treatment of periprosthetic joint infection. J Bone Joint Surg Am 97(18):1495–1502
Grosso MJ, Kozaily E, Cacciola G, Parvizi J (2021) Characterizing femoral and acetabular bone loss in two-stage revision total hip arthroplasty for infection. J Arthroplasty 36(1):311–316
Lazic I, Scheele C, Pohlig F, von Eisenhart-Rothe R, Suren C (2021) Treatment options in PJI - is two-stage still gold standard? J Orthop 23:180–184
Insall JN, Thompson FM, Brause BD (1983) Two-stage reimplantation for the salvage of infected total knee arthroplasty. JBJS 65(8):1087–1098
Craig A, King SW, van Duren BH, Veysi VT, Jain S, Palan J (2022) Articular spacers in two-stage revision arthroplasty for prosthetic joint infection of the hip and the knee. EFORT Open Rev 7(2):137–152
De Martino I, Mancino F, Cacciola G, Di Matteo V, Maccauro G (2022) Local delivery of antibiotic and antiseptic. In: Longo UG, Budhiparama NC, Lustig S, Becker R, Espregueira-Mendes J (eds) Infection in Knee Replacement. Springer, Cham
Maden C, Jaibaji M, Konan S, Zagra L, Borella M, Harvey A et al (2021) The outcomes of surgical management of failed two-stage revision knee arthroplasty. Acta Biomed 92(3):e2021197
Gehrke T, Alijanipour P, Parvizi J (2015) The management of an infected total knee arthroplasty. Bone Joint J 97(10 Supp A):20–29
Bialecki J, Bucsi L, Fernando N, Foguet P, Guo S, Haddad F et al (2019) Hip and knee section, treatment, one stage exchange: proceedings of international consensus on orthopedic infections. J Arthroplasty 34(2S):S421–S426
Bakhtiari IG, Vles G, Busch SM, Frommelt L, Gehrke T, Salber J et al (2022) Septic failure after one-stage exchange for prosthetic joint infection of the hip: microbiological implications. J Arthroplasty 37(2):373–378
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160
Burns PB, Rohrich RJ, Chung KC (2011) The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg 128(1):305–310
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Le N, Blackman B, Zakharia A, Cohen D, de Sa D (2022) MPFL repair after acute first-time patellar dislocation results in lower redislocation rates and less knee pain compared to rehabilitation: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07222-w
Risitano S, Cacciola G, Sabatini L, Capella M, Bosco F, Giustra F et al (2022) Restricted kinematic alignment in primary total knee arthroplasty: a systematic review of radiographic and clinical data. J Orthop 33:37–43
Göksan SB, Freeman MA (1992) One-stage reimplantation for infected total knee arthroplasty. J Bone Joint Surg Br 74(1):78–82
Whiteside LA, Peppers M, Nayfeh TA, Roy ME (2011) Methicillin-resistant Staphylococcus aureus in TKA treated with revision and direct intra-articular antibiotic infusion. Clin Orthop Relat Res 469(1):26–33
Singer J, Merz A, Frommelt L, Fink B (2012) High rate of infection control with one-stage revision of septic knee prostheses excluding MRSA and MRSE. Clin Orthop Relat Res 470(5):1461–1471
Baker P, Petheram TG, Kurtz S, Konttinen YT, Gregg P, Deehan D (2013) Patient reported outcome measures after revision of the infected TKR: comparison of single versus two-stage revision. Knee Surg Sports Traumatol Arthrosc 21(12):2713–2720
Jenny JY, Barbe B, Gaudias J, Boeri C, Argenson JN (2013) High infection control rate and function after routine one-stage exchange for chronically infected TKA. Clin Orthop Relat Res 471(1):238–243
Tibrewal S, Malagelada F, Jeyaseelan L, Posch F, Scott G (2014) Single-stage revision for the infected total knee replacement: results from a single centre. Bone Joint J 96(6):759–764
Haddad FS, Sukeik M, Alazzawi S (2015) Is single-stage revision according to a strict protocol effective in treatment of chronic knee arthroplasty infections? Clin Orthop Relat Res 473(1):8–14
Massin P, Delory T, Lhotellier L, Pasquier G, Roche O, Cazenave A et al (2016) Infection recurrence factors in one- and two-stage total knee prosthesis exchanges. Knee Surg Sports Traumatol Arthrosc 24(10):3131–3139
Zahar A, Kendoff DO, Klatte TO, Gehrke TA (2016) Can good infection control be obtained in one-stage exchange of the infected TKA to a rotating hinge design? 10-year results. Clin Orthop Relat Res 474(1):81–87
Castellani L, Daneman N, Mubareka S, Jenkinson R (2017) Factors associated with choice and success of one- versus two-stage revision arthroplasty for infected hip and knee prostheses. HSS J 13(3):224–231
Abdelaziz H, Biewald P, Anastasiadis Z, Haasper C, Gehrke T, Hawi N et al (2020) Midterm results after tantalum cones in 1-stage knee exchange for periprosthetic joint infection: a single-center study. J Arthroplasty 35(4):1084–1089
Holland G, Brown G, Goudie S, Brenkel I, Walmsley PJ (2021) Results of using a “2-in-1” single-stage revision total knee arthroplasty for infection with associated bone loss: prospective 2-year follow-up. J Knee Surg 34(5):526–532
Klemt C, Tirumala V, Oganesyan R, Xiong L, van den Kieboom J, Kwon YM (2021) Single-stage revision of the infected total knee arthroplasty is associated with improved functional outcomes: a propensity score-matched cohort study. J Arthroplasty 36(1):298–304
Ji B, Li G, Zhang X, Wang Y, Mu W, Cao L (2021) Midterm survival of a varus-valgus constrained implant following one-stage revision for periprosthetic joint infection: a single-center study. J Knee Surg. https://doi.org/10.1055/s-0041-1731739
Pellegrini A, Meani E, Macchi V, Legnani C (2021) One-stage revision surgery provides infection eradication and satisfying outcomes for infected knee arthroplasty in selected patients. Expert Rev Anti Infect Ther 19(7):945–948
Razii N, Clutton JM, Kakar R, Morgan-Jones R (2021) Single-stage revision for the infected total knee arthroplasty: the cardiff experience. Bone Jt Open 2(5):305–313
Rossmann M, Minde T, Citak M, Gehrke T, Sandiford NA, Klatte TO et al (2021) High rate of reinfection with new bacteria following one-stage exchange for enterococcal periprosthetic infection of the knee: a single-center study. J Arthroplasty 36(2):711–716
Tuecking LR, Silligmann J, Savov P, Omar M, Windhagen H, Ettinger M (2021) Detailed revision risk analysis after single- vs two-stage revision total knee arthroplasty in periprosthetic joint infection: a retrospective tertiary center analysis. Antibiotics 10(10):1177
Goud AL, Harlianto NI, Ezzafzafi S, Veltman ES, Bekkers JEJ, van der Wal BCH (2021) Reinfection rates after one- and two-stage revision surgery for hip and knee arthroplasty: a systematic review and meta-analysis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04190-7
Kunutsor SK, Whitehouse MR, Lenguerrand E, Blom AW, Beswick AD; INFORM Team (2016) Re-infection outcomes following one- and two-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PLoS ONE 11(3):e0151537
Citak M, Friedenstab J, Abdelaziz H, Suero EM, Zahar A, Salber J et al (2019) Risk factors for failure after 1-stage exchange total knee arthroplasty in the management of periprosthetic joint infection. J Bone Joint Surg Am 101(12):1061–1069
Aalirezaie A, Bauer TW, Fayaz H, Griffin W, Higuera CA, Krenn V et al (2019) Hip and knee section, diagnosis, reimplantation: proceedings of international consensus on orthopedic infections. J Arthroplasty 34(2):369–379
Chen JL, Huang TY, Hsu WB, Lee CW, Chiang YC, Chang PJ et al (2022) Characterization of methicillin-resistant staphylococcus aureus isolates from periprosthetic joint infections. Pathogens 11(7):719
Santoso A, Yoon TR, Park KS, Anwar IB, Utomo P, Soetjahjo B et al (2020) The results of two-stage revision for methicillin-resistant periprosthetic joint infection (PJI) of the hip. Malays Orthop J 14(1):18–23
Mittal Y, Fehring TK, Hanssen A, Marculescu C, Odum SM, Osmon D (2007) Two-stage reimplantation for periprosthetic knee infection involving resistant organisms. J Bone Joint Surg Am 89(6):1227–1231
Salgado CD, Dash S, Cantey JR, Marculescu CE (2007) Higher risk of failure of methicillin-resistant staphylococcus aureus prosthetic joint infections. Clin Orthop Relat Res 461:48–53
Cacciola G, De Meo F, Cavaliere P (2018) Mechanical and elution properties of G3 low viscosity bone cement loaded up to three antibiotics. J Orthop 15(4):1004–1007
Jakobs O, Schoof B, Klatte TO, Schmidl S, Fensky F, Guenther D et al (2015) Fungal periprosthetic joint infection in total knee arthroplasty: a systematic review. Orthop Rev (Pavia) 7(1):5623
Gross CE, Della Valle CJ, Rex JC, Traven SA, Durante EC (2021) Fungal periprosthetic joint infection: a review of demographics and management. J Arthroplasty 36(5):1758–1764
Schoof B, Jakobs O, Schmidl S, Klatte TO, Frommelt L, Gehrke T et al (2015) Fungal periprosthetic joint infection of the hip: a systematic review. Orthop Rev (Pavia) 7(1):5748
Marculescu CE, Cantey JR (2008) Polymicrobial prosthetic joint infections: risk factors and outcome. Clin Orthop Relat Res 466(6):1397–1404
Valenzuela MM, Averkamp BJ, Odum SM, Rowe TM, Fehring TK (2022) Polymicrobial colonization of prosthetic joint infections treated with open wound management. J Arthroplasty 37(7S):S653–S656
Acknowledgements
None.
Funding
Open access funding provided by Università degli Studi di Torino within the CRUI-CARE Agreement. No funding has been received for this study.
Author information
Authors and Affiliations
Contributions
GC, FB, FG, and LB have contributed substantially to conception and design, data acquisition, analysis, and interpretation. They have been involved in drafting the manuscript and revising it critically for important intellectual content, given final approval of the version to be published. They agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. DV, SR, MC, and LS have contributed substantially to the data analysis, interpretation, and manuscript drafting. PC and AM have made substantial contributions to concept and design the manuscript and revising it critically for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest for this study to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All patients were informed about the study and consented to participate.
Informed consent
All patients were informed about the study and consented to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bosco, F., Cacciola, G., Giustra, F. et al. Characterizing recurrent infections after one-stage revision for periprosthetic joint infection of the knee: a systematic review of the literature. Eur J Orthop Surg Traumatol 33, 2703–2715 (2023). https://doi.org/10.1007/s00590-023-03480-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03480-7