Abstract
Purpose
The purpose of this study is to report and compare outcome data of both primary and revision cases using a rotating hinge knee (RHK) implant.
Methods
This study retrospectively analyzed 63 cases (19 primary, 44 revisions) at a mean follow-up of 34 ± 8 months after RHK implantation. Outcome parameters were stability, range of motion (ROM), loosening, Hospital of Special Surgery Score (HSS), Knee Society Score (KSS), Oxford Knee Score (OKS), EQ-5D-3L, and Visual Analog Scale (VAS) for overall function. Revision rates and implant survival are reported.
Results
Eleven percent showed medio-lateral instability < 5 mm, a mean ROM of 115° ± 17° and radiologic loosening occurred in 8% (2% symptomatic). PROMS showed the following results: HSS 79 ± 18, KSS 78 ± 27, OKS 26 ± 10, EQ-5D index 0.741 ± 0.233 and VAS 70 ± 20. Primary cases revealed better outcomes in HHS (p = .035) and OKS (p = 0.047). KSS, EQ-5D index and VAS did not differ between primary and revision cases (p = 0.070; p = 0.377; p = 0.117). Revision rate was 6.3% with an implant survival of 96.8%.
Conclusions
RHK arthroplasty can be performed with good clinical outcome and low revision rate in revision and complex primary cases. RHK is an option in cases where standard arthroplasty and even implants with a higher degree of constraint have reached their limits.
Level of Evidence
Level III, retrospective cohort study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hinged or highly constrained knee arthroplasty is a valuable treatment option for surgical salvage in situations where a sufficient joint-stability cannot be accomplished with conventional, unconstrained implants.
Especially in revision surgery with ligamentous laxity and instability, and/or excessive bone loss, or extensor mechanism impairment an increased level of implant constraint may be required. However, this implant type is also being used in primary TKA, where it may offer a viable surgical alternative in cases of severe degenerative and inflammatory arthritis with extreme deformity, bone loss and/or ligamentous insufficiency. [2, 22]
Rotating hinge implants (RHI) were introduced in the late 1970s with the aim to prevent the complications (mainly mechanical failure) of fixed hinge implants [21, 24]. The most significant improvement in the design of these prostheses is the ability to rotate, the introduction of metal wedge augmentation and modular fluted stems with variable offset, achieving better alignment and press-fit fixation. Due to these mechanical improvements, complications of hinged TKA decreased dramatically [14]. Nevertheless, heterogeneous results and frequency of complications have been reported [14, 23]. A short-term (1–5 years) survival of up to 92% and mid-term (6–10 years) survival of up to 82% has been shown. The most common reasons for revision surgery were infection, aseptic loosening and peri-prosthetic fractures [1, 7, 8]. When used in revision surgery, the main indications for an RHI were aseptic loosening of prior TKA, bone loss, ligamentous instability, peri-prosthetic fractures, and infection. [24] When used in primary cases the main indications where ligamentous insufficiency, bone loss, and gross joint destruction [12].
Due to the heterogenty of outcome data regarding this kind of implant the objective of the current study is to report the indications, clinical outcomes, and survival associated with the use of RHI for primary and revision cases.
Material and methods
This study represents a single-center retrospective study assessing the outcome after implantation of a Rotating Hinge Knee (RHK) arthroplasty (GMK Hinge, Medacta international, Castel San Pietro, Switzerland) performed at our institution between December 2015 and August 2018. The cantonal ethics committee approved the study.
Inclusion criteria were primary and revision total knee arthroplasties with the use of the above-mentioned implant, performed for any reason with available outcome scores at a follow-up of a minimum of two years. [5, 6, 10] Exclusion criteria were the usage of other implants, refusal of participation and incomplete final follow-up data.
In total, 63 RHKs (right 38, left 25) in 63 patients (37 female, 26 male) were evaluated. The mean age at the index-surgery (RHK implantation) was 69 ± 9 years. The mean follow-up was 34 ± 8 months. Complete demographic data is given in Table 2.
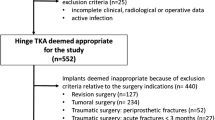
Nineteen RHKs were implanted as primary TKA and 44 in revision cases. A flowchart illustrating the study cohort is provided in Fig. 1. Prior to revision surgery a primary TKA (n = 31), a condylar constrained TKA (n = 9), a hinged prosthesis (n = 3), and a uni-condylar prosthesis (n = 1) had been used. In the primary group in 17 cases, a complete follow-up with clinical and radiological evaluation as well as PROMs and analysis of the medical history was possible. Two patients did not present at our outpatient clinic and therefore only medical history and PROMs could be obtained. In the revision group, 37 cases were available for complete and seven for partial follow-up (without clinical and radiological assessment).
The radiologic assessment consisted of an antero-posterior (a.p.) and lateral radiograph of the knee as well as a standing long leg radiograph. Clinical examination focused on the evaluation of instability and range of motion. Moreover, Hospital of Special Surgery Score (HSS), Knee Society Score (KSS), Oxford Knee Score (OKS), EQ-5D-3L, and Visual Analog Scale (VAS) for overall function and satisfaction were raised. The outcome ranges of the used scores are reported in Table 1.
The radiographs were analyzed for signs of implant loosening defined as a gap of more than 2 mm in the bone-cement- or bone-implant-interface [16]. The anatomical axis was measured on the long leg radiographs. The medical history, including the surgical report were evaluated for the number of previous surgeries, the decision making for a RHK and subsequent revisions. Furthermore, demographic data including patient age, ASA-Score, height, and body weight were collected.
Statistical analysis
Statistical analysis was conducted in SPSS (IBM SPSS Statistics, Version 25 for Windows) and STATA 16.1 (StataCorp, The College Station, Texas, USA) with a significance level of p < 0.05. The Kolmogorov–Smirnov test was used to check for normal distribution of data. Data is reported as mean ± standard deviation (SD). An unpaired t-test was used to compare the outcome in primary and revision cases. All variables (BMI and sex) that showed at least a very weak evidence (p < 0.2) for an association with the exposure (primary or revision arthroplasty), were included in a multivariable linear regression analyzed for the different outcome parameters. No adjustment of multiple testing was performed. Kaplan–Meier survival graphs were calculated for the endpoints revision and implant survival.
Results
The main indications for revision that lead to the use of a RHK were infection (n = 16) and aseptic loosening (n = 15) followed by instability (n = 8), painful TKA without a specific reason (n = 4) and polyethylene wear (n = 1).
The main reasons to use the RHK as a primary implant were severe medial and/or lateral ligamentous instability (n = 15) and fixed valgus deformity over 20 degrees (n = 12) followed by extension deficit over 20 degrees (n = 7), rheumatoid arthritis with severe bone destruction (n = 5), and posttraumatic bone loss (n = 2). All patients in this group possessed two or more of the above-mentioned pathologies.
At the final follow-up limited medio-lateral instability of less than 5 mm was detected in 7 cases (13%). In the other 47 cases (87%) no instability was present. An antero-posterior instability was not detected in this cohort. The mean range of motion was 115 ± 17 degrees.
PROMS showed satisfactory results in the upper third of each scale and are displayed in Table 2.
In 53 cases a mean anatomical valgus of 6 ± 2 degrees was measured, in one case a varus malalignment of 7 degrees was present. In five cases a radiolucent line of at least 2 mm width suspicious for implant loosening was detected in the bone-cement or bone-implant interface of tibia and/or femur. Four of those patients were without clinical symptoms. One patient experienced pain during walking but refused to undergo revision for aseptic loosening.
Subgroup analysis comparing the outcome of RHK implantation in primary and revision cases, revealed a significantly better outcome in the primary group with regards to ROM (p = 0.002), HSS (p = 0.035), KSS expectation and satisfaction score (p = 0.004), KSS functional activity score (p = 0.023), and OKS (p = 0.047). KSS objective score (p = 0.070), VAS for overall function and satisfaction (p = 0.117), and the EQ-5D index (p = 0.377) did not show significant differences. After including gender and BMI as possible confounding factors via multivariate linear regression, significant differences between primary and revision group could only be detected for ROM (p = 0.004), KSS expectation and satisfaction scores (p = 0.030) and the KSS satisfaction sub-score (p = 0.035). The results are as well summarized and reported in Tables 2 and 3.
At the final follow-up four cases had been revised (6.3%) and in two cases (3.2%) the implant had been removed, resulting in an implant survival of 96.8% at a mean follow-up of 34 months. The Kaplan–Meier survival graphs for the endpoints revision and implant removal are displayed in Figs. 2 and 3. One infection was considered chronic and was treated with a two-stage-exchange. In the other three cases a debridement, change of the mobile parts and administration of antibiotics (DAIR procedure) was performed due to acute infection. The mean time to revision was 6 ± 5 months. The closer analysis of these cases revealed one early infection (three weeks after implantation due to wound healing problems) in a primary case that was treated successfully with DAIR. The other three cases were in the revision group and the initial RHK implantation had already been for infection. Two of them were treated with DAIR and one with a two-stage-exchange. One prosthesis of the latter group that received DAIR in the first place had to undergo one-stage-revision three months later due to persistent infection.
Discussion
Rotating hinge knees are important implants to address anatomic deficiencies like ligamentous instability, bone loss, and gross deformities that cannot be treated with standard TKA or even higher constrained but not hinged implant. The primary application of rotating hinge implants are complex TKA revision surgeries. [14, 25] RHKs are associated with a higher complication rate as compared to standard implants but the results improved during the last 20 years [18]. These implants are necessary and valuable tools in cases where standard implants reach their limits, but the indication should be strict due to higher complication and revision rates. The most frequent conditions leading to the implantation of a RHK in this study were infection and aseptic loosening, followed by ligamentous instability. This is in accordance with the available literature. [4, 8, 25]
The reason for using such implants in primary cases is the complex nature of these cases including severe bone loss, high grade deformities, ligamentous and muscular insufficiency associated with an increased risk of a less favorable outcome [21]. Another proposed indication is a intraarticular fracture in the elderly patient [19]. First generation hinged implants showed high rates of mechanical complications due to their high degree of constraint. [21] Even current generation RHKs such as the one used in this cohort were shown to be associated with high revision rates of 10–20% during the first 2 years when used in revision and complex primary cases. [7, 8, 22, 23] There is an ongoing debate on, whether RHK should be used in complex primary cases. [9] Recent studies showed acceptable survival rates of 80–90% after 7–10 years. [1, 15, 20] Therefore, there is a trend to a recommendation of this implants in complex primary situations. Nevertheless, age and indications might be important factors influencing survival. A recent study of 238 primary RKH with a minimum follow-up of 10 years, showed a survival of 94% in the age group over 60 years, while below that age only 77% survival could be reached. Moreover, the same study found a survival of 96% in varus knees and of 79% in valgus knees. The combination of age under 60 and valgus even worsened the survival to 64% [12]. These significant differences in survival rates should sensitize the surgeon to make patient selection for primary RHK very carefully. The average age of 68 years in our cohort may be one of the reasons for the good survival. A condylar constrained knee should be thought of as an alternative which has been reported to have significantly better outcomes compared to RHK [17].
Regarding clinical outcome, the here reported KSS score of 78 points shows slightly inferior outcome compared to primary standard TKA. A study of primary TKA with standard implants reported a KSS score of 92 points at a medium-term follow-up of 6.9 years [3]. Considering the longer follow-up, our values are slightly inferior, but still striking given the complex primary situation. Unfortunately, there is no exclusive study of complex cases treated with standard implants that would allow a direct comparison of our results. The mean outcome scores in a study reporting outcomes of a RHI with comparable follow-up were mean 81 points in the KSS objective score and 36 points in the KSS functional score. [4] The respective values in our study were 78 point in the KSS objective score, which is in the same range, while the KSS functional score was better in our cohort with 55 points.
Looking at the EQ-5D VAS level for overall function and satisfaction, no representative data was available for Switzerland. Therefore, we compared our data to the biggest neighbor country Germany, where a mean EQ-5D VAS score for overall function and satisfaction of 69 has been reported in the age group of 65–74 years [11]. This cohort data represents a cross section of society without elaborating on preexisting conditions or prior surgery. The value of 70 points given here corresponds to this representative reference population. When comparing primary and revision cases, the former showed significantly better results. Though after multivariate linear regression comparable functional outcomes in almost every (sub-) score were found.
After a mean follow-up of 3 years, implant survival rate was 97%, which is remarkable as 70% of the implants were used in revision cases. An exclusive study of one-stage revision using an RHK implant showed a revision rate of 40% at 8 years postoperatively with an implant survival of 80% at five years postoperative [13]. These markedly inferior results compared to our cohort highlight the in the literature available discrepancy regarding outcomes of RHK. In comparison, a study on 408 RHK reported a revision rate of 9.7% at two years postoperatively which better matches our revision rate of 6.3% at three years postoperative [4]. Table 4 gives an overview on outcome and survival rate of relevant studies reporting on rotating hinge implants.
Due to its retrospective character, our study has some limitations. First, preoperative PROMS were not available, making it impossible to evaluate disability before surgery or indicate improvement with surgery. This circumstance complicates the comparability of our data with the literature. Second, only 30% of the cases were primary cases, leading to statistical inaccuracy while comparing primary and revision cases. Third, the mean follow-up of 3 years is too short to give general recommendations for this type of implant especially when used as a primary implant. Forth, the different gender and BMI distribution were possible confounders with the result that only ROM and satisfaction were significantly lower in the revision group, while no differences could be detected for the other outcome parameters. Fifth, the number of cases was too small to further assess and compare the outcomes with regard to the indication leading to primary implantation or revision. However, there are only few studies available evaluating the survival and functional outcome of modern RHKs. The present study is the first one reporting the survival and outcome of this specific implant (GMK Hinge, Medacta international, Castel San Pietro, Switzerland). The case number is limited but within the range of other studies reporting on such rather rarely used implants [1]. The follow-up of other studies evaluating RHK ranges from 1 to 17 years with the majority of studies reporting short- to medium-term follow-up [14].
Conclusions
Rotating hinge knee arthroplasty can be performed with good clinical outcome and low complication rate in revision and complex primary cases. The latter is associated with even better mid-term results. RHK is an option in cases where standard arthroplasty and even implants with a higher degree of constraint have reached their limits. The increasing use of these implants will also provide a basis for reliable long-term outcome data.
References
Abdulkarim A, Keane A, Hu SY, Glen L, Murphy DJ (2019) Rotating-hinge knee prosthesis as a viable option in primary surgery: Literature review & meta-analysis. Orthop Traumatol Surg Res 105:1351–1359. https://doi.org/10.1016/j.otsr.2019.08.012
Baker P, Critchley R, Gray A, Jameson S, Gregg P, Port A et al (2014) Mid-term survival following primary hinged total knee replacement is good irrespective of the indication for surgery. Knee Surg Sports Traumatol Arthrosc 22:599–608. https://doi.org/10.1007/s00167-012-2305-y
Bingham JS, Salib CG, Hanssen AD, Taunton MJ, Pagnano MW, Abdel MP (2020) Clinical outcomes and survivorship of contemporary cementless primary total knee arthroplasties. JBJS Rev 8:e2000026. https://doi.org/10.2106/JBJS.RVW.20.00026
Cottino U, Abdel MP, Perry KI, Mara KC, Lewallen DG, Hanssen AD (2017) Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses. J Bone Joint Surg Am 99:324–330. https://doi.org/10.2106/JBJS.16.00307
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69. https://doi.org/10.1302/0301-620x.80b1.7859
Devlin NJ, Brooks R (2017) EQ-5D and the EuroQol group: past, present and future. Appl Health Econ Health Policy 15:127–137. https://doi.org/10.1007/s40258-017-0310-5
Gudnason A, Milbrink J, Hailer NP (2011) Implant survival and outcome after rotating-hinge total knee revision arthroplasty: a minimum 6-year follow-up. Arch Orthop Trauma Surg 131:1601–1607. https://doi.org/10.1007/s00402-011-1330-5
Hecker A, Putz HA, Wangler S, Klenke FM (2022) Survival, functional outcome and satisfaction of first revision total knee arthroplasty at a mean eleven-year follow-up. Eur J Orthop Surg Traumatol. Doi: https://doi.org/10.1007/s00590-022-03206-1
Hintze JV, Niemelainen M, Sintonen H, Nieminen J, Eskelinen A (2021) Good mid-term outcome of the rotating hinge knee in primary total knee arthroplasty—results of a single center cohort of 106 knees with a median follow-up of 6.3 years. Knee 28:273–281. https://doi.org/10.1016/j.knee.2020.12.016
Irrgang JJ, Anderson AF (2002) Development and validation of health-related quality of life measures for the knee. Clin Orthop Relat Res 1976–2007:402
Janssen MF, Szende A, Cabases J, Ramos-Goni JM, Vilagut G, Konig HH (2019) Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. Eur J Health Econ 20:205–216. https://doi.org/10.1007/s10198-018-0955-5
Kendoff D, Haasper C, Gehrke T, Klauser W, Sandiford N (2020) Management of gonarthrosis with a rotating hinge prosthesis: minimum 10-year follow-up. Clin Orthop Surg 12:464–469. https://doi.org/10.4055/cios19153
Kocaoglu H, Hennes F, Abdelaziz H, Neufeld ME, Gehrke T, Citak M (2022) Survival analysis of one-stage exchange of infected unicompartmental knee arthroplasty: a single-center study with minimum 3 years follow-up. Eur J Orthop Surg Traumatol. Doi: https://doi.org/10.1007/s00590-021-03187-7
Kouk S, Rathod PA, Maheshwari AV, Deshmukh AJ (2018) Rotating hinge prosthesis for complex revision total knee arthroplasty: a review of the literature. J Clin Orthop Trauma 9:29–33. https://doi.org/10.1016/j.jcot.2017.11.020
Kowalczewski J, Marczak D, Synder M, Sibinski M (2014) Primary rotating-hinge total knee arthroplasty: good outcomes at mid-term follow-up. J Arthroplasty 29:1202–1206. https://doi.org/10.1016/j.arth.2013.12.013
Kumar N, Yadav C, Raj R, Anand S (2014) How to interpret postoperative X-rays after total knee arthroplasty. Orthop Surg 6:179–186. https://doi.org/10.1111/os.12123
Lim JBT, Pang HN, Tay KJD, Chia SL, Lo NN, Yeo SJ (2020) Increased constraint of rotating hinge knee prosthesis is associated with poorer clinical outcomes as compared to constrained condylar knee prosthesis in total knee arthroplasty. Eur J Orthop Surg Traumatol 30:529–535. https://doi.org/10.1007/s00590-019-02598-x
Martin JR, Beahrs TR, Stuhlman CR, Trousdale RT (2016) Complex Primary Total Knee Arthroplasty: Long-Term Outcomes. J Bone Joint Surg Am 98:1459–1470. https://doi.org/10.2106/JBJS.15.01173
Mounasamy V, Cui Q, Brown TE, Saleh KJ, Mihalko WM (2007) Primary total knee arthroplasty for a complex distal femur fracture in the elderly: a case report. Eur J Orthop Surg Traumatol 17:491–494. https://doi.org/10.1007/s00590-007-0224-2
Neri T, Boyer B, Papin PE, Martz P, Vaz G, Eichler D et al (2020) Contemporary rotating hinge arthroplasty can safely be recommended in complex primary surgery. Knee Surg Sports Traumatol Arthrosc 28:1780–1788. https://doi.org/10.1007/s00167-019-05589-x
Pasquier G, Ehlinger M, Mainard D (2019) The role of rotating hinge implants in revision total knee arthroplasty. EFORT Open Rev 4:269–278. https://doi.org/10.1302/2058-5241.4.180070
Rodriguez-Merchan EC (2019) Total knee arthroplasty using hinge joints: Indications and results. EFORT Open Rev 4:121–132. https://doi.org/10.1302/2058-5241.4.180056
Rouquette L, Batailler C, Muller B, Neyret P, Servien E, Lustig S (2020) Early complications and causes of revision after rotating-hinge TKA. Arch Orthop Trauma Surg 140:109–119. https://doi.org/10.1007/s00402-019-03290-9
Touzopoulos P, Drosos GI, Ververidis A, Kazakos K (2015) Constrained Implants in Total Knee Replacement. Surg Technol Int 26:307–316
Wignadasan W, Chang JS, Kayani B, Kontoghiorghe C, Haddad FS (2021) Long-term results of revision total knee arthroplasty using a rotating hinge implant. Knee 28:72–80. https://doi.org/10.1016/j.knee.2020.11.009
Funding
Open access funding provided by University of Bern. Frank M. Klenke received financial research support from Medacta international unrelated to this project. The other authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Inerest
The other authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Local review board that approved the study: Cantonal ethics-commission Bern. Application BASEC-Nr. 2020–01559.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hecker, A., Pütz, HJ.A., Wangler, S. et al. Indications, clinical outcome and survival of rotating hinge total knee arthroplasty in a retrospective study of 63 primary and revision cases. Eur J Orthop Surg Traumatol 33, 1885–1894 (2023). https://doi.org/10.1007/s00590-022-03349-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03349-1