Abstract
Background
Anxiety and depression are associated with patient dissatisfaction after total knee arthroplasty (TKA). Understanding whether preoperative knee-related symptoms could be a cause of anxiety and depression might help prevent unnecessary delay of surgery for this group of patients. We investigated changes in prevalence of anxiety and depression symptoms one year after TKA, and compared demographic data between patients with and without anxiety and depression symptoms preoperatively.
Methods
This was a prospective cohort study of 403 patients scheduled for TKA. Data on patient-related outcome measures and the prevalence of anxiety and depression symptoms were collected preoperatively and one year postoperatively. Before–after differences in anxiety/depression prevalence were compared with a chi-square test, and differences in demographic data between the groups with and without anxiety and/or depression symptoms were compared with an independent t test.
Results
Among the 15% of patients with anxiety symptoms before surgery, 59% had improved in these symptoms one year after surgery; while among the 10% with depression symptoms before surgery, 60% had improved one year after surgery. Patients with preoperative anxiety and/or depression were younger, and had higher body mass index, lower general quality of life (EQ-5D-3L), higher pain scores (visual analog scale), and lower knee-related (KOOS) scores on all subscales except sport.
Conclusion
Presurgical symptoms of anxiety and depression seem to be partly caused by knee symptoms. Understanding of this issue would offer better strategies to prevent unnecessary delay of surgery in this group of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Osteoarthritis is a common and disabling disease of the knee joint [1,2,3]. Total knee arthroplasty (TKA) is effective in improving pain, function, and quality of life for patients with knee osteoarthritis [4,5,6], but about a fifth of patients are not satisfied after the operation [7,8,9]. Preoperative depression and anxiety are predictors for dissatisfaction after TKA [10,11,12]. Overall, a fifth of patients with osteoarthritis experience anxiety and/or depression [13]. However, the annual report from Swedish knee arthroplasty registry (SKAR) in the last two years showed that about 35% of Swedish patients who underwent TKA were reported anxiety symptoms before surgery[14, 15].
Anxiety is a disorder in which the feeling of fear is persistent and overwhelming in relation to a normal situation [16, 17]. Its prevalence in a general population can be as high as 33% [16, 18]. In contrast, only 4–8% of people have a clinical diagnosis of depression. Symptoms of depression are much more frequent than this, but only about a third of patients with depression symptoms require treatment [19].
Previous literature recommends that patients’ anxiety and depression should be assessed and managed before surgery in order to decrease the dissatisfaction rate [10, 20, 21]. However, there is little knowledge about whether the symptoms of depression and anxiety are a result of symptoms and disabilities caused by the knee osteoarthritis. One study showed that increasing disability and poorer quality of life are reasons for higher anxiety prevalence among elderly people [22]. Others found that depression improved after hip/knee replacement surgery due to a reduction in pain [23], and that depression and anxiety symptoms improved 6 months after surgery [24].
The main aim of this study was therefore to investigate changes in the prevalence of anxiety and depression one year after primary TKA. Understanding of this issue might lead to a better preoperative assessment of patients scheduled for TKA. The second aim was to compare preoperative demographic data between patients who did and did not have anxiety and/or depression symptoms, in order to help build up a preoperative profile of patients with these symptoms.
Methods
Patient selection
We performed a prospective cohort study with a consecutive sample of patients scheduled for knee replacement surgery between April 2016 and April 2018 at three hospitals in a county in central Sweden, one university hospital and two local hospitals, serving in total approximately 300,000 people. The surgeons used a standard paramedian approach. Each orthopedic surgeon performed between 25 and 75 primary TKAs per year. The inclusion criteria were having knee osteoarthritis and being scheduled for primary knee replacement surgery at one of the three hospitals. The exclusion criteria were being scheduled for a revision of knee arthroplasty or a unicompartmental knee arthroplasty, or having a diagnosis other than osteoarthritis.
Patient-reported outcome measures (PROMs) were assessed with a questionnaire used by the SKAR. This registry collects individual-based data on patients and surgeries. SKAR provided us with the PROMs questionnaire used annually by the registry, software for entering and calculating scores on the Hospital Anxiety and Depression Scale (HADS), and access to SKAR’s data program for entering PROMs and HADS data. This access concerned only our patients and was restricted to the common database. Thus, we took advantage of SKAR routines in terms of using a well-validated questionnaire and high-quality software which protects the patient’s identity.
Outcome measures
The patients were asked to fill out a PROMs questionnaire at two time points: before surgery and one year after surgery. The questionnaire included the Knee Injury and Osteoarthritis Outcome Score (KOOS), a visual analog scale (VAS) for measuring pain, a general quality of life questionnaire (EQ-5D-3L), and HADS.
KOOS is a knee-specific questionnaire comprising five subscales: pain (9 items), other symptoms (7 items), activities of daily living (17 items), sport and recreation function (5 items), and knee-related quality of life (4 items). It takes about 10 min to answer the questions [25, 26].
A VAS is the commonest and easiest pain rating scale. The patient rates their pain intensity from 0 to 100, with 0 representing no pain and 100 representing the highest pain intensity. It takes less than a minute to complete [27]. SKAR uses the VAS to measure both the patient’s current pain and the patient’s expectation of what their pain would be after surgery.
EQ-5D-3L is a five-dimensional three-level generic instrument covering mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. It is well-known and takes less than a minute to complete [28].
HADS is a simple questionnaire which takes 2–5 min to complete. It consists of 7 items for anxiety and 7 items for depression. The minimum score is 0 and the maximum is 21 for each of the sub-scores. Patients are considered to have anxiety or depression symptoms if their HADS-Anxiety (HADS-A) or HADS-Depression (HADS-D) score, respectively, is more than 7 [29].
All of these PROMs questionnaires have been psychometrically validated [28, 30].
Statistics
A chi-square test was used to compare the two groups with/without anxiety before and one year after surgery. The dependent variable was anxiety symptoms pre-surgery, the independent variable was TKA, and the control variable was symptoms one year postoperatively.
An independent t test was used to compare demographic data between the two groups with and without anxiety before surgery. Similar statistical tests were performed for depression symptoms.
McNemar test was used for pre- and postoperative comparisons of anxiety and depression. Odds ratios were calculated, as were 95% confidence intervals (CIs) when appropriate. Differences were regarded as significant when the p value was less than 0.05. Version 25 of the SPSS software package (IBM, SPSS Inc., Chicago, Illinois, USA) was used for the quantitative analyses.
The power of the study was calculated on the basis of previous studies [23, 24] and a sample size calculator [31]. We expected that 10–20% of patients (n = 30–60) would have symptoms of anxiety and/or depression, and hence estimated that enrolling about 300 patients would be enough to produce statistically significant differences with a power of 0.8 and alpha of 0.05. However, we enrolled 403 patients to compensate for eventual attrition.
The effect size was calculated by measuring the eta-squared value using SPSS with both cross-table comparison and univariate analysis of variance. Eta-squared define the effect size as small, medium and large when its value is 0.01, 0.06 and 0.14, respectively [32, 33].We considered the large effect size to be clinically important.
Results
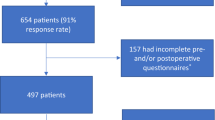
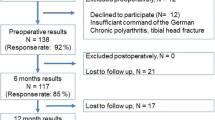
Of the 610 patients who underwent surgery between April 2016 and April 2018, 207 were excluded. Of them, due to declining participation (n = 37), unicompartmental knee arthroplasty (n = 22), revision surgery (n = 12), diagnosis other than primary osteoarthritis (n = 22), and incomplete data (n = 114), leaving 403 included in the study (94% response rate) (Fig. 1).
Reasons for incomplete data were:
-
1.
At the beginning of the study the nurses had not yet got into the routine of distributing the questionnaire, which caused them to miss some patients
-
2.
Patients delaying their answers for more than 3 months
-
3.
Incomplete answering of the questionnaire
-
4.
Patients not returning the preoperative or postoperative questionnaire despite reminders
-
5.
Death
Missing data were distributed randomly, and did not affect a specific group or hospital. Demographics of the patients with incomplete data are shown in Table 1.
Of the 403 patients with complete data, 15% (n = 61) reported significant anxiety symptoms (HADS-A ≥ 8) before TKA, while the remaining 85% (n = 342) were regarded as not having anxiety symptoms (HADS-A < 8). One year after surgery, the group with anxiety showed a significant reduction in HADS-A score, with 59% of the patients in this group now having normal scores (n = 36; p < 0.001). The remaining 41% (n = 25) continued to report anxiety one year after surgery. Thus, the odds ratio for being anxiety-free one year after surgery was 1.6 (95% CI: 1.3–2.0; p < 0.001). Further analysis of the group without preoperative anxiety showed that 98% (n = 335) of them still reported no anxiety symptoms one year after surgery, while symptoms had developed in 2% (n = 7). Thus, the odds ratio for having anxiety symptoms one year after surgery was 0.05 (95% CI: 0.02–0.11; p < 0.001) (Fig. 2).
Further demographic analysis of both groups preoperatively showed that the patients with preoperative anxiety symptoms tended to be younger, and to have higher body mass index (BMI), lower EQ-5D index, lower general health, and lower scores on the KOOS subscales for symptoms, pain, activities of daily living, and knee-related quality of life. All these differences were statistically significant (Table 2; Fig. 3). Gender, American Society of Anesthesiologists (ASA) class, surgical time, preoperative VAS, expected VAS, and preoperative KOOS sport/recreation did not differ significantly between the groups (Table 2; Fig. 3).
Of the 403 patients, 10% (n = 40) reported significant depression symptoms (HADS-D ≥ 8) before TKA, while the remaining 90% (n = 363) were regarded as not having depression (HADS-D < 8). One year after surgery, the group with depression showed a statistically significant reduction in HADS-D score, with 60% of the patients in this group now having normal scores (n = 24; p < 0.001) The remaining 40% (n = 16) continued to report depression one year after surgery. Thus, the odds ratio for being depression-free one year after surgery was 1.6 (95% CI: 1.2–2.0; p < 0.001). Further analysis of the group without preoperative depression showed that 96% (n = 349) of them still reported no depression symptoms one year after surgery, while symptoms had developed in 4% (n = 14). Thus, the odds ratio for having depression symptoms one year after surgery was 0.09 (95% CI: 0.05–0.18; p < 0.001) (Fig. 4).
Further demographic analysis of both groups preoperatively showed that the patients with preoperative depression symptoms tended to be younger, and to have higher BMI, higher preoperative VAS, lower preoperative EQ-5D index, lower general health, and lower scores on the KOOS subscales for symptoms, pain, activities of daily living, and knee-related quality of life. All these differences were statistically significant (Table 3; Fig. 5). Gender, ASA class, surgical time, expected VAS, and preoperative KOOS sport/recreation did not differ significantly between the groups (Table 3; Fig. 5).
Patients who showed anxiety symptoms (n = 32) and/or depression symptoms (n = 30) one year after surgery differed from patients without these symptoms in terms of being younger and more likely to be female, having higher BMI, and reporting higher postoperative pain, lower general health, increased comorbidity, generally less satisfaction with their knees, and lower KOOS scores on all subscales (Tables 4, 5; Figs. 6, 7).
There were seven patients who did not report anxiety symptoms before surgery but they developed such symptoms one year after surgery. Similarly, there were also 14 patients who did not report depression symptoms before surgery but they reported such symptoms one year after surgery. The changes were statistically significant regarding anxiety but not depression (p < 0.0001 and p = 0.143, respectively).
Clinical significance was measured by calculating the effect size (eta-squared value) of the reduction in anxiety and depression symptoms. Eta-squared was 0.26 (p < 0.001) for anxiety and 0.17 (p < 0.0001) for depression. Both values were considered a large effect size and considered being clinically relevant.
Discussion
This study examined changes in the prevalence of anxiety and depression symptoms between two time points, before and one year after a total knee arthroplasty in patients with knee osteoarthritis. We showed a significant reduction in anxiety and depression symptoms one year after surgery in patients with such symptoms prior to surgery.
Many previous studies have shown the negative impact of anxiety on the outcome after TKA [7, 8, 20, 21, 34]. This could be used as an argument not to operate on patients with anxiety or depression symptoms, or at least to postpone surgery. However, it is not ethical to either totally exclude these patients from surgery or extend their suffering by postponing surgery. On the other hand, it is important to accurately assess the patient’s preoperative anxiety state in order to avoid patient dissatisfaction, which could be defined as poor results after surgery.
The prevalence of anxiety in a general population varies in the literature, but is estimated to be as high as 33% [16, 18]. It is difficult to say whether the symptoms of anxiety found in our study were related to knee symptoms or were part of the general population prevalence.
The significant reduction in anxiety symptoms that we found one year after surgery might be important for knee surgeons to know when assessing patients preoperatively. Taking into account the improvement of anxiety symptoms in 59% of patients could decrease the discrimination against patients with anxiety symptoms. In addition, our description of the demographics of patients with preoperative anxiety symptoms might aid knee surgeons in clearly defining these patients preoperatively.
Our interpretation of the results is that many patients experienced anxiety/depression symptoms before surgery due to knee symptoms. This interpretation is supported by our further analysis of patients who continued to have anxiety and/or depression one year after surgery. The analysis revealed that these patients had more knee pain and lower KOOS subscale scores postoperatively compared to patients who did not show anxiety/depression symptoms one year after TKA. Our results are in line with previous studies showing the impact of knee symptoms on patients’ anxiety state [22, 24, 35].
The prevalence of depression symptoms before TKA in our data was 10%. A statistically significant 60% reduction in these symptoms one year after surgery might indicate the effect of knee symptom alleviation after surgery. This result is also in line with previous studies [23, 35]. Tarakji et al. (2018) showed a post-surgery improvement in depression symptoms, decrease in pain, and improvement in physical function, and interpreted this as an additional benefit of knee arthroplasty. We found that patients who described more depression symptoms before and after surgery had more knee pain and symptoms than patients who did not have depression symptoms.
In contrast, most earlier studies investigated the negative impact of depression on the outcome after knee arthroplasty [7, 10, 11, 36, 37]. Here, again, relying on these studies would lead to discriminating against a group of patients who would be helped by knee arthroplasty, and hence unnecessarily increasing their suffering by excluding or postponing them from surgery. As with anxiety, the demographic data we report here can provide a profile of patients with and without depression symptoms before surgery, which could help in correctly analyzing patients with preoperative depression symptoms.
A strength of this study was its prospective cohort design with large sample size. This allowed the calculation of prevalence and odds ratios for both groups with anxiety and depression symptoms before and after surgery. The results were not only statistically significant but also showed a clinically significant impact. The effect size of symptom reduction was considered to be large because the eta-squared value was larger than 0.14 [32, 33].
Another strength was that we included all patients with knee osteoarthritis who underwent TKA at three different hospitals. This served to minimize the risk of selection bias even though many cases were lost to follow-up.
The relatively large number of missing cases (n = 114, 18%) could be regarded as a weakness. However, it did not affect any one specific group, and it was distributed randomly among the patients. Further analysis of patients with incomplete data was performed. This showed that these patients tend to be younger, have higher BMI, more often Charnley class C and reported more presurgical anxiety symptoms. On the other hand, there were no significant differences regarding gender, ASA and presurgical depression symptoms.
Another limitation was the dichotomization of anxiety and depression before and after surgery, meaning that we did not take the severity of the depression and anxiety symptoms into account. Further classification of anxiety and depression symptoms into mild, moderate, and severe would have spread the patients into several subgroups, leading to a small number of patients in each subgroup, which in turn would have affected the statistical significance of the results. Further studies with larger sample size are needed in order to analyze the subgroups of anxiety and depression symptoms and clarify the role of symptom severity in relation to improvement of symptoms one year after TKA.
Another limitation was relating to the fact that both anxiety and especially depression symptoms are episodic and often recurrent with spontaneous worsening and improvement [38, 39]. Thus, we do not know the number of patients who improved spontaneously or as a result of improved knee symptoms. On the other hand, the same principle should apply in patients with spontaneous worsening of anxiety/depression symptoms. Moreover, comparison among the groups in this study showed that patients with anxiety or depression symptoms had significantly higher knee complaints whether before or after surgery. Moreover, the HADS score of below 7 is regarded in the literature as normal value regardless of the variations below this score [29].
Conclusions
This study showed a significant reduction in anxiety and depression symptoms one year after TKA, which has clinical implications for daily orthopedic work. Our results can serve as a tool to support the beneficial effect of TKA in patients with knee arthrosis alongside anxiety or/and depression symptoms. Excluding this group of patients or postponing surgery would lead to more patient suffering as well as a higher economic burden on the community. Further studies with larger samples are needed to examine the subgroups of patients with anxiety and depression symptoms.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- HADS:
-
Hospital Anxiety and Depression Scale
- KOOS:
-
Knee injury and Osteoarthritis Outcome Score
- PROMS:
-
Patient-Related Outcome Measures
- SKAR:
-
Swedish Knee Arthroplasty Register
- TKA:
-
Total Knee Arthroplasty
- VAS:
-
Visual Analog Scale
References
Hussain SM, Neilly DW, Baliga S, Patil S, Meek R (2016) Knee osteoarthritis: a review of management options. Scott Med J 61(1):7–16
Veronese N, Stubbs B, Solmi M, Smith TO, Noale M, Schofield P, Maggi S (2018) Knee osteoarthritis and risk of hypertension: a longitudinal cohort study. Rejuvenation Res 21(1):15–21
Hana S, Aicha BT, Selim D, Ines M, Rawdha T (2018) Clinical and radiographic features of knee osteoarthritis of elderly patients. Curr Rheumatol Rev 14(2):181–187
Bontempi M, Cardinale U, Bragonzoni L, Macchiarola L, Grassi A, Signorelli C, Marcheggiani Muccioli GM, Zaffagnini S (2017) Total knee replacement: intraoperative and postoperative kinematic assessment. Acta Biomed 88(2s):32–37
Austin DC, Torchia MT, Moschetti WE, Jevsevar DS, Keeney BJ (2018) Patient outcomes after total knee arthroplasty in patients older than 80 years. J Arthroplast 33(11):3465–3473
Harding P, Holland AE, Delany C, Hinman RS (2014) Do activity levels increase after total hip and knee arthroplasty? Clin Orthop Relat Res 472(5):1502–1511
Gibon E, Goodman MJ, Goodman SB (2017) Patient satisfaction after total knee arthroplasty: a realistic or imaginary goal? Orthop Clin North Am 48(4):421–431
Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW (2017) Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplast 32(12):3854–3860
Howells N, Murray J, Wylde V, Dieppe P, Blom A (2016) Persistent pain after knee replacement: do factors associated with pain vary with degree of patient dissatisfaction? Osteoarthr Cartil 24(12):2061–2068
Ali A, Lindstrand A, Sundberg M, Flivik G (2017) Preoperative anxiety and depression correlate with dissatisfaction after total knee arthroplasty: a prospective longitudinal cohort study of 186 patients, with 4-year follow-up. J Arthroplast 32(3):767–770
Bierke S, Haner M, Petersen W (2016) Influence of somatization and depressive symptoms on the course of pain within the first year after uncomplicated total knee replacement: a prospective study. Int Orthop 40(7):1353–1360
Wylde V, Trela-Larsen L, Whitehouse MR, Blom AW (2017) Preoperative psychosocial risk factors for poor outcomes at 1 and 5 years after total knee replacement. Acta Orthop 88(5):530–536
Stubbs B, Aluko Y, Myint PK, Smith TO (2016) Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing 45(2):228–235
SKAR (2019) Annual report Swedish knee arthroplasty register 2018. SKAR, Sweden
SKAR (2020) Annual report 2019. Lund university, Sweden
Dean E (2016) Anxiety. Nurs Stand 30(46):15
Schuyler D (2016) Anxiety. Prim Care Companion CNS Disord 18(5):1
Nechita D, Nechita F, Motorga R (2018) A review of the influence the anxiety exerts on human life. Rom J Morphol Embryol 59(4):1045–1051
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC (2018) Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep 8(1):2861
Bierke S, Petersen W (2017) Influence of anxiety and pain catastrophizing on the course of pain within the first year after uncomplicated total knee replacement: a prospective study. Arch Orthop Trauma Surg 137(12):1735–1742
Alattas SA, Smith T, Bhatti M, Wilson-Nunn D, Donell S (2017) Greater pre-operative anxiety, pain and poorer function predict a worse outcome of a total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(11):3403–3410
Koychev I, Ebmeier KP (2016) Anxiety in older adults often goes undiagnosed. Practitioner 260(1789):17–20
Tarakji BA, Wynkoop AT, Srivastava AK, O’Connor EG, Atkinson TS (2018) Improvement in depression and physical health following total joint arthroplasty. J Arthroplast 33(8):2423–2427
Hassett AL, Marshall E, Bailey AM, Moser S, Clauw DJ, Hooten WM, Urquhart A, Brummett CM (2018) Changes in anxiety and depression are mediated by changes in pain severity in patients undergoing lower-extremity total joint arthroplasty. Reg Anesth Pain Med 43(1):14–18
Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM (2016) Knee injury and osteoarthritis outcome score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthr Cartil 24(8):1317–1329
Roos EM, Lohmander LS (2003) The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), Short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res (Hoboken) 63(Suppl 11):S240-252
Devlin NJ, Brooks R (2017) EQ-5D and the euroqol group: past, present and future. Appl Health Econ Health Policy 15(2):127–137
Stern AF (2014) The hospital anxiety and depression scale. Occup Med (Lond) 64(5):393–394
Djukanovic I, Carlsson J, Arestedt K (2017) Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65–80 years old? A psychometric evaluation study. Health Qual Life Outcomes 15(1):193
Sample Size Calculator Determines the minimum number of subjects for adequate study power. https://clincalc.com/stats/samplesize.aspx.
Rules of thumb on magnitudes of effect sizes. http://imaging.mrc-cbu.cam.ac.uk/statswiki/FAQ/effectSize.
Lakens D (2013) Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol 4:863
Dhurve K, Scholes C, El-Tawil S, Shaikh A, Weng LK, Levin K, Fritsch B, Parker D, Coolican M (2017) Multifactorial analysis of dissatisfaction after primary total knee replacement. Knee 24(4):856–862
Duivenvoorden T, Vissers MM, Verhaar JA, Busschbach JJ, Gosens T, Bloem RM, Bierma-Zeinstra SM, Reijman M (2013) Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthr Cartil 21(12):1834–1840
Bistolfi A, Bettoni E, Aprato A, Milani P, Berchialla P, Graziano E, Massazza G, Lee GC (2017) The presence and influence of mild depressive symptoms on post-operative pain perception following primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(9):2792–2800
Gold HT, Slover JD, Joo L, Bosco J, Iorio R, Oh C (2016) Association of depression with 90-day hospital readmission after total joint arthroplasty. J Arthroplast 31(11):2385–2388
Stordal E, Bjartveit Kruger M, Dahl NH, Kruger O, Mykletun A, Dahl AA (2001) Depression in relation to age and gender in the general population: the nord-trondelag health study (HUNT). Acta Psychiatr Scand 104(3):210–216
Stordal E, Morken G, Mykletun A, Neckelmann D, Dahl AA (2008) Monthly variation in prevalence rates of comorbid depression and anxiety in the general population at 63–65 degrees North: the HUNT study. J Affect Disord 106(3):273–278
Acknowledgments
We thank Ole Brus (Clinical Epidemiology and Biostatistics, School of Medical Sciences, Örebro University, Örebro, Sweden) for statistical advice and help with the SPSS software package, and Inger Andersson (nurse and chief coordinator, Department of Orthopedics, Örebro University Hospital, Sweden) for her well-structured and organized data entry and for sending reminders to the patients who did not answer in good time.
Funding
Open Access funding provided by Örebro University. This study was funded by the Örebro Research Committee, Sweden, and the Orthopaedic Department, Karlskoga Hospital, Sweden. No external funding or benefits were received. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
AM created the study protocol and design and wrote the manuscript. AM and MHN performed the analysis. PW and MHN contributed to the study design. MHN and PW contributed to the revision of the manuscript. AM and PW collected the data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Consent to participate
Verbal and written consent were obtained from the participants before surgery, and a new written consent form was sent together with the questionnaire one year after surgery. The data were treated with full confidentiality.
Ethical approval
The study was approved by the Regional Ethical Review Board of Uppsala, Sweden (ref: 2016/191 [2019–02077]).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahdi, A., Hälleberg-Nyman, M. & Wretenberg, P. Reduction in anxiety and depression symptoms one year after knee replacement: a register-based cohort study of 403 patients. Eur J Orthop Surg Traumatol 31, 1215–1224 (2021). https://doi.org/10.1007/s00590-020-02860-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02860-7