Abstract
Introduction
Little is known about the association between well-fixed polished tapered cemented stems (PTCS) implanted by the line-to-line technique and changes of stem migration, or the change of functional anteversion of the femur after total hip arthroplasty (THA).
Materials and methods
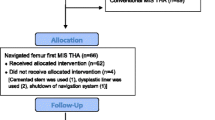
This retrospective study included 422 two-stage bilateral primary THAs performed using PTCS implanted by the line-to-line technique. CT scans were made on both the target side (first postoperative CT) and on the contralateral side (second postoperative CT) 1 week postoperatively. The mean follow-up was 7.8 months. CT data for each scan were transferred to 3D template software (Zed hip, Lexi, Japan). The postoperative changes of anatomical stem anteversion (ASA), functional femoral anteversion (FFA), and stem subsidence were evaluated.
Results
A total of 20 THAs with CT scans were available on 3D template software. The ASA and the FFA had migrated − 0.68° ± 0.62° and − 5.5° ± 9.7°, respectively, over the follow-up period. A significant positive correlation was observed between the change of subsidence and ASA (r2 = 0.34, p = 0.007), between the FFA on the second postoperative CT and ASA on the first postoperative CT (r2 = 0.26, p = 0.02) and between the FFA on the second postoperative CT and FFA on the first postoperative CT (r2 = 0.52, p = 0.0003).
Conclusion
This study indicates that the change in axial rotation of a PTCS implanted by the line-to-line technique was less than that reported by other studies and the preoperative external rotation contracture was substantially improved after THA.





Similar content being viewed by others
References
Petheram TG, Whitehouse SL, Kazi HA, Hubble MJ, Timperley AJ, Wilson MJ, Howell JR (2016) The Exeter universal cemented femoral stem at 20–25 years: a report of 382 hips. Bone Jt J 98:1441–1449
Ling RS, Charity J, Lee AJ, Whitehouse SL, Timperley AJ, Gie GA (2009) The long-term results of the original Exeter polished cemented femoral component: a follow-up report. J Arthroplasty 24:511–517. https://doi.org/10.1016/j.arth.2009.02.002
Purbach B, Kay PR, Siney PD, Fleming PA, Wroblewski BM (2013) The C-stem in clinical practice: 15-year follow-up of a triple tapered polished cemented stem. J Arthroplasty 28:1367–1371. https://doi.org/10.1016/j.arth.2012.10.030
Burston BJ, Barnett AJ, Amirfeyz R, Yates PJ, Bannister GC (2012) Clinical and radiological results of the collarless polished tapered stem at 15 years follow-up. J Bone Jt Surg Br 94:889–894. https://doi.org/10.1302/0301-620X.94B7.28799
Shen G (1998) Femoral stem fixation. An engineering interpretation of the long-term outcome of Charnley and Exeter stems. J Bone Jt Surg Br 80:754–756
Eden OR, Lee AJ, Hooper RM (2002) Stress relaxation modelling of polymethylmethacrylate bone cement. Proc Inst Mech Eng Part H J Eng Med 216:195–199
Scheerlinck T, Casteleyn PP (2006) The design features of cemented femoral hip implants. J Bone Jt Surg Br 88:1409–1418
Nizard RS, Sedel L, Christel P, Meunier A, Soudry M, Witvoet J (1992) Ten-year survivorship of cemented ceramic–ceramic total hip prosthesis. Clin Orthop Relat Res 282:53–63
Erivan R, Villatte G, Khelif YR, Pereira B, Galvin M, Descamps S, Boisgard S (2017) The Müller self-locking cemented total hip prosthesis with polyethylene liner: after 20 years, what did they become? Int Orthop 41:47–54. https://doi.org/10.1007/s00264-016-3191-6
Kerboull L, Hamadouche M, Courpied JP, Kerboull M (2004) Long-term results of Charnley–Kerboull hip arthroplasty in patients younger than 50 years. Clin Orthop Relat Res 418:112–118
Langlais F, Kerboull M, Sedel L, Ling RS (2003) The 'French paradox'. J Bone Jt Surg Br 85:17–20
Williams HD, Browne G, Gie GA, Ling RS, Timperley AJ, Wendover NA (2002) The Exeter universal cemented femoral component at 8–12 years. A study of the first 325 hips. J Bone Jt Surg Br 84:324–334
Carrington NC, Sierra RJ, Gie GA, Hubble MJ, Timperley AJ, Howell JR (2009) The Exeter universal cemented femoral component at 15–17 years: an update on the first 325 hips. J Bone Jt Surg Br 91:730–737. https://doi.org/10.1302/0301-620X.91B6.21627
Sundberg M, Besjakov J, von Schewelow T, Carlsson A (2005) Movement patterns of the C-stem femoral component: an RSA study of 33 primary total hip arthroplasties followed for 2 years. J Bone Jt Surg Br 87:1352–1356
Alfaro-Adrián J, Gill HS, Murray DW (1999) Cement migration after THR. A comparison of Charnley elite and Exeter femoral stems using RSA. J Bone Jt Surg Br 81:130–134
Murray DW, Gulati A, Gill HS (2013) Ten-year RSA-measured migration of the Exeter femoral stem. Bone Jt J 95:605–608. https://doi.org/10.1302/0301-620X.95B5.31330
von Schewelov T, Carlsson A, Sanzén L, Besjakov J (2014) Continuous distal migration and internal rotation of the C-stem prosthesis without any adverse clinical effects: an RSA study of 33 primary total hip arthroplasties followed for up to 10 years. Bone Jt J 96:604–608. https://doi.org/10.1302/0301-620X.96B5.33580
El Masri F, Kerboull L, Kerboull M, Courpied JP, Hamadouche M (2010) Is the so-called 'French paradox' a reality? Long-term survival and migration of the Charnley–Kerboull stem cemented line-to-line. J Bone Jt Surg Br 92:342–348. https://doi.org/10.1302/0301-620X.92B3.23151
Nieuwenhuijse MJ, Valstar ER, Kaptein BL, Nelissen RG (2012) The Exeter femoral stem continues to migrate during its first decade after implantation: 10–12 years of follow-up with radiostereometric analysis (RSA). Acta Orthop 83:129–134. https://doi.org/10.3109/17453674.2012.672093
McCalden RW, Charron KD, Yuan X, Bourne RB, Naudie DD, MacDonald SJ (2010) Randomised controlled trial comparing early migration of two collarless polished cemented stems using radiostereometric analysis. J Bone Jt Surg Br 92:935–940. https://doi.org/10.1302/0301-620X.92B7.24462
Uemura K, Takao M, Hamada H, Sakai T, Sugano N (2018) Change in axial rotation of the femur in the resting supine position following total hip arthroplasty. Artif Organs 42:290–296. https://doi.org/10.1111/aor.12998
Uemura K, Takao M, Otake Y et al (2018) Can anatomic measurements of stem anteversion angle be considered as the functional anteversion angle? J Arthroplasty 33:595–600. https://doi.org/10.1016/j.arth.2017.09.027
Hayashi S, Fujishiro T, Hashimoto S, Kanzaki N, Kuroda R, Kurosaka M (2015) The contributing factors of tapered wedge stem alignment during mini-invasive total hip arthroplasty. J Orthop Surg Res 10:52. https://doi.org/10.1186/s13018-015-0192-x
Inoue D, Kabata T, Maeda T et al (2016) The correlation between clinical radiological outcome and contact state of implant and femur using three-dimensional templating software in cementless total hip arthroplasty. Eur J Orthop Surg Traumatol 26:591–598. https://doi.org/10.1007/s00590-016-1796-5
Takahashi E, Kaneuji A, Tsuda R et al (2017) The influence of cement thickness on stem subsidence and cement creep in a collarless polished tapered stem: when are thick cement mantles detrimental? Bone Jt Res 6:351–357. https://doi.org/10.1302/2046-3758.65
Abadie P, Lebel B, Pineau V, Burdin G, Vielpeau C (2010) Cemented total hip stem design influence on adaptative cortical thickness and femoral morphology. Orthop Traumatol Surg Res 96:104–110. https://doi.org/10.1016/j.rcot.2010.02.006
Stefánsdóttir A, Franzén H, Johnsson R, Ornstein E, Sundberg M (2004) Movement pattern of the Exeter femoral stem; a radiostereometric analysis of 22 primary hip arthroplasties followed for 5 years. Acta Orthop Scand 75:408–414
Numata Y, Kaneuji A, Kerboull L et al (2018) Biomechanical behaviour of a French femoral component with thin cement mantle: the 'French paradox' may not be a paradox after all. Bone Jt Res 7:485–493. https://doi.org/10.1302/2046-3758.77
Acknowledgements
We are grateful to Dr. Satoshi Iida, Dr. Chiho Suzuki, Dr. Junichi Nakamura, Dr. Yuya Kawarai, Dr. Takushi Nakatani, Associate Professor Sumihisa Orita and Professor Seiji Ohtori head of our department, for their valuable suggestions and support during the course of this study. All authors have read and approved the submitted version. Study design: Shuichi Miyamoto, Satoshi Iida, Sumihisa Orita, Seiji Ohtori. Drafting the protocol: Shuichi Miyamoto, Satoshi Iida. Advice on the statistical analysis: Shuichi Miyamoto, Junichi Nakamura, Sumihisa Orita. Patient recruitment and data collection: Chiho Suzuki, Yuya Kawarai, Takushi Nakatani. First draft of the manuscript: Shuichi Miyamoto.
Funding
No author received any funding or financial support that may be perceived to have biased the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Ethical standards
The study protocol was in accordance with the Declaration of Helsinki for human research and approved by the Matsudo City General Hospital ethics committee.
Informed consent
Informed consent was obtained from the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyamoto, S., Iida, S., Suzuki, C. et al. Postoperative migration of the anatomical and functional anteversion angle following total hip arthroplasty with a well-fixed cemented femoral component with line-to-line implantation. Eur J Orthop Surg Traumatol 30, 1067–1074 (2020). https://doi.org/10.1007/s00590-020-02671-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02671-w