Abstract
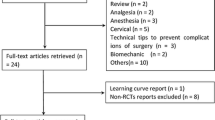
Treatment for lumbar disc herniation after failed conservative treatment is discectomy. Discectomy can significantly relieve back pain as well as radicular symptoms. However, many patients with lumbar discectomy experience moderate-to-severe back pain and radicular leg pain. The results of application of epidural steroids (ES) for pain management after lumbar discectomy have previously been inconclusive. We have conducted a systematic review and meta-analysis aims to compare outcomes (efficacy and complications) of epidural steroid application and placebo after discectomy in lumbar disc herniation. This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Relevant studies that reported visual analog scale of back and leg pain, morphine consumption, hospital stay and post-operative complications of either group were identified from Medline and Scopus from the date of inception to 28 October 2017. A total of 12 studies were pooled and analysed, with nine studies having undergone conventional discectomy and three studies having undergone minimally invasive surgery (MIS) discectomy. Overall, there were 1006 patients (502 in the ES group and 504 in the placebo group) included. The unstandardized mean difference of VAS of back pain at 1 week and 1 month, leg pain at 1 week and 1 month, morphine consumption and hospital stay was − 0.53 (95% CI − 1.42, 0.36) score, − 0.89 (95% CI − 1.36, − 0.42) score, − 0.63 (95% CI − 0.75, − 0.50) score, − 0.47 (95% CI − 0.78, − 0.15) score, − 8.47 (95% CI − 16.16, − 0.78) mg and − 0.89 (95% CI − 1.49, − 0.30) days lower when compared to placebo after lumbar discectomy in patients with lumbar disc herniation. A total of ten studies compared the ratio of complication between the ES and placebo groups. No significant differences were noted for complications within the two groups (0.92; 95% CI 0.47, 1.83). This meta-analysis analysed lower back and leg pain, morphine consumption and hospital stay, with no significant difference in complications for ES application after lumbar discectomy in lumbar disc herniation. In terms of surgical approaches with MIS compared to conventional approach, this review demonstrates that ES can reduce post-operative morphine consumption when the surgical approach is conventional, but not for MIS.
Level of evidence I.



Similar content being viewed by others
References
Abrishamkar S, Rafiei AR, Sabouri M, Moradi S, Tabesh H, Rahmani P, Hekmatnia A, Torkashvand M, Eshraghi N, Baghershahi G (2011) The effect of impregnated autogenous epidural adipose tissue with bupivacaine, methylprednisolone acetate or normal saline on postoperative radicular and low back pain in lumbar disc surgery under spinal anesthesia; a randomized clinical trial study. J Res Med Sci 16(5):621
Akinduro OO, Miller BA, Haussen DC, Pradilla G, Ahmad FU (2015) Complications of intraoperative epidural steroid use in lumbar discectomy: a systematic review and meta-analysis. Neurosurg Focus 39(4):E12. https://doi.org/10.3171/2015.7.focus15269
Aljabi Y, El-Shawarby A, Cawley DT, Aherne T (2015) Effect of epidural methylprednisolone on post-operative pain and length of hospital stay in patients undergoing lumbar microdiscectomy. Surg J R Coll Surg Edinb Irel 13(5):245–249. https://doi.org/10.1016/j.surge.2014.03.012
Bahari S, El-Dahab M, Cleary M, Sparkes J (2010) Efficacy of triamcinolone acetonide and bupivacaine for pain after lumbar discectomy. Eur Spine J 19(7):1099–1103. https://doi.org/10.1007/s00586-010-1360-7
Debi R, Halperin N, Mirovsky Y (2002) Local application of steroids following lumbar discectomy. J Spinal Disord Tech 15(4):273–276
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56(2):455–463
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Fan S, Hu Z, Zhao F, Zhao X, Huang Y, Fang X (2010) Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J 19(2):316–324. https://doi.org/10.1007/s00586-009-1191-6
Glasser RS, Knego RS, Delashaw JB, Fessler RG (1993) The perioperative use of corticosteroids and bupivacaine in the management of lumbar disc disease. J Neurosurg 78(3):383–387. https://doi.org/10.3171/jns.1993.78.3.0383
Hurlbert RJ, Theodore N, Drabier JB, Magwood AM, Sonntag VK (1999) A prospective randomized double-blind controlled trial to evaluate the efficacy of an analgesic epidural paste following lumbar decompressive surgery. J Neurosurg 90(2 Suppl):191–197
Jamjoom BA, Jamjoom AB (2014) Efficacy of intraoperative epidural steroids in lumbar discectomy: a systematic review. BMC Musculoskelet Disord. https://doi.org/10.1186/1471-2474-15-146
Jirarattanaphochai K, Jung S, Thienthong S, Krisanaprakornkit W, Sumananont C (2007) Peridural methylprednisolone and wound infiltration with bupivacaine for postoperative pain control after posterior lumbar spine surgery: a randomized double-blinded placebo-controlled trial. Spine 32(6):609–616. https://doi.org/10.1097/01.brs.0000257541.91728.a1
Lavyne MH, Bilsky MH (1992) Epidural steroids, postoperative morbidity, and recovery in patients undergoing microsurgical lumbar discectomy. J Neurosurg 77(1):90–95. https://doi.org/10.3171/jns.1992.77.1.0090
Liu S, Boutrand JP, Tadie M (2001) Use of a collagen-based sealant to prevent in vivo epidural adhesions in an adult rat laminectomy model. J Neurosurg 94(1 Suppl):61–67
Lotfinia I, Khallaghi E, Meshkini A, Shakeri M, Shima M, Safaeian A (2007) Interaoperative use of epidural methylprednisolone or bupivacaine for postsurgical lumbar discectomy pain relief: a randomized, placebo-controlled trial. Ann Saudi Med 27(4):279–283
Lundin A, Magnuson A, Axelsson K, Kogler H, Samuelsson L (2003) The effect of perioperative corticosteroids on the outcome of microscopic lumbar disc surgery. Eur Spine J 12(6):625–630. https://doi.org/10.1007/s00586-003-0554-7
Mirzai H, Tekin I, Alincak H (2002) Perioperative use of corticosteroid and bupivacaine combination in lumbar disc surgery: a randomized controlled trial. Spine 27(4):343–346. https://doi.org/10.1097/00007632-200202150-00003
Modi H, Chung KJ, Yoon HS, Yoo HS, Yoo JH (2009) Local application of low-dose Depo-Medrol is effective in reducing immediate postoperative back pain. Int Orthop 33(3):737–743. https://doi.org/10.1007/s00264-008-0547-6
Murphy RW (1977) Nerve roots and spinal nerves in degenerative disk disease. Clin Orthop Relat Res 129:46–60
Palmer TM, Peter JL, Sutton AJ, Moreno SG (2008) Contour-enhanced funnel plots for meta-analysis. STATA J 8(2):242–254
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2008) Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 61(10):991–996. https://doi.org/10.1016/j.jclinepi.2007.11.010
Pobereskin LH, Sneyd JR (2000) Does wound irrigation with triamcinolone reduce pain after surgery to the lumbar spine? Br J Anaesth 84(6):731–734
Rasmussen S, Krum-Møller DS, Lauridsen LR, Jensen SEH, Mandøe H, Gerlif C, Kehlet H (2008) Epidural steroid following discectomy for herniated lumbar disc reduces neurological impairment and enhances recovery: a randomized study with two-year follow-up. Spine 33(19):2028–2033. https://doi.org/10.1097/BRS.0b013e3181833903
Shin SH, Hwang BW, Keum HJ, Lee SJ, Park SJ, Lee SH (2015) Epidural steroids after a percutaneous endoscopic lumbar discectomy. Spine 40(15):E859–E865. https://doi.org/10.1097/BRS.0000000000000990
StataCorp (2015) Stata statistical software: release 14. StataCorp LP, College Station
Waqas M, Shallwani H, Shamim M, Ahmad K (2017) Perioperative steroids for lumbar disc surgery: a meta-analysis of randomized controlled trials. Surg Neurol Int. https://doi.org/10.4103/sni.sni_478_16
Acknowledgements
All authors declare no funding source or sponsor involvement in the study design, collection, analysis and interpretation of the data, in writing the manuscript and in submission of the manuscript for publication.
Author information
Authors and Affiliations
Contributions
AA was responsible for the conception and design, collection and assembly of data, analysis and interpretation of the data, drafting of the manuscript, final approval of the article. MS was responsible for the conception and design, collection and assembly of data, critical revision of the manuscript for important intellectual content, final approval of the article. SP was responsible for manuscript writing, critical revision of the manuscript for important intellectual content, final approval of the article. KS was responsible for manuscript writing, critical revision of the manuscript for important intellectual contents, final approval of the article. PP was responsible for collection and assembly of data. CP was responsible for collection and assembly of data. JK was responsible for the conception and design, collection and assembly of data, supervise in analysis and interpretation of the data, writing the manuscript, critical revision of the manuscript for important intellectual contents, final approval of the article, statistical expertise.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interests.
Ethical standards
This article does not contain any studies with human participants performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arirachakaran, A., Siripaiboonkij, M., Pairuchvej, S. et al. Comparative outcomes of epidural steroids versus placebo after lumbar discectomy in lumbar disc herniation: a systematic review and meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 28, 1589–1599 (2018). https://doi.org/10.1007/s00590-018-2229-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2229-4