Abstract
Purpose
The use of tranexamic acid (TXA) in total hip arthroplasty (THA) can significantly reduce blood losses with many clinical and economical advantages. However, no consensus has been reached regarding the optimal regimen for TXA administration. The aim of this study is to analyse and compare the haemostatic effect of two different intravenous (IV) regimens of TXA.
Materials and methods
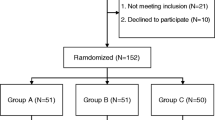
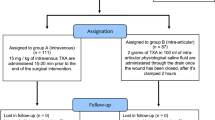
We planned a single-centre, prospective, randomized study including 80 patients who underwent primary unilateral minimally invasive THA because of a hip osteoarthritic degeneration. We divided patients into two groups: the G10 group received two IV doses of 10 mg/kg of TXA, and the G20 group received two doses of 20 mg/kg.
Results
No significant differences in mean minimum levels of Hb and HcT stratified by days after surgery were uncovered between the two groups despite the use of two different dosages of TXA. Also the mean blood volume loss was statistically similar between two groups. No differences were also observed regarding the occurrence of adverse effects.
Conclusions
In two IV bolus regimens of TXA administration, the use of a dose of 10 or 20 mg/kg provides statistically similar results in blood loss sparing. Therefore, the use of two 10 mg/kg doses could be considered more advisable in order to reduce the potential thromboembolic risks related to this drug.

Similar content being viewed by others
References
Memtsoudis SG, Sun X, Chiu YL, Nurok M, Stundner O, Pastores SM, Mazumdar M (2012) Utilization of critical care services among patients undergoing total hip and knee arthroplasty: epidemiology and risk factors. Anesthesiology 117(1):107–116. doi:10.1097/ALN.0b013e31825afd36
Browne JA, Adib F, Brown TE, Novicoff WM (2013) Transfusion rates are increasing following total hip arthroplasty: risk factors and outcomes. J Arthroplasty 28(8 Suppl):34–37. doi:10.1016/j.arth.2013.03.035
Ahmed I, Chan JK, Jenkins P, Brenkel I, Walmsley P (2012) Estimating the transfusion risk following total knee arthroplasty. Orthopedics 35(10):e1465–e1471. doi:10.3928/01477447-20120919-13
Lemaire R (2008) Strategies for blood management in orthopaedic and trauma surgery. The Journal of Bone and Joint Surgery 90(9):1128–1136. doi:10.1302/0301-620X.90B9.21115
Kumar A (2009) Perioperative management of anemia: limits of blood transfusion and alternatives to it. Cleve Clin J Med 76(Suppl 4):S112–S118. doi:10.3949/ccjm.76.s4.18
Cardone D, Klein AA (2009) Perioperative blood conservation. Eur J Anaesthesiol 26(9):722–729. doi:10.1097/EJA.0b013e32832c5280
Sharrock NE, Mineo R, Urquhart B, Salvati EA (1993) The effect of two levels of hypotension on intraoperative blood loss during total hip arthroplasty performed under lumbar epidural anesthesia. Anesth Analg 76(3):580–584
Rajesparan K, Biant LC, Ahmad M, Field RE (2009) The effect of an intravenous bolus of tranexamic acid on blood loss in total hip replacement. The Journal of Bone and Joint Surgery 91(6):776–783. doi:10.1302/0301-620X.91B6.22393
Hoylaerts M, Lijnen HR, Collen D (1981) Studies on the mechanism of the antifibrinolytic action of tranexamic acid. Biochem Biophys Acta 673(1):75–85
Eubanks JD (2010) Antifibrinolytics in major orthopaedic surgery. J Am Acad Orthop Surg 18(3):132–138
Mongan PD, Brown RS, Thwaites BK (1998) Tranexamic acid and aprotinin reduce postoperative bleeding and transfusions during primary coronary revascularization. Anesth Analg 87(2):258–265
Boylan JF, Klinck JR, Sandler AN, Arellano R, Greig PD, Nierenberg H, Roger SL, Glynn MF (1996) Tranexamic acid reduces blood loss, transfusion requirements, and coagulation factor use in primary orthotopic liver transplantation. Anesthesiology 85(5):1043–1048 (discussion 1030A-1031A)
Wellington K, Wagstaff AJ (2003) Tranexamic acid: a review of its use in the management of menorrhagia. Drugs 63(13):1417–1433
Poeran J, Rasul R, Suzuki S, Danninger T, Mazumdar M, Opperer M, Boettner F, Memtsoudis SG (2014) Tranexamic acid use and postoperative outcomes in patients undergoing total hip or knee arthroplasty in the United States: retrospective analysis of effectiveness and safety. BMJ 349:g4829. doi:10.1136/bmj.g4829
Sukeik M, Alshryda S, Haddad FS, Mason JM (2011) Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. The Journal of Bone and Joint Surgery 93(1):39–46. doi:10.1302/0301-620X.93B1.24984
Xu Q, Yang Y, Shi P, Zhou J, Dai W, Yao Z, Zhang C (2014) Repeated doses of intravenous tranexamic acid are effective and safe at reducing perioperative blood loss in total knee arthroplasty. Biosci Trends 8(3):169–175
Irisson E, Hemon Y, Pauly V, Parratte S, Argenson JN, Kerbaul F (2012) Tranexamic acid reduces blood loss and financial cost in primary total hip and knee replacement surgery. Orthop Traumatol Surg Res OTSR 98(5):477–483. doi:10.1016/j.otsr.2012.05.002
Weber EW, Slappendel R, Prins MH, van der Schaaf DB, Durieux ME, Strumper D (2005) Perioperative blood transfusions and delayed wound healing after hip replacement surgery: effects on duration of hospitalization. Anesth Analg 100(5):1416–1421. doi:10.1213/01.ANE.0000150610.44631.9D (table of contents)
DiBlasi JF, Smith RP, Garavaglia J, Quedado J, Frye BM, Dietz MJ (2016) Comparing cost, efficacy, and safety of intravenous and topical tranexamic acid in total hip and knee arthroplasty. Am J Orthop 45(7):E439–E443
McGoldrick NP, O’Connor EM, Davarinos N, Galvin R, Quinlan JF (2015) Cost benefit analysis of the use of tranexamic acid in primary lower limb arthroplasty: a retrospective cohort study. World J Orthop 6(11):977–982. doi:10.5312/wjo.v6.i11.977
Slover J, Bosco J (2014) Cost analysis of use of tranexamic acid to prevent major bleeding complications in hip and knee arthroplasty surgery. Am J Orthop 43(10):E217–E220
Lecker I, Wang DS, Whissell PD, Avramescu S, Mazer CD, Orser BA (2016) Tranexamic acid-associated seizures: causes and treatment. Ann Neurol 79(1):18–26. doi:10.1002/ana.24558
Ng W, Jerath A, Wasowicz M (2015) Tranexamic acid: a clinical review. Anaesthesiol Intensive Ther 47(4):339–350. doi:10.5603/AIT.a2015.0011
Hunt BJ (2015) The current place of tranexamic acid in the management of bleeding. Anaesthesia 70(Suppl 1):50–53. doi:10.1111/anae.12910 (e18)
Lin Z, Xiaoyi Z (2016) Tranexamic acid-associated seizures: a meta-analysis. Seizure 36:70–73. doi:10.1016/j.seizure.2016.02.011
Moskal JT, Capps SG (2016) Meta-analysis of intravenous tranexamic acid in primary total hip arthroplasty. Orthopedics 39(5):e883–e892. doi:10.3928/01477447-20160526-02
Chen S, Wu K, Kong G, Feng W, Deng Z, Wang H (2016) The efficacy of topical tranexamic acid in total hip arthroplasty: a meta-analysis. BMC Musculoskelet Disord 17:81. doi:10.1186/s12891-016-0923-0
Vaglio S, Prisco D, Biancofiore G, Rafanelli D, Antonioli P, Lisanti M, Andreani L, Basso L, Velati C, Grazzini G, Liumbruno GM (2016) Recommendations for the implementation of a Patient Blood Management programme. Application to elective major orthopaedic surgery in adults. Blood Transfus 14(1):23–65. doi:10.2450/2015.0172-15
Mercuriali F, Inghilleri G (1996) Proposal of an algorithm to help the choice of the best transfusion strategy. Curr Med Res Opin 13(8):465–478. doi:10.1185/03007999609115227
Allen TH, Peng MT, Chen KP, Huang TF, Chang C, Fang HS (1956) Prediction of blood volume and adiposity in man from body weight and cube of height. Metab, Clin Exp 5(3):328–345
Kagoma YK, Crowther MA, Douketis J, Bhandari M, Eikelboom J, Lim W (2009) Use of antifibrinolytic therapy to reduce transfusion in patients undergoing orthopedic surgery: a systematic review of randomized trials. Thromb Res 123(5):687–696. doi:10.1016/j.thromres.2008.09.015
Zufferey P, Merquiol F, Laporte S, Decousus H, Mismetti P, Auboyer C, Samama CM, Molliex S (2006) Do antifibrinolytics reduce allogeneic blood transfusion in orthopedic surgery? Anesthesiology 105(5):1034–1046
Nilsson IM (1980) Clinical pharmacology of aminocaproic and tranexamic acids. J Clin Pathol Suppl 14:41–47
Benoni GBS, Fredin H (1995) Application of pharmacokinetics data from healthy volunteers for the prediction of plasma concentrations of tranexamic acid in surgical patients. Clin Drug Invest 10:280–287
Sano MHH, Kojima C, Akimoto T (1976) Absorption and excretion of tranexamic acid following intravenous, intramuscular and oral administration in healthy volunteers. Jpn J Clin Pharmacol Ther 7:376–382
Maniar RN, Kumar G, Singhi T, Nayak RM, Maniar PR (2012) Most effective regimen of tranexamic acid in knee arthroplasty: a prospective randomized controlled study in 240 patients. Clin Orthop Relat Res 470(9):2605–2612. doi:10.1007/s11999-012-2310-y
Lemay E, Guay J, Cote C, Roy A (2004) Tranexamic acid reduces the need for allogenic red blood cell transfusions in patients undergoing total hip replacement. Can J Anaesth 51(1):31–37. doi:10.1007/BF03018543
Salido JA, Marin LA, Gomez LA, Zorrilla P, Martinez C (2002) Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery: analysis of predictive factors. J Bone Joint Surg 84-A(2):216–220
Benoni G, Lethagen S, Nilsson P, Fredin H (2000) Tranexamic acid, given at the end of the operation, does not reduce postoperative blood loss in hip arthroplasty. Acta Orthop Scand 71(3):250–254. doi:10.1080/000164700317411834
Benoni G (1999) Tranexamic acid reduces the blood loss in knee arthroplasty—if it’s administered at the right time. Lakartidningen 96(24):2967–2969
Acknowledgements
Thanks to Prof. M. Lisanti for his precious teachings.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Piolanti, N., Del Chiaro, A., Matassi, F. et al. Clinical and instrumental evaluation of two different regimens of tranexamic acid in total hip arthroplasty: a single-centre, prospective, randomized study with 80 patients. Eur J Orthop Surg Traumatol 28, 233–237 (2018). https://doi.org/10.1007/s00590-017-2038-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-017-2038-1