Abstract
Objectives
Hydroxyapatite (HA) is commonly used as bone substitute in clinical practices. However, only few studies have compared the relationship between the mixture ratio of bone graft in the actual clinical field and fusion rate according to bone graft volume. The study aimed to analyze the fusion rate according to the mixture ratio and the amount of bone graft in minimally invasive transforaminal lumbar interbody fusion (MI-TLIF).
Methods
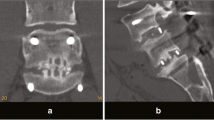
A total number of 88 subjects who completed a 2-year follow-up after MI-TLIF participated in this study. Subjects were divided into three groups: Group 1 with local autograft, Group II with a mixture of HA and autobone of over 50 %, and Group III with a mixture of HA and autobone of less than 50 %. Subjects were also grouped into two groups: Group A with a graft volume of less than 12 ml and Group B with more than 12 ml. The correlation of mixture ratio and the graft volume with fusion rate was analyzed. For clinical analysis, visual analogue scale for pain and Oswestry Disability Index were used. Bone integration was evaluated based on the classification methods described in the Burkus study.
Results
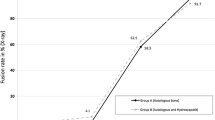
Fusion rates are increased according to the ratio of autograft in all groups: 90.9 % in Group I, 87.8 % in Group II, and 85.7 % in Group III. However, there were no significant differences between groups (p = 0.22). The fusion rates significantly increased as the amount of bone graft increased to over 12 ml, showing 81.5 % in Group A and 92.0 % in Group B (p = 0.03).
Conclusions
A high rate of fusion was achieved in MI-TLIF in graft volume of more than 12 ml. We therefore recommend at least 12 ml of bone graft volume for successful fusion.



Similar content being viewed by others
References
Dhall SS, Wang MY, Mummaneni PV (2008) Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine 9(6):560–565. doi:10.3171/SPI.2008.9.08142
Isaacs RE, Podichetty VK, Santiago P, Sandhu FA, Spears J, Kelly K, Rice L, Fessler RG (2005) Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine 3(2):98–105. doi:10.3171/spi.2005.3.2.0098
Mummaneni PV, Rodts GE, Jr (2005) The mini-open transforaminal lumbar interbody fusion. Neurosurgery 57(4):256–261 discussion 256–261
Park P, Foley KT (2008) Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis: technique and outcomes after a minimum of 2 years’ follow-up. Neurosurg Focus 25(2):E16. doi:10.3171/FOC/2008/25/8/E16
Park Y, Ha JW, Lee YT, Sung NY (2011) The effect of a radiographic solid fusion on clinical outcomes after minimally invasive transforaminal lumbar interbody fusion. Spine J 11(3):205–212
Aspenberg P, Albrektsson T, Thorngren KG (1989) Local application of growth-factor IGF-1 to healing bone. Experiments with a titanium chamber in rabbits. Acta Orthop Scand 60(5):607–610. doi:10.3109/17453678909150132
Cook SD, Dalton JE, Prewett AB, Whitecloud TS, 3rd (1995) In vivo evaluation of demineralized bone matrix as a bone graft substitute for posterior spinal fusion. Spine (Phila Pa 1976) 20 (8):877–886. doi:10.1097/00007632-199504150-00002
Cook SD, Dalton JE, Tan EH, Whitecloud TS, 3rd, Rueger DC (1994) In vivo evaluation of recombinant human osteogenic protein (rhOP-1) implants as a bone graft substitute for spinal fusions. Spine (Phila Pa 1976) 19 (15):1655–1663. doi:10.1097/00007632-199408000-00002
Louis-Ugbo J, Murakami H, Kim HS, Minamide A, Boden SD (2004) Evidence of osteoinduction by Grafton demineralized bone matrix in nonhuman primate spinal fusion. Spine (Phila Pa 1976) 29(4):360–366 discussion Z361
Martin GJ, Jr, Boden SD, Titus L, Scarborough NL (1999) New formulations of demineralized bone matrix as a more effective graft alternative in experimental posterolateral lumbar spine arthrodesis. Spine (Phila Pa 1976) 24(7):637–645
Choi DJAD, Lee SL et al (2008) The effect of demineralized bone matrix as a graft enhancer in posterior lumbar interbody fusion using cage and local bone chips. J Korean Soc Spine Surg 15(3):97. doi:10.4184/jkss.2008.15.3.157
Spivak JM, Hasharoni A (2001) Use of hydroxyapatite in spine surgery. Eur Spine J 10(Suppl 2):S197–S204. doi:10.1007/s005860100286
Chung JMCB, Lee CK, Lee JH et al (2009) Posterior lumbar interbody fusion using hydroxyapatite block—comparison with metal and PEEK cages. J Korean Soc Spine Surg 16(4):7. doi:10.4184/jkss.2009.16.4.243
Burkus JK, Foley K, Haid RW, LeHuec JC (2001) Surgical Interbody Research Group—radiographic assessment of interbody fusion devices: fusion criteria for anterior lumbar interbody surgery. Neurosurg Focus 10(4):E11
Foley KT, Holly LT, Schwender JD (2003) Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 28 (15 Suppl):S26–35. doi:10.1097/01.BRS.0000076895.52418.5E
Schwender JD, Holly LT, Rouben DP, Foley KT (2005) Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech 18(Suppl):S1–S6
Thalgott JS, Giuffre JM, Fritts K, Timlin M, Klezl Z (2001) Instrumented posterolateral lumbar fusion using coralline hydroxyapatite with or without demineralized bone matrix, as an adjunct to autologous bone. Spine J 1(2):131–137
Hwang CJBJ, Koo KH, Lee JH, Yeom JS, Chang BS, Lee CK (2007) A comparative experimental study of allograft and porous hydroxyapatite as bone substitutes. J Korean Orthop Assoc 42:7. doi:10.4055/jkoa.2007.42.4.545
Finkemeier CG (2002) Bone-grafting and bone-graft substitutes. J Bone Joint Surg Am 84-A(3):454–464. doi:10.3923/javaa.2010.1055.1067
Sartoris DJ, Gershuni DH, Akeson WH, Holmes RE, Resnick D (1986) Coralline hydroxyapatite bone graft substitutes: preliminary report of radiographic evaluation. Radiology 159(1):133–137. doi:10.1016/S1067-2516(96)80058-5
Cheng USKD, Cho JL et al (2008) Comparison of the effect of hydroxyapatite and allogeneous bone as an adjunct to autogenous iliac bone grafting in posterolateral spinal fusion. J Korean Orthop Assoc 43:5
Kang HJKT, Kweon SH et al (2011) The usefulness of hydroxyapatite bone transposition in treatment of metaphyseal fracture with bone defect. J Korean Musculoskelet Transpl Soc 11(1):5
Korovessis P, Koureas G, Zacharatos S, Papazisis Z, Lambiris E (2005) Correlative radiological, self-assessment and clinical analysis of evolution in instrumented dorsal and lateral fusion for degenerative lumbar spine disease. Autograft versus coralline hydroxyapatite. Eur Spine J 14(7):630–638. doi:10.1007/s00586-004-0855-5
Bucholz RW (2002) Nonallograft osteoconductive bone graft substitutes. Clin Orthop Relat Res 395:44–52
Boden SD, Martin GJ, Jr., Morone M, Ugbo JL, Titus L, Hutton WC (1999) The use of coralline hydroxyapatite with bone marrow, autogenous bone graft, or osteoinductive bone protein extract for posterolateral lumbar spine fusion. Spine (Phila Pa 1976) 24(4):320–327
Karabekir HS, Gocmen-Mas N, Edizer M, Ertekin T, Yazici C, Atamturk D (2011) Lumbar vertebra morphometry and stereological assesment of intervertebral space volumetry: a methodological study. Ann Anat 193(3):231–236. doi:10.1016/j.aanat.2011.01.011
Pfirrmann CW, Metzdorf A, Elfering A, Hodler J, Boos N (2006) Effect of aging and degeneration on disc volume and shape: a quantitative study in asymptomatic volunteers. J Orthop Res 24(5):1086–1094. doi:10.1002/jor.20113
Riouallon G, Lachaniette CH, Poignard A, Allain J (2013) Outcomes of anterior lumbar interbody fusion in low-grade isthmic spondylolisthesis in adults: a continuous series of 65 cases with an average follow-up of 6.6 years. Orthop Traumatol Surg Res 99(2):155–161. doi:10.1016/j.otsr.2012.12.009
Zairi F, Arikat A, Allaoui M, Assaker R (2013) Transforaminal lumbar interbody fusion: comparison between open and mini-open approaches with two years follow-up. J Neurol Surg A Cent Eur Neurosurg 74(3):131–135. doi:10.1055/s-0032-1330956
Conflict of interest
No conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoo, JS., Min, SH. & Yoon, SH. Fusion rate according to mixture ratio and volumes of bone graft in minimally invasive transforaminal lumbar interbody fusion: minimum 2-year follow-up. Eur J Orthop Surg Traumatol 25 (Suppl 1), 183–189 (2015). https://doi.org/10.1007/s00590-014-1529-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1529-6