Abstract
Purpose
Cauda equina syndrome (CES) may have significant individual consequences if diagnostic delays occur. Our aim was to evaluate the presenting subjective and objective features of patients with suspected CES in comparison to those with radiologically confirmed cauda equina compression (CEC)..
Methods
This was a retrospective analysis of all cases presenting with suspected CES to a tertiary emergency care unit over a two-year period. CEC was defined as radiological confirmation of CEC by Consultant Musculoskeletal (MSK) Radiologist report (MSK-CEC) and by measured canal occupancy due to an acute disc extrusion (> 75%)[measured by a Senior Spinal Surgeon (SP-CEC)]. Routine data collection was compared between categories. Chi square, multivariate regression analyses and ROC analysis of multiple predictors was performed.
Results
530 patients were included in this analysis, 60 (11.3%) had MSK-CEC, and 470 had NO- CEC. Only 43/60 (71.7%) had emergent surgery. Those with MSK-CEC and SP-CEC were statistically more likely to present with bilateral leg pain [(MSK-CEC OR 2.6, 95%CI 1.2, 5.8; p = 0.02)(SP-CEC OR 4.7, 95%CI 1.7, 12.8; p = 0.003)]; and absent bilateral ankle reflexes [(MSK-CEC OR 4.3; 95% CI 2.0, 9.6; p < 0.001)(SP CEC OR 2.5; 95%CI 1.0, 6.19; p = 0.05)] on multivariate analysis. The ROC curve analysis acceptable diagnostic utility of having SP-CEC when both are present [Area under the curve 0.72 (95%CI 0.61, 0.83); p < 0.0001].
Conclusion
This study suggests that in those presenting with CES symptoms, the presence of both bilateral leg pain and absent ankle reflexes pose an acceptable diagnostic tool to predict a large acute disc herniation on MRI scan..
Highlights
The most predictive features of radiological cauda equina compression were bilateral leg pain and absent bilateral ankle reflexes when patients present with other features of suspected CES (including any of urinary, bowel, sexual dysfunction and/or perineal sensory change).
Radiological definitions of cauda equina compression vary across studies making comparisons difficult across existing evidence.
In cases where there is progression of symptoms, in severity, distribution or laterality of symptoms, we would suggest a low threshold for same-day emergency imaging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cauda equina syndrome (CES) includes any combination of back and/or leg pain with one of the following: altered urinary, bowel or sexual function or sensation; and/or sensory changes to the perineal and perianal region [1]. CES is a clinical syndrome, and if any combination of these symptoms is present in the presence of a radiologically confirmed large intervertebral disc or other compressive cause (cauda equina compression [CEC]), then emergency surgery is recommended [2]. CES, although serious, is a rare condition with estimated incidences of 1 in 100 000 in primary care, and around 19% in those presenting with symptoms of CES [3].
In time and resource pressured emergency settings, clinicians need clear guidance on when same day MRI imaging is most likely to result in CEC diagnosis. Previous studies have sought to determine whether any objective or subjective features of assessment were predictive of CEC on MRI scan [4,5,6]. One prospective study found post-void residual bladder volume of more than 200mls had a sensitivity of 94.1% and specificity of 66.8% with predicting a large disc on MRI scan [5]. In contrast, Angus et al., found that bilateral leg pain, dermatomal sensory loss and loss of lower limb reflexes was strongly suggestive of a radiological CEC diagnosis [4]. Pooled data from a systematic review found poor predictive value associated with any objective findings [6]. Few studies have explored the predictive values associated with subjective reporting of CES symptoms and conflicting results exist regarding the predictive values of objective signs [4, 5]. A National UK CES pathway was released in February 2023 to guide decisions on when to perform same day imaging [7]. Prior to these standards, there remained a lack of specialism and resource to manage patients with suspected CES on the frontline, with many patients not receiving MRI scans timeously, or having repeated attendances to the emergency department (ED) [8, 9]. Clinicians seek reassurance of when to perform same day imaging given the variability of patient presentation and the significant impact of medico-legal implications.
CES is a clinical syndrome with 17 different descriptions in the literature, [10, 11] which makes differential diagnoses challenging. Recent studies have highlighted the poor inter-rater reliability in defining radiological CEC [12]. In addition, there is a lack of standardisation of how to define radiological CEC, with some studies using Consultant Radiologist report [4] and others using a measure of more than 75% canal occupancy [13].
In 2020, our NHS Trust implemented a physiotherapist-led acute spinal assessment unit (ASAU) [14, 15]. The service relies on input from the on-call spinal surgical team, liaising with the radiology registrars for same-day imaging, bed managers for admissions, and primary care teams on discharge. When the service was set up, there were no existing pathways or guidance for tertiary care hospitals or emergency departments regarding the management of suspected CES. We developed a clinical pathway using the available evidence from identified literature [4,5,6, 16] in conjunction with our Consultant Surgeon team, and revised this annually, resulting in this project. Our local pathway continues to evolve informed by our dataset. The aim of this project was to identify clinical predictors of subjective and objective features in patients presenting with suspected CES that might help predict MRI scan findings of an acute large canal occupying disc extrusion.
Methods
Study design
A retrospective analysis of a prospectively collected consecutive dataset between January 2020 and July 2021 at an ASAU of a major trauma and tertiary spinal referral centre in the UK, serving a population of 4.5 million. The evaluation was registered with the hospital audit team (220160-C), as it was an observational study, no ethical approval was required. This project is reported in accordance with the STARD guidelines [17](See Supplementary material)
Setting
The ASAU unit was implemented in January 2020, and staffed by an advanced spinal practitioner physiotherapist, health care assistant and spinal nurse. All patients seen on the unit were entered into an online database with information regarding referrer, attending diagnosis, discharged diagnosis, MRI requests and overall outcome (admission or discharge). For those with an admitting diagnosis of suspected CES and available MRI scan, electronic notes were pulled to gather the relevant data for this evaluation. Cases with serious pathology were excluded from this analysis.
Patient cohort and reference standard diagnosis
Patients were included in the evaluation if they were over 18 years of age and had undergone MRI due to suspected CES in the acute spinal pathway. All clinical documentation was reviewed from available records, and in most cases was recorded prior to MRI scan. Data was extracted by the study team (LW and ED) to include demographic data, subjective and objective assessment findings, and time to MRI. Please see Table 1 for categories extracted for subjective and objective features. Categorical data (final diagnosis, subjective and objective findings) was coded accordingly. This was checked by a member of the research team (FK).
Diagnosis of cauda equina compression
CES diagnosis confirmation was based on the MRI scan findings for the study group. Two approaches to the evaluation of the imaging were utilised: the first was based on the formal report of a consultant musculoskeletal (MSK-CEC) radiologist stating “cauda equina compression” [4]. The second definition was based on the imaging interpretation of two senior spinal surgery fellows (SP-CEC)[ME and CZ] for the presence of an acute large (≥ 75%) canal occupying disc extrusion [13].
Data analysis
Descriptive data (counts, percentages, mean and standard deviation (SD)) for all subjective and objective data categories was used to describe the sample. Data for the final diagnosis was collapsed into binary values of MSK-CEC or NO-CEC as well as SP-CEC and NO-CEC and for each of the subjective and objective features (e.g. urinary symptoms yes/ no, bilateral absent ankle reflexes yes or no). The following variables were collapsed into dichotomous (yes/no): bilateral leg pain, sexual dysfunction, perineal sensory change, absent bilateral ankle jerks and PVR > 200 ml. These were compared using a χ-square analysis for the binary values. We considered statistically significant p-values < 0.05. Positive and negative predictive values and sensitivity and specificity scores were calculated for the likelihood of detecting MSK-CEC and SP-CEC.
Univariate logistic regression analysis was carried out to obtain the crude (unadjusted) odds ratios (ORs) for subjective and objective risk characteristics associated with a diagnosis of MSK-CEC and repeated with a diagnosis of SP-CEC. Those demonstrating statistically significant results with the univariate analysis were taken forward to a multivariate analysis to evaluate the independent key predictor variables for MSK-CEC and SP-CEC. 95% confidence intervals (CIs) are reported throughout. We then tested the clinical utility of the combined predictive features, by running a ROC curve analysis to assess the ability to diagnose patients with MSK-CEC and SP-CEC. An area under the curve of 0.5 suggests a lack of ability to diagnose patients with and without MSK- and SP-CEC, 0.7 to 0.8 is considered acceptable, 0.8 to 0.9 is considered excellent, and more than 0.9 is considered outstanding as diagnostic utility [18].
We did not calculate a sample size as this was a service evaluation project and used a sample that was pragmatic. Analysis only including cases with data and numbers for each recorded analysis are recorded throughout. SPSS v27.0 was used for all analyses.
Results
Description of sample
Full data sets were obtained for 530 patients (see Fig. 1 for included cases flow chart). Of these, 60 (11.3%) had MSK-CEC, and 470 had NO-CEC. In contrast, when using a definition of SP-CEC, only 24 cases (4.5%) had SP-CEC and 506 had NO-CEC as seen in Tables 2a and 2b. All cases of SP-CEC were also classified as MSK-CEC. Of those that had MSK-CEC only 43/60 (71.7%), and in SP-CEC, 19/24 (79.2%) proceeded to have surgery emergently.
Flow chart to demonstrate eligible cases and diagnostic accuracy cases used at each stage. Legend SDEC = Same Day Emergency Care unit; MRI = Magnetic Resonance Image; MSK = musculoskeletal; MSK-CEC = Musculoskeletal Radiologist Cauda Equina Compression; No-CEC = No Cauda Equina Compression; SP-CEC = Spinal Fellow Measured canal occupancy Cauda Equina Compression
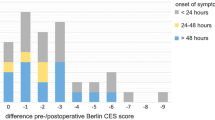
Subjective symptoms
Figure 2 demonstrates the frequency of reported subjective symptoms across all groups of suspected CES with a diagnosis of MSK-CEC and SP-CEC. Chi-square analysis found statistically significant differences between MSK-CEC and NO-CEC in: bilateral leg pain [MSK-CEC (n = 40/60, 66.7%), NO-CEC (n = 186/468, 39.7%)(p = < 0.001) and sexual dysfunction with MSK-CEC (n = 10/35, 28.6%), and NO-CEC (n = 35/281, 12.5%)(p = 0.01). When using a definition of SP-CEC, Chi-square analysis similarly found a statistically significant difference between SP-CEC [bilateral leg pain] (n = 18/24, 75.0%) and NO-CEC (n = 208/504, 41.3%)(p = 0.001); and those reporting sexual dysfunction [SP-CEC (n = 5/13, 38.5%), and NO-CEC (n = 40/303, 13.2%)(p = 0.01)]. See Table 3 for sensitivity and specificity values. Please see Appendix 1 for comparisons of frequency counts across MSK-CEC, SP-CEC and NO-CEC.
Objective signs
Figure 3 demonstrates the reported percentages of objective signs between the NO-CEC and MSK-CEC and SP-CEC groups respectively. Please see Appendix 2 for comparisons of frequency counts across MSK-CEC, SP-CEC and NO-CEC. Chi-square analysis identified the absence of bilateral ankle reflexes [(MSK-CEC n = 23/57, 40.4%; NO-CEC n = 63/439, 14.4%; p < 0.001); (SP-CEC n = 8/23, 34.8%; NO-CEC n = 78/473, 16.5%; p = 0.03)] as statistically significant. ORs for the association between MSK-CEC and NO-CEC for the significant variables in the univariate analyses are presented in Table 4.
Diagnostic test characteristics - multivariate analysis
Those with MSK-CEC and SP-CEC were statistically more likely to present with subjective features of bilateral leg pain [(MSK-CEC OR 2.6, 95%CI 1.2, 5.8; p = 0.02); (SP-CEC OR 4.7, 95%CI 1.7, 12.8; p = 0.003)] and absent bilateral ankle reflexes [MSK-CEC (OR 4.3; 95% CI 2.0, 9.6; p < 0.001); SP-CEC (OR 2.5; 95%CI 1.0, 6.19; p = 0.05)] on multivariate analysis.
The ROC curve analysis (see Fig. 4a and b) demonstrates that when a patient presents with bilateral leg pain and bilateral absent ankle jerks, then the likelihood of having SP-CEC is acceptable [Area under the curve 0.72 (95%CI 0.61, 0.83); p < 0.0001].
Discussion
This evaluation found that the most predictive features of both MSK-CEC and SP-CEC were bilateral leg pain and absent bilateral ankle reflexes presenting with other features of suspected CES. There has been much debate about the management of patients presenting to musculoskeletal services with bilateral leg pain and no other symptoms. UK guidance is clear on the need for same-day imaging when patients present with any combination of new bladder, bowel, sexual dysfunction or perineal sensory change [7]. However, sudden onset of bilateral leg pain or progression of unilateral to bilateral leg pain should be considered as a risk factor for progression of CES, and an urgent MRI scan requested (not same day) [7]. The findings of this paper suggest that when patients present with any other CES features in conjunction with bilateral leg pain and absent ankle reflexes, then a higher level of suspicion should be employed.
This study has demonstrated that although clinical definitions of CEC may vary (MSK-CEC vs. SP-CEC) the predictive findings were the same across both groups. There was considerable debate within our author team about the definition used to determine CEC. This demonstrates the consequences of a radiological definition, as incidence of MSK-CEC and SP-CEC differed, suggesting that an agreed definition is necessary to allow translation into clinical practice. Poor inter-rater reliability between spinal registrars, consultant spinal surgeons and medical students has been recently demonstrated, highlighting the difficulty with diagnosing radiological CEC [12]. Woodfield et al. used a primary definition of more than 50% canal occupancy, and reported 70% of their cohort had more than 75% canal occlusion [19]. Our analysis finds similar results to that of Angus et al. [4] who analysed patient cases from presentation to an emergency village managed by a consultant physiotherapist. They defined CEC using Consultant Radiologist report (as per our MSK-CEC) and found a similar incidence of radiological CEC (111/996, 11%) to our dataset (11.3%), whereas the incidence of SP-CEC was much lower at 4.5%. It is unlikely that patients with 70–75% radiological canal occupancy and symptoms suggestive of CES will not be operated on emergently, and this suggests a need for a working definition based on both radiological and clinical features for more transparent merging of research papers and clinical practice. This may also require additional study to understand the degree of cauda equina nerve compression required to result in symptoms requiring decompressive surgery.
The lower than expected surgical conversion rate between these two groups (MSK-CEC n = 43/60 [71.7%]; SP-CEC 19/24 [79.2%]) may reflect the variability within current practice. Hoeritzauer et al. [13]. reported a surgical conversion of 87% of their CEC cases. Patients may have subtle or stable symptoms as seen in some of our dataset who had fluctuating stable symptoms over a 2–3/month period. Patients may also choose not to have surgery or trial a course of ‘watch and wait’ when symptoms are again variable or intermittent. This highlights the importance of clear safety-netting and shared decision making, using validated tools such as the patient consent forms from the UK National CES pathway [7].
We found similar findings to Angus et al. with bilateral leg pain and absent bilateral ankle reflexes; whereas in contrast, they reported the additional association of dermatomal sensory loss [4]. Previous studies have highlighted the importance of bilateral leg symptoms in early MRI scans, and this study provides additional support for this [20]. Other studies have not found any differences between subjective or objective presenting features in predicting diagnosis of CEC [9].
This study is one of the few to incorporate multivariate modelling in a ROC analysis to compare the clinical utility of multiple predictors. When patients present with symptoms of both bilateral leg pain and absent bilateral reflexes and other CES features, then a high degree of suspicion should be employed in clinical practice. The International Federation of Orthopaedic Musculoskeletal and Manual Physical Therapists’ framework [16] has provided guidance regarding the clinical reasoning process and index of suspicion for cases of suspected red flag pathology such as CES. In cases where there is progression of symptoms, we would suggest a low threshold for same-day emergency imaging.
Across different international health systems there is a drive to standardise how patients with spinal pathology are managed, and the UK National Getting it Right First Time CES pathway is an example of how services or nations may do this [7]. These pathways aim to reduce delays to diagnosis, in particular MRI scanning, for those with suspected CES symptoms. The findings of this evaluation are in keeping with the national UK pathway, as bilateral symptoms alongside a suspicion of CES features were most predictive of MSK-CEC and SP-CEC, suggesting clinicians should be sensitive to changes in patient presentation. Other studies have demonstrated that early diagnosis of CES such as mild symptoms with bilateral features optimises post-surgical recovery. [20] No other country has produced such comprehensive guidance for the assessment and management of suspected CES. The American Association of Neurological Surgeons [21] and Radiologists [22] both have reference to CES imaging and management, but without clarity on what symptoms, within what timeframes should trigger imaging or emergency surgery.
Strengths and limitations
This study has included a large cohort of patients that have routinely presented to an emergency care setting either through self-referral, primary care referral or secondary care review. However, this was a tertiary hospital setting, and so it is possible that more CES cases were seen than would be expected in other settings. However, the retrospective nature of the analysis is limited by incomplete data, and does not include participant outcomes, qualitative insights, or patient involvement. Further, there was no standardisation or uniformity in assessment procedures. Missing data was frequently due to clinician non-recording, and it can be assumed that in those with less severe presentation there may have been innate bias to record or assess less.
Clinical and research implications
Clinical assessment should be supported by a clinical reasoning framework using the clinicians’ index of suspicion and an overall picture of the patient’s general improvement/ worsening/ stability to justify emergency referral and imaging. Further prospective cohort studies with patients presenting with CES symptoms, and patient-reported outcome measures may be useful to validate these findings. Consensus on a radiological definition of CEC will be helpful to define what is meant by CEC and what thresholds should be used for future agreement and meta-analysis of studies.
Conclusion
This study suggests that in those presenting with suspected CES, bilateral leg pain and absent bilateral ankle reflexes are an acceptable diagnostic tool to predict a large acute disc herniation on MRI scan. Further research to standardise the radiological definition of CEC is required to improve the quality and comparability across studies.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Lavy C, James A, Wilson-MacDonald J, Fairbank J (2009) Cauda Equina syndrome. BMJ (Online) 338(7699):881–884 PMID:19336488
British Association of Spine Surgeons, Society of British Neurological Surgeons (2018) Standards of Care for Investigation and Management of Cauda Equina Syndrome
Hoeritzauer I, Wood M, Copley PC, Demetriades AK, Woodfield J (2020) What is the incidence of cauda equina syndrome? A systematic review. J Neurosurg Spine Am Association Neurol Surg 32(6):832–841 PMID:32059184
Angus M, Curtis-Lopez CM, Carrasco R, Currie V, Siddique I, Horner DE Determination of potential risk characteristics for cauda equina compression in emergency department patients presenting with atraumatic back pain: a 4-year retrospective cohort analysis within a tertiary referral neurosciences centre. Emergency Medicine Journal 2021;emermed-2020-210540. https://doi.org/10.1136/emermed-2020-210540
Katzouraki G, Zubairi AJ, Hershkovich O, Grevitt MP (2020) A prospective study of the role of bladder scanning and post-void residual volume measurement in improving diagnostic accuracy of cauda equina syndrome. Bone Joint J Br Editorial Soc Bone Joint Surg 102(6):677–682 PMID:32475252
Dionne N, Adefolarin A, Kunzelman D, Trehan N, Finucane L, Levesque L, Walton DM, Sadi J (2019) What is the diagnostic accuracy of red flags related to cauda equina syndrome (CES), when compared to Magnetic Resonance Imaging (MRI)? A systematic review. Musculoskelet Sci Pract Elsevier Ltd 42:125–133 PMID:31132655
GIRFT (2023) Spinal Surgery: National Suspected Cauda Equina Syndrome (CES) Pathway
Jalloh I, Minhas P (2007) Delays in the treatment of cauda equina syndrome due to its variable clinical features in patients presenting to the emergency department. Emerg Med J 24(1):33–34 PMID:17183040
Hussain MM, Razak AA, Hassan SS, Choudhari KA, Spink GM (2018) Time to implement a national referral pathway for suspected cauda equina syndrome: review and outcome of 250 referrals. Br J Neurosurg Taylor Francis Ltd 32(3):264–268 PMID:29607679
Fraser S, Roberts L, Murphy E (2009) Cauda Equina syndrome: a literature review of its definition and clinical presentation. Arch Phys Med Rehabil Arch Phys Med Rehabil 90(11):1964–1968 PMID:19887225
Lavy C, Marks P, Dangas K, Todd N (2022) Cauda Equina syndrome—a practical guide to definition and classification. Int Orthop Springer Sci Bus Media Deutschland GmbH ; p. 165–169. PMID:34862914
Hoeritzauer I, Paterson M, Jamjoom AAB, Srikandarajah N, Soleiman H, Poon MTC, Copley PC, Graves C, MacKay S, Duong C, Leung AHC, Eames N, Statham PFX, Darwish S, Sell PJ, Thorpe P, Shekhar H, Roy H, Woodfield J (2023) Cauda Equina syndrome: POOR INTER-RATER AGREEMENT FOR DIAGNOSTIC CATEGORIES. Bone and Joint Journal British Editorial Society of Bone and joint surgery. 105(B9):1007–1012 PMID:37652459
Hoeritzauer I, Pronin S, Carson A, Statham P, Demetriades AK, Stone J (2018) The clinical features and outcome of scan-negative and scan-positive cases in suspected cauda equina syndrome: a retrospective study of 276 patients. J Neurol Springer Berlin Heidelberg 265(12):2916–2926 PMID:30298195
Wood L, Dunstan E (2021) A Same Day Emergency Care (SDEC) Unit for Atraumatic Spinal Pain – Preliminary Results. Virtual Britspine
Wood L, Dunstan E (2020) A novel spinal rapid access unit led by advanced spinal physiotherapists to manage urgent spinal presentations. Physiotherapy (United Kingdom)
Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL, Beneciuk JM, Leech RL, Selfe J (2020) International framework for red flags for potential serious spinal pathologies. J Orthop Sports Phys Therapy Mov Sci Media 50(7):350–372 PMID:32438853
Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L, Irwig L, Levine D, Reitsma JB, De Vet HCW, Bossuyt PMM (2016) STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open 6(e012799). https://doi.org/10.1136/bmjopen-2016
Lalkhen AG, Mccluskey A (2008) Clinical tests: sensitivity and specificity. Continuing Education in Anaesthesia. Crit Care Pain 8(6):221–223. https://doi.org/10.1093/bjaceaccp/mkn041
Woodfield J, Hoeritzauer I, Jamjoom AAB, Jung J, Lammy S, Pronin S, Hannan CJ, Watts A, Hughes L, Moon RDC, Darwish S, Roy H, Copley PC, Poon MTC, Thorpe P, Srikandarajah N, Grahovac G, Demetriades AK, Eames N, Sell PJ, Statham PFX, Abdelsadg M, Abulaila MM, Ahmed U, Ajmi Q, Al-Mahfoudh R, Ali C, Amarouche M, Andalib A, Arora M, Arora M, Awan M, Baig Mirza A, Bateman A, Bennett I, Bhatti I, Bodkin P, Bommireddy L, Bonanos G, Borg A, Boukas A, Bourne J, Brennan R, Brown J, Brown K, Burton O, Busby C, Chiverton N, Clark S, Copley PC, Cudlip S, Cunningham Y, Dardis R, Darwish S, Davies B, Demetriades AK, Deore S, Derham C, Dherijha M, Dobson G, Duncan J, Durnford A, Durst AZ, Dyson EW, Eames N, Edlmann E, Edwards-Bailey A, Elserius A, Elson B, Fadelalla M, Fountain DM, Gardner A, Ghosh A, Gill JR, Glasmacher SA, Gordon R, Grahovac G, Grenfell R, Habeebullah A, Haliasos N, Hammett T, Hannan CJ, Hill CS, Hoeritzauer I, Holmes D, Hossain-Ibrahim K, Hughes L, Hussain M, Hussain S, Ibrahim R, Jamjoom AA, John B, Joshi S, Jung J, Kennion O, Khan M, Klejnotowska A, Kumaria A, LaCava R, Lammy S, Lawrence A, Lea M, Leung AH, Liew I, Luo W, MacCormac O, Manfield J, Mannion R, Merola J, Mishra P, Mohmoud KA, Moon R, Morrison R, Murray O, Nader-Sepahi A, Nnandi C, Pandit A, Patel N, Philip A, Poon MT, Prasad KSM, Pronin S, Pujara S, Purushothaman B, Rajwani K, Rasul FT, Roy H, Sadek A-R, Schramm M, Scicluna G, Sell PJ, Shafafy R, Sharma H, Sheikh A, Sivasubramaniam V, Sofela A, Spink G, Srikandarajah N, Statham PF, Stokes S, Strachan E, Thakar C, Thanabalasundaram G, Thorpe P, Ulbricht C, Watts A, Whitcher A, White D, Whitehouse K, Wilby M, Woodfield J, Zolnourian A (2023) Presentation, management, and outcomes of cauda equina syndrome up to one year after surgery, using clinician and participant reporting: a multi-centre prospective cohort study. 24:100545 The Lancet Regional Health - Europe. https://doi.org/10.1016/j.lanepe.2022.100545
Todd NV (2017) Guidelines for cauda equina syndrome. Red flags and white flags. Systematic review and implications for triage. Br J Neurosurg Br J Neurosurg 31(3):336–339 PMID:28637110
Wiseman D, American Association of Neurological Surgeons (2024). Cauda Equina Syndrome. Patient Content. https://www.aans.org/patients/conditions-treatments/cauda-equina-syndrome/ [accessed Jul 11, 2024]
Hutchins TA, Peckham M, Shah LM, Parsons MS, Agarwal V, Boulter DJ, Burns J, Cassidy RC, Davis MA, Holly LT, Hunt CH, Khan MA, Moritani T, Ortiz AO, O’Toole JE, Powers WJ, Promes SB, Reitman C, Shah VN, Singh S, Timpone VM, Corey AS (2021) ACR appropriateness Criteria® Low Back Pain: 2021 update. J Am Coll Radiol Elsevier B V 18(11):S361–S379 PMID:34794594
Funding
This work was not funded.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Lianne Wood, Eleanor Dunstan, Christos Zlatanos, Mohamed Elkazaz and Faris Karouni. The first draft of the manuscript was written by Lianne Wood and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare they have no competing or conflicts of interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wood, L., Dunstan, E., Karouni, F. et al. Can clinical presentation predict radiologically confirmed cauda equina syndrome: retrospective case review of 530 cases at a tertiary emergency department. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08474-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08474-5