Abstract
Study design
Systematic review.
Purpose
Osteoporotic vertebral fractures (OVFs) and degenerative spine conditions are age-related and associated with higher morbidity and mortality and greater health care costs. The relationship between OVFs and prevalent spine degeneration is rarely reported. The aim of this study was to systematically review current literature on the influence of preexisting degenerative spine conditions in patients with OVFs on the occurrence of complications during and after treatment.
Methods
A systematic literature review adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was performed using Web of Science and MEDLINE. We considered English and German articles published from January 1990 to December 2022. The inclusion criteria were patients with OVFs and preexisting spinal degeneration with complications such as subsequent fractures, deformity, implant failure and surgical and general complications. The included studies were controlled trials, cohort studies, and case series.
Results
Ten articles met the inclusion criteria (two prospective studies, seven retrospective studies and one case series). These were divided into two groups: studies on OVFs in patients with coexisting degenerative spine conditions (n = 5) and studies on OVFs following surgical treatment for degenerative spine conditions (n = 5). Three studies reported more complications in patients with OVFs and severe degeneration. One study stated the opposite. One study did not find any correlation. The remaining studies described complications narratively. Subsequent fractures were the most frequent complications.
Conclusion
OVFs in patients with preexisting spinal degeneration seem to cause more complications. In addition to subsequent fractures, other complications have rarely been examined. The presence of degenerative changes or undergoing surgical correction may increase the risk of subsequent fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures are the most common type of osteoporotic fractures and are associated with substantial risks of morbidity and mortality [1]. Osteoporotic vertebral fractures (OVFs) occur in 30–50% of people aged > 50 years [2]. The European Prospective Osteoporosis Study Group reported an OVF incidence of approximately 11/1000 per year in European women and 6/1000 per year in European men [3]. The incidence increases markedly with age regardless of sex. OVFs play an important role from clinical and public health perspectives because of its association with back pain, disability, and impaired health-related quality of life [3].
In addition to osteoporosis, degenerative spine conditions are more prevalent in older adults and are associated with high risks of morbidity and mortality and greater health care costs [4]. These include disc degeneration, scoliosis, spondylolisthesis, and stenosis. In a meta-analysis-based calculation, Ravindra et al. [5] determined that approximately 266 million individuals worldwide (3.6%) are diagnosed with symptomatic degenerative spine diseases every year. Both the incidence and prevalence increased in older populations. For example, a prevalence of > 90% for disc degeneration in patients > 50 years is described [6].
The relationship between osteoporosis and degeneration, in terms of synergistic or antagonistic effects, remains unclear. An inverse relationship has been discussed due to the higher bone mineral density in patients with osteoarthritis [7]. In contrast, other studies claim an association between both conditions. For example, narrowing of the intervertebral disc space has been suggested to increase the risk of OVF [8].
The aim of this study was to systematically review current literature on the influence of preexisting degenerative spine conditions in patients with OVFs on the occurrence of complications, including vertebral fractures, deformity, implant failure, surgical site infection, and general complications.
Methods
A systematic review of the literature was performed, and the study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (registration number: CRD42021249485).
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we conducted a systematic electronic search of Web of Science and MEDLINE for articles written in English and German from January 1990 to December 2022 [9]. The databases were queried using the following search terms: spine AND fracture AND (degenerative OR olisthesis OR scoliosis OR stenosis).
The addressed PI(C)O – question was [10]: “In a population of patients with osteoporotic vertebral fractures (P), do preexisting degenerative changes or their surgical treatment (I), have an influence on the occurrence of complications (O)?”.
Inclusion criteria
-
1.
Studies involving patients with thoracic or lumbar OVFs after no or minor trauma,
-
2.
Studies involving patients with preexisting degenerative changes (including disc degeneration, scoliosis, spondylolisthesis and stenosis).
-
3.
Studies designed as randomized or nonrandomized controlled trials, cohort studies or case series (n ≥ 5).
-
4.
Studies in which the outcome of interest was the occurrence of complications (vertebral fractures, deformity, implant failure, surgical site infection, and general complications).
Exclusion criteria
-
1.
Studies involving patients with pathological fractures, malignancy, spondylodiscitis or high-energy injury,
-
2.
Studies involving patients with cervical spine fractures,
-
3.
Studies written as case reports, case series (n < 5), cadaver studies, technical reports or systematic reviews.
The results from both databases were combined, and duplicate titles were removed. Two reviewers (DW and PP) reviewed articles at each stage of the selection process (titles, abstracts, and full-length articles). During the first steps, disagreement led to inclusion. The references of all the included studies were screened to identify eligible articles.
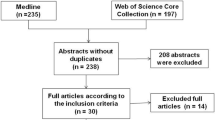
At the final stage of selection, discrepancies were discussed until consensus was reached. A flowchart of the process is shown in Fig. 1.
Search strategy flow diagram in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol [9]
One author (DW) extracted data from the included articles. Study quality was independently assessed by two authors (DW and PP) using the Oxford Centre for Evidence-Based Medicine criteria. Consensus was reached following discussion. Basic information extracted included the title, year of publication, authors, journal title, number of patients, and study design. Specific information extracted included the number and level of fractures, type and stage of degeneration, treatment of the fracture and/or degeneration, and complications that met the inclusion criteria. Due to the heterogeneity of the studies, a meta-analysis was not possible; thus, the results are presented in a narrative form.
Results
Study selection
Ten studies met the inclusion criteria (Tables 1 and 2). The publication dates ranged from 1991 to 2022. Common reasons for exclusion were no primary data, absence of or missing information on osteoporosis or degeneration, no occurrence of spine fracture, and missing information on complications (Fig. 1).
Articles were divided into two groups. Five studies involved patients who were treated for OVFs and had coexisting degenerative spinal conditions. In the remaining five studies, OVFs were treated following surgical treatment for degenerative spinal conditions. Tables 1 and 2 present a tabulated summary of the manuscripts and their relevant results. Table 3 summarizes the treatments and complications.
Patients who were treated for OVF and had coexisting degenerative spine conditions
This group included one case series (n = 8), two retrospective cohort studies, one prospective single-center study and one prospective, multicenter study (Table 1).
Three studies found more complications in patients with acute (proven by MRI) OVFs if there was underlying degeneration.
Sabo et al. [11] described a case series of eight women > 75 years who underwent surgical treatment for OVFs (vertebroplasty or kyphoplasty) and to correct a lumbar scoliotic curve between 6–50°. The measurement of osteoporosis was not further elaborated upon. The presence of lumbar scoliosis led to OVFs and was associated with subsequent OVFs in the following months (n = 8/8), sacral insufficiency fractures (n = 3/8) and other fractures (n = 3/8). No threshold for the severity of scoliosis was defined, and the authors reported that 38% (n = 3) of patients had scoliosis > 20°. Based on their findings, the authors recommended medication for osteoporosis, early treatment for fractures affecting the coronal profile, and augmentation of adjacent vertebrae.
Oishi et al. [12] identified coexisting degenerative spondylolisthesis at the OVF level as a risk factor for the occurrence of neurological deficits. Patients with neurological deficits had a significantly higher frequency of coexisting degenerative spondylolisthesis at the affected disc level than those without neurological deficits (50% [11/22] vs. 13%, [11/82], p < 0,005) [12]. Coexisting degeneration and neurological symptoms depended on the signal intensity in the T1W MR images. The bone mineral density (BMD) of the hip was measured using dual-energy X-ray absorptiometry (DXA). OVFs indicated by total low intensity might have had increased bone fragility compared to those with OVFs indicated by superior/inferior low intensity. However, OVFs indicated by superior/inferior low intensity on T1W MR images was more often associated with coexisting degenerative spondylolisthesis than OVFs indicated by total low intensity (26.3% [6/28] vs. 21.4% [15/57]) and resulted more often in the occurrence of neurological symptoms.
In a single-center prospective study, Estublier et al. [4] analyzed the relationship between disc degeneration and acute fragility fractures in men. Disc degeneration was defined using a four-point scale based on the severity of disc space narrowing. Of the 765 men, 64 had a preexisting OVF. The BMD of the hip and the spine were measured using DXA.
In 659 men with follow-up radiographs, 28 incident vertebral fractures occurred in 27 men over 7.5 years. They concluded that severe disc degeneration is accompanied by higher spinal bone mineral density and an increased risk of vertebral fractures.
In contrast, in a multicenter prospective study, Rahmani et al. [13] described that fracturing of the endplate and less disc degeneration were risk factors for non-union of OVFs. They classified preexisting disc degeneration into eight groups based on the modified Pfirrmann grading system, considering nucleus signal intensity, distinction between the inner and outer fibers of the annulus, and posterior aspects of disc and disc height. DXA has been used to measure the BMD of the hip. Existing disc degeneration appears to be associated with higher BMD. However, the relationship between BMD, degeneration, and OVFs has not been further analyzed. The patients were treated conservatively with corsets (96%) and teriparatide (14%). Delayed union at the 6-month follow-up could be seen in 27 cases (19%). They discussed a higher motion level of a healthier disc as a risk factor for poor fracture healing.
Ross et al. [14] found no association between preexisting degeneration and OVFs. Of the 897 women, 61 had at least one preexisting OVF. Twenty-four (6.6%) patients sustained subsequent fractures during an average follow-up of 4.7 years. Spinal degeneration (osteoarthritis, spondylolisthesis, disc degeneration, and scoliosis), whether absent or present, did not have a significant influence. Notably, Ross et al. [14] solely investigated radiographs and not magnetic resonance images. They found that poor bone mass and the number of vertebral fractures were risk factors for subsequent fractures. A difference of two standard deviations (SD) in bone mass led to a rate ratio of 3-4.4 for a new OVF. Therefore, the authors recommended a systemic treatment for osteoporosis.
Occurrence of OVF following surgical treatment for degenerative spine conditions
This group included five retrospective cohort studies (Table 2). The studies involved patients with degenerative spine diseases and OVF and listed complications without investigating further interactions or conclusions.
Hayashi et al. [15] retrospectively analyzed the outcome of posterior lumbar interbody fusion (PLIF) for spinal canal stenosis, spondylolisthesis or degenerative lumbar scoliosis. Twelve of 96 (12.5%) patients had preexisting acute OVFs, and 18 (19%) patients presented with a newly identified postoperative OVF.
The method for measuring osteoporosis was not further elaborated upon. Overall, perioperative complications (anemia, cardiopulmonary, gastrointestinal or urinary tract infections) were identified in 16 patients (17%), surgery-specific complications (dural tear, hematoma, neurologic deficit, infection, implant failure, non-union, and adjacent segmental degeneration) occurred in 22 patients (23%), major complications (blood transfusion, additional antibiotics, treatment by another department) were noted in 11 patients (11.5%), and revision surgery was required in seven patients (7%). Liao and Chen [16] found significantly more preoperative OVFs (10.5% [4/38] vs. 2.6% [1/38]) and postoperative OVFs (13.2% [5/38] vs. 2.6% [1/38]) in patients older than 80 years after instrumented surgery for degenerative lumbar spondylolisthesis. In the group of patients aged ≥ 80 years, five postoperative complications were described: implant loosening (1 case), pneumonia (1 case), urinary tract infection (1 case) and wound infections (2 cases). The description of how osteoporosis was measured and the exact timing of the OVFs lack further detail.
In a retrospective study, Yang et al. [17] investigated the treatment options for urgent adjacent OVFs occurring after lumbar instrumented fusion for degenerative diseases in 23 patients. The BMD of the spine was measured using DXA. The BMD at the cranial level to fusion decreased time-dependent. All fractures were treated with percutaneous vertebroplasty. In addition to cement leakage in four patients, no surgery-related complications were reported. Two patients had new fractures within nine months: one was treated conservatively, and the other underwent vertebroplasty.
Kim et al. [18] retrospectively reviewed the data of 201 patients who underwent instrumented arthrodesis for degenerative lumbar disorders. Twenty-five patients suffered a subsequent OVF, which was associated with an aggravation of back pain. DXA has been utilized to measure the hip’s BMD, revealing a negative correlation with back pain. Lee et al. [19] compared the efficacy of non-operative treatment in comparison with decompression surgery in patients with lumbar spinal stenosis in a retrospective study. In the conservative group, 14/36 (39%) patients had a preexisting OVF, and 17/59 (29%) had a preexisting OVF in the surgery group. Preexisting OVFs did not influence the choice of treatment. The surgery group showed a greater decrease in the risk of falling, which did not correlate with the existing OVFs. The measurement of osteoporosis and the exact timing of the OVFs were not further expounded upon.
Discussion
In summary, regarding the relationship between OVF and spine degeneration, the occurrence of complications other than subsequent OVF has rarely been examined. The presence of degenerative changes or surgical correction may increase the risk of a subsequent fracture. Despite the paucity of available data, most authors concurred with the essential role of osteoporosis therapy.
To the best of our knowledge, this is the first systematic review investigating the relationship between OVF and spinal degenerative changes that influence the occurrence of complications.
The search terms were generally worded to ensure the inclusion of all potentially relevant articles, which led to a high number of potentially suitable articles (n = 3738). Owing to the small number of remaining articles, we included studies involving patients who sustained an OVF after degeneration surgery as a second group.
Literature on the relationship between OVFs and spine degeneration has shown a middle-rate level of evidence (LoE). Two prospective studies were included. Interestingly, they contradict each other. Rahmani et al. [13] described endplate failure and less disc degeneration as risk factors for non-union of OVFs. They suggested that endplate damage may trigger a pathological cascade that leads to adjacent disc degeneration. On the other hand, a healthier disc seemed to be associated with a higher range of motion and therefore could lead to a higher rate of bony non-union. Estublier et al. [4] assumed that severe disc degeneration mimics a higher bone mineral density but increases the risk of subsequent OVF. Furthermore, they discussed that spinal degeneration is associated with sarcopenia, poor proprioception, pain and postural instability and could lead to a higher risk of falls, thereby causing more OVFs.
Among the studies with lower LoE, two corroborated the findings of Estublier et al. [4] by demonstrating an association between severe degeneration and a higher incidence of OVFs [11, 12]. Oishi et al. [12] distinguished a correlation between degeneration and OVFs in patients with neurological deficits. Ross et al. [14] did not observe any influence from one to another. This could be attributed to the exclusive use of radiographs and the absence of MRI images for analysis. The remaining studies did not mention interdependence. The data did not indicate whether preexisting OVFs are a risk factor for postoperative complications.
The most frequently examined complication was the occurrence of subsequent vertebral fractures in eight out of ten studies. Except for two studies, most studies solely described the appearance of a subsequent OVF without providing further explanation. In their small study, Sabo et al. [11] (LoE IV) hypothesized that the acceleration of degeneration increases the risk of new fractures.
Three studies described a resulting deformity, three studies described material failure, five studies described surgical complications, and four studies described non-fracture-associated complications (Table 3).
Additionally, seven studies considered the worsening of pain and mobility. Two studies indicated worse clinical outcomes if OVFs occurred after surgery for degenerative conditions [15, 18]. In summary, most of the included studies showed that patients with both OVFs and preexisting spinal degeneration appeared to have more complications. However, most complications have been described descriptively without further discussion on their relationship with OVF and degeneration.
Furthermore, Liao and Chen [16] reported an increased incidence of complications in older patients (> 80 years). It should be considered that advanced age associated with a higher prevalence of comorbidities could contribute to the increased occurrence of complications and to a greater degree of degeneration. Therefore, patient age should be considered as a separate surrogate parameter.
DXA was the predominant method for measuring the BMD of the hip and/or spine [4, 12,13,14, 17, 18]. Overall, a decreased BMD is associated with a higher number of OVFs. Two studies postulated that spinal degeneration is associated with a higher BMD of the spine [4, 13]. Therefore, the measurement of spinal BMD appears to be less informative in the presence of degeneration. Supplementing the measurement at the hip should be considered.
Yang et al. described a decrease in BMD at the cranial level to fusion. This could be an explanation for the occurrence of adjacent OVFs after surgical treatment. The remaining studies did not comment on the relationship between degeneration, BMD, and OVFs. Four studies did not describe the measurement of osteoporosis at all [11, 15, 16, 19]. Six studies drew conclusions regarding the treatment of patients with OVF and degeneration. Ross et al. [14] and Hayashi et al. [15] highlighted the importance of systemic osteoporosis treatment.
Sabo et al. [11] and Yang et al. [17] made contradictory recommendations regarding prophylactic vertebroplasty. Sabo et al. [11] suggested performing them more often, while Yang et al. [17] advised against it; however, they only described four cases of asymptomatic cement leakage. Both studies showed a low LoE (IV and IIIB).
In addition to the included studies, Wang et al. [20] discussed the association between osteoporosis and OVFs to increase disc degeneration based on two of their own large prospective multicenter studies. However, the sources did not contain any individual studies that directly focused on a patient population with osteoporotic fractures and degeneration coexisting. The study itself was not included in our analysis, as it was a systematic review.
This systematic review was limited by the heterogeneity and quality of available evidence regarding the specific questions of this review. In part, conflicting statements regarding complications and conclusions regarding treatment have been made.
Further studies are necessary to identify patients who would likely benefit more from conservative therapy than surgery, as well as to determine which surgical strategy should be applied to reduce the incidence of complications.
Conclusion
Overall, the few available studies have a low level of evidence.
Patients with both OVF and preexisting spinal degeneration seemed to have more complications. Subsequent fractures were the most frequently analyzed and found complications. However, other complications have been rarely examined. The presence of non-disc-specific degenerative changes or their surgical correction may increase the risk of subsequent fracture. Despite the scarcity of data, most authors agree on the importance of osteoporosis therapies.
Data availability
All data analysed during this study are included in this published article.
References
Schousboe JT (2016) Epidemiology of vertebral fractures. J Clin Densitom 19:8–22. https://doi.org/10.1016/j.jocd.2015.08.004
Ballane G, Cauley JA, Luckey MM, Fuleihan GEH (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28:1531–1542. https://doi.org/10.1007/s00198-017-3909-3
Felsenberg D, Silman AJ, Lunt M et al (2002) Incidence of vertebral fracture in europe: results from the European prospective osteoporosis study (EPOS). J Bone Min Res 17:716–724. https://doi.org/10.1359/jbmr.2002.17.4.716
Estublier C, Chapurlat R, Szulc P (2017) Older men with severe disc degeneration have more incident vertebral fractures-the prospective MINOS cohort study. Rheumatology (Oxford) 56:37–45. https://doi.org/10.1093/rheumatology/kew327
Ravindra VM, Senglaub SS, Rattani A et al (2018) Degenerative lumbar spine disease: estimating global incidence and worldwide volume. Global Spine J 8:784–794. https://doi.org/10.1177/2192568218770769
Teraguchi M, Yoshimura N, Hashizume H et al (2014) Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthritis Cartilage 22:104–110. https://doi.org/10.1016/j.joca.2013.10.019
Dequeker J, Aerssens J, Luyten FP (2003) Osteoarthritis and osteoporosis: clinical and research evidence of inverse relationship. Aging Clin Exp Res 15:426–439. https://doi.org/10.1007/bf03327364
Sornay-Rendu E, Allard C, Munoz F, Duboeuf F, Delmas PD (2006) Disc space narrowing as a new risk factor for vertebral fracture: the OFELY study. Arthritis Rheum 54:1262–1269. https://doi.org/10.1002/art.21737
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Farrugia P, Petrisor BA, Farrokhyar F, Bhandari M (2010) Practical tips for surgical research: research questions, hypotheses and objectives. Can J Surg 53:278–281
Sabo A, Hatgis J, Granville M, Jacobson RE (2017) Multilevel contiguous osteoporotic lumbar compression fractures: the relationship of scoliosis to the development of cascading fractures. Cureus 9:e1962. https://doi.org/10.7759/cureus.1962
Oishi Y, Nakamura E, Murase M et al (2019) Lower lumbar osteoporotic vertebral fractures with neurological symptoms might have two different pathogeneses according to early magnetic resonance images. Acta Neurochir (Wien) 161:2211–2222. https://doi.org/10.1007/s00701-019-04045-6
Rahmani MS, Takahashi S, Hoshino M et al (2018) The degeneration of adjacent intervertebral discs negatively influence union rate of osteoporotic vertebral fracture: a multicenter cohort study. J Orthop Sci 23:627–634. https://doi.org/10.1016/j.jos.2018.03.008
Ross PD, Davis JW, Epstein RS, Wasnich RD (1991) Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med. https://doi.org/10.7326/0003-4819-114-11-919. 114:919 – 23
Hayashi K, Matsumura A, Konishi S, Kato M, Namikawa T, Nakamura H (2016) Clinical outcomes of posterior lumbar interbody fusion for patients 80 years of age and older with lumbar degenerative disease: minimum 2 years’ follow-up. Global Spine J 6:665–672. https://doi.org/10.1055/s-0036-1578806
Liao JC, Chen WJ (2018) Surgical outcomes in the elderly with degenerative spondylolisthesis: comparative study between patients over 80 years of age and under 80 years-a gender-, diagnosis-, and surgical method-matched two-cohort analyses. Spine J 18:734–739. https://doi.org/10.1016/j.spinee.2017.08.250
Yang SC, Chen HS, Kao YH, Tu YK, Liu K, Cheng HC (2013) Clinical evaluation of percutaneous vertebroplasty for symptomatic adjacent vertebral compression fracture. J Spinal Disord Tech 26:E130–E136. https://doi.org/10.1097/BSD.0b013e318278577f
Kim BH, Choi DH, Jeon SH, Choi YS (2010) Relationship between new osteoporotic vertebral fracture and instrumented lumbar arthrodesis. Asian Spine J 4:77–81. https://doi.org/10.4184/asj.2010.4.2.77
Lee BH, Kim TH, Park MS et al (2014) Comparison of effects of nonoperative treatment and decompression surgery on risk of patients with lumbar spinal stenosis falling: evaluation with functional mobility tests. J Bone Joint Surg Am 96:e110. https://doi.org/10.2106/jbjs.m.00427
Wáng YXJ, Deng M, Griffith JF et al (2022) Healthier Chinese spine’: an update of osteoporotic fractures in men (MrOS) and in women (MsOS) Hong Kong spine radiograph studies. Quant Imaging Med Surg 12:2090–2105. https://doi.org/10.21037/qims-2021-07
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Professor Christoph-Eckhard Heyde and Professor Georg Osterhoff had the idea for the article. All authors contributed to the study conception and design. Dr. Dina Wiersbicki and Dr. Philipp Pieroh performed the literature search and data analysis. The first draft of the manuscript was written by Dr. Dina Wiersbicki. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This article is a systematic review. This article does not contain any studies with human participants or animals performed by any of the authors.
As far as the authors can ascertain, the studies have been approved by the appropriate institutional or national research ethics committee and have been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Consent to participate
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wiersbicki, D.W., Osterhoff, G., Heyde, CE. et al. The relation of osteoporotic vertebral fractures and spine degeneration on the occurrence of complications: a systematic review. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08403-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08403-6