Abstract
Purpose
Practice-based research networks are collaborations between clinicians and researchers to advance primary care research. This study aims to assess the feasibility for longitudinal data collection within a newly established chiropractic PBRN in Switzerland.
Methods
A prospective observational cohort feasibility study was performed. PBRN participating chiropractors were asked to recruit patients seeking new conservative health care for musculoskeletal pain from March 28, 2022, to September 28, 2022. Participants completed clinically oriented survey questions and patient-reported outcome measures before the initial chiropractic assessment as well as 1 h, 2 weeks, 6 weeks, and 12 weeks thereafter. Feasibility was assessed through a variety of process, resource, and management metrics. Patient clinical outcomes were also assessed.
Results
A total of 76 clinicians from 35 unique primary care chiropractic clinics across Switzerland participated. A total of 1431 patients were invited to participate, of which 573 (mean age 47 years, 51% female) were enrolled. Patient survey response proportions were 76%, 64%, 61%, and 56%, at the 1-h, 2-, 6-, and 12-week survey follow-ups, respectively. Evidence of an association was found between increased patient age (OR = 1.03, 95%CI 1.01–1.04), patient from a German-speaking region (OR = 1.81, 95%CI 1.17–2.86), non-smokers (OR = 1.89, 95%CI 1.13–3.17), and increased pain impact score at baseline (OR = 1.18, 95%CI 1.01–1.38) and response to all surveys.
Conclusion
The Swiss ChiCo pilot study exceeded its prespecified feasibility objectives. Nationwide longitudinal data capture was highly feasible. Similar to other practice-based cohorts, participant retention remains a challenge.
Trial registration Swiss chiropractic cohort (Swiss ChiCo) pilot study (ClinicalTrials.gov identifier: NCT05116020).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Practice-based research networks (PBRNs) are a concept that originated with the expansion of the primary care medical specialty in the 1960s [1]. PBRNs are defined as groups of at least 15 ambulatory practices devoted to the care of patients and affiliated by a mission to investigate questions related to community-based practice [2]. Although all PBRNs share common overarching characteristics, how data are collected can differ. The Family Medicine ICPC-Research using Electronic Medical Records (FIRE) project is a registry-based PBRN whereby clinicians are linked through an electronic record system [3]. Alternatively, the Australian Chiropractic Research Network (ACORN) used a sub-study PBRN model for data collection [4, 5]. In sub-study PBRN models, clinicians willing to participate in research activities are identified. After a clinician roster is established, nested sub-studies are supported by these clinicians [6]. This approach is described as the more flexible PBRN model, as projects do not have to comply with a rigid patient management system [6]. However, the promise of this flexibility has yet to be comprehensively tested [7,8,9].
In 2021, our research team launched a sub-study-based Swiss chiropractic PBRN [10, 11]. The aim of this current study was to assess the feasibility of conducting a nationwide prospective cohort study from this novel PBRN. Feasibility was assessed through a variety of process, resource, and management metrics [12]. Patient clinical outcomes were also explored.
Materials and methods
We reported this study according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement and the Consolidated Standards of Reporting Trials (CONSORT) extension to randomized feasibility trials (Supplemental File 1 and 2) [13,14,15].
Setting
Chiropractic in Switzerland is a medical profession that focuses on the management of musculoskeletal (MSK) disorders. Swiss chiropractors can be consulted directly without physician referral [16]. Summary of the Swiss chiropractic PBRN is provided in our published report [11]. Study onboarding sessions were organized with PBRN clinicians motivated to participate in patient recruitment for this study. When possible, other clinicians and front desk staff participated.
Design and feasibility
The Swiss ChiCo pilot study was a 12-week prospective cohort pilot study of adults seeking new conservative care for MSK pain and conducted from March 28, 2022, to January 6, 2023. Swiss chiropractors endorsed that it would be feasible to recruit 5–10 patients per clinician. Based on clinician feedback and published reports, we aimed to recruit a minimum of 15 clinics [2, 17]. It was deemed feasible to expand the Swiss ChiCo pilot study if 100 patients were enrolled across 15 unique practices. We requested solo clinics (one clinician) to consecutively recruit 10 patients and group clinics (≥ 2 clinicians) to consecutively recruit at least five patients per participating clinician.
The primary feasibility objectives were to assess: (1) the proportion of chiropractic patients who were invited and agreed to participate and (2) patient participant follow-up and retention across 12 weeks. Primary clinical objectives at the patient level included: (1) pain impact over 12 weeks (measured by the pain, enjoyment, and general activity (PEG) scale) and (2) musculoskeletal health status over 12 weeks (measured by the musculoskeletal health status questionnaire (MSK-HQ)) [18, 19]. Further information on study outcomes is provided in the published study protocol [10].
Clinician and patient participants
All chiropractors were eligible to participate in patient recruitment. Clinicians from the PBRN that endorsed motivation to participate in this patient pilot study were initially contacted [11]. Through snowball recruitment, a clinician that endorsed motivation was able to recruit other chiropractors both within and outside the PBRN to participate.
Patients were eligible to participate if they were 18 years or older, seeking new conservative care for a MSK pain complaint, and were able to respond to study questionnaires in either German, French, Italian, or English. New conservative MSK care was defined as not having received chiropractic, massage therapy, osteopathy, or physiotherapy for the MSK complaint within the past month and not being a follow-up visit.
Data collection procedures
Data were collected through questionnaires using the Research Electronic Data Capture (REDCap) web application [20]. After an electronic consent, patients forwarded to the first study survey (baseline). This survey was completed prior to the initial chiropractic consultation via a study tablet. Subsequent surveys were emailed directly to patients 1 h after the completion of the baseline survey (post-initial consultation) and at 2, 6, and 12 weeks thereafter. Patients who completed informed consent and at minimum partially completed the baseline questionnaire (defined as providing information on at least one clinical outcome) were considered enrolled. We retrospectively contacted clinics to populate missing information on the variables of “sex” and “nationality” for patients who had dropped out between the baseline and post-initial consultation time points. Electronic survey reminders were implemented to reduce survey nonresponse.
Participating clinics received an individualized monthly clinic report which provided recruitment totals and aggregate clinical outcome metrics on their patients. Patient participants received individualized feedback patient reports after their 6- and 12-week survey time points. The patient reports provided information on clinical outcomes collected at baseline and at 6- and 12-week follow-up. Example reports are provided in Supplemental File 3 and 4.
Variables and outcome measures
Clinician and clinic level information
Information collected on participant clinicians include sex, age, language, licensure status, years of practice, and affiliation status in the Swiss chiropractic PBRN. The years of practice variable were derived from the register of medical professions in Switzerland (MedReg) [21].
Variables collected from clinics included address, number of participant chiropractors within practice, front desk staff presence at the onboarding session, number of days from onboarding to study initiation, patient recruitment start date, patient recruitment end date, number of new patients or returning–new patients visits each month, and recruitment target performance.
Patient-level information
The baseline questionnaire contained information on patient age, language, pain impact prior to visit (PEG scale), MSK health status (MSK-HQ), and question 9 of the brief illness perception questionnaire (Brief IPQ) [18, 19, 22].
The post-initial consultation collected information on participant characteristics, injury characteristics, and patient-reported outcome measures such as the PEG scale, MSK-HQ, and the Örebro musculoskeletal pain screening questionnaire short (OMPSQ-short) [18, 19, 23]. Questions on how the COVID-19 pandemic had impacted patient quality of life, physical activity, and ability to seek medical treatment were also included.
Subsequent patient surveys at 2-, 6-, and 12-week follow-up had a standardized design which focused on clinical course of MSK pain. Response to a follow-up survey was conceptualized as either partial response (operationalized as completion of at least one clinical outcome measurement) or full response (fully completing all questions in a follow-up survey). At each follow-up, patients were asked about clinical care/course characteristics. Patient-reported outcome measures of the PEG scale, MSK-HQ, and patients’ global impression of change (PGIC, score range 1 (completely recovered) to 7 (worse than ever)) were also asked [18, 19, 24].
Statistical analysis
All data were extracted from REDCap into R (version 4.2.2). The prespecified statistical analysis plan is provided in Supplemental File 5. Participant clinician, clinic, and patient characteristics were described. Clinics that met recruitment targets (set at 10 patients in a solo practice and five patients/participating clinician in a group practice) were categorized as achieving target recruitment. Patient participant retention and response times were described with 95% confidence intervals (95%CIs). Patient characteristics of respondents and non-respondents to each follow-up questionnaire were compared descriptively. Average monthly recruitment rate across all clinics was defined as the individual clinic-specific recruitment rate per month divided by the maximum number of recruitment clinics [25].
Multivariable logistic regression was used to assess factors associated with clinic recruitment target achievement. Independent variables included in this model were language region (German, French, and Italian), front desk staff presence at onboarding session (no and yes), motivation of primary clinician contact to participate, delay between onboarding session and patient recruitment (> 2 weeks and ≤ 2 weeks), and practice size (group and solo).
Mixed effects logistic regression analysis with clinic set as a random intercept was used to investigate factors associated with patient response to all study surveys. Predictor variables included patient age, sex, smoking status (current smokers and non-smokers), language region (German, French, and Italian), PEG score collected at baseline, MSK-HQ score collected at baseline, medication use for pain (yes and no), duration of complaint (> 30 days and ≤ 30 days), and OMPSQ-short. Variables included were based on respondent analyses conducted from chiropractic cohorts and clinical reasoning [17, 26]. Results of both logistic regression analyses were presented as ORs with 95%CIs.
Results
Characteristics of clinicians and clinics
A total of 59 chiropractors in 46 clinics endorsed being motivated to participate [11]. A total of 35 clinics and 76 clinicians were included in our study (see Supplemental File 6). The typical participating clinician had a median age of 44 years, was female, and spoke German. In total, 71% of clinicians were participants in the Swiss chiropractic PBRN [11]. Clinician characteristics are provided in Table 1.
Participant clinicians practiced in 35 unique clinics across Switzerland. A majority of clinics were group practices. Clinic front desk staff participated in study onboarding sessions in approximately 30% of clinics. The majority of clinics began patient recruitment within 2 weeks of onboarding.
Clinics participated in patient recruitment for an average of 3.5 months. Nine out of 10 patients were recruited within the first 3 months (Supplemental File 7). The average recruitment rate was 5.3 patients per clinic per month. This ranged from a low of 0.33 to a high of 17.67 patients recruited per month. Figure 1 provides an overview of clinic recruitment rates across Swiss regions. In total, 20 clinics (57%) met the target recruitment goal. Participating clinic characteristics are provided in Table 2. Evidence of an association was found between solo practice size and meeting recruitment goal (OR = 9.85, 95%CI 1.6–100.7) referent to group practices, while clinics from German-speaking regions were less likely to meet their recruitment goals (OR = 0.13, 95%CI 0.01–0.82) (Supplemental File 8).
Characteristics of patients
Patients were recruited from March 28, 2022, to September 28, 2022, with the final patient survey collected on January 6, 2023. Figure 2 details patient participant recruitment and flow. A total of 8265 candidate study patients visited a participating clinic during the study recruitment period. A total of 1431 patients were deemed potentially eligible and invited to participate, of which 846 expressed initial interest after reading the study information form. See Supplemental File 9 for reasons for non-interest. Our final study population was 573 patients who completed informed consent and at least partially completed the baseline questionnaire. Of the 573 enrolled participants, 434 (76%) completed the post-initial consultation survey, 369 (64%) completed the 2-week, 350 (61%) completed the 6-week, and 322 (56%) completed the 12-week follow-up surveys. Average response times varied from 2 days for the baseline survey to 7 days for the 12-week survey. Supplemental File 10 provides additional response time information.
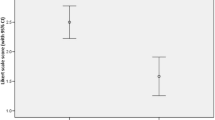
Table 3 provides information about baseline patient characteristics. Patient participants were more commonly female, had an average of 47 years, and were German speakers (60%). The most common MSK pain location was low back pain (41%). Duration of pain was most commonly reported as between 2 weeks and 3 months (31%), followed by more than 12 months (29%). Almost 40% of patients reported using pain medication. Patients reported an average PEG scale score of 5.1 and an average MSK-HQ score of 32.0 prior to their appointment. Table 4 provides information on patient characteristics at follow-up time points. At the 12-week follow-up time point, patients had an average PEG score of 2 (95%CI 1.7–2.1) and MSK-HQ score 45 (95%CI 44.0–46.1). Figure 3 and Supplemental File 11 provide further information on clinical outcomes. Supplemental File 12 provides information on COVID-19 collected variables.
Respondents to follow-up questionnaires were older and proportionally more female than non-respondents (Supplemental File 13). Evidence of an association was found between older age and response to all survey questionnaires (OR = 1.03, 95%CI 1.01–1.04), German language region (OR = 1.81, 95%CI 1.17–2.86) referent to French- and Italian-speaking regions, non-smoker status (OR = 1.89, 95%CI 1.13–3.17) referent to smokers, and increased PEG scale total score at baseline (OR = 1.18, 95%CI 1.01–1.38). Supplemental File 14 provides an overview of this regression model.
Discussion
In this study, we report the feasibility of conducting a nationwide cohort study within the Swiss chiropractic PBRN. Of the 1431 patients invited, 40% were enrolled. Patient response was 76%, 64%, 61%, and 56% for the 1 h, 2-, 6-, and 12-week follow-up time points, respectively. With a total of 35 participant clinics and 573 enrolled patients during a study recruitment period of 6 months, the Swiss ChiCo pilot study exceeded its feasibility objectives.
Significance of findings—clinician and clinic level
Overall, 76 clinicians within 35 clinics participated in patient recruitment. Compared to group practices, solo practitioner clinics had higher odds of reaching target patient enrollment. Solo practitioners have been shown to participate less in voluntary research when compared to clinicians within-group practices [27]. In this study, solo practitioner clinics were a strong resource for patient recruitment. It can be hypothesized that the reduced patient flow at smaller clinics allows more time to introduce a study effectively. Clinic organizational processes (recruitment workload), study methods (clinical relevance and pragmatic methods), and clinicians (doctor–patient relationship) all play a crucial role in the recruitment of patients [28, 29]. Clinicians can be aided by simplifying recruitment methods, providing extra staffing, or providing compensation for protected research time [28, 30].
Significance of findings—patient level
The average clinic-specific patient recruitment rate for the Swiss ChiCo pilot study was 5.3 patients/month. Patient retention after 12 weeks was reported at 56%, with older patients, patients from German-speaking regions, non-smokers, and those with higher pain impact scores at higher odds to complete all study questionnaires. Well-documented challenges to observational research include participant recruitment and follow-up retention [31]. Poor recruitment and retention can impact the diversity of the patient sample and ability for a study to draw meaningful conclusions [32]. The use of decentralized clinical research methods can add flexibility to data collection methods and reduce participant burden [33,34,35]. Decentralized methods employed in the Swiss ChiCo pilot study included the use of electronic screening and informed consent, recruitment from a diverse group of clinics, and electronic participant feedback.
Strengths and limitations
This study has several strengths. First, the study methodology was developed through consultation with stakeholders. Second, the study protocol was published and registered. Third, participants were recruited across Switzerland. This study has several limitations. First, consecutive patient recruitment may not have occurred in all clinics. Consecutive recruitment prevents sampling bias. Second, all data were collected through self-report and subject to recall bias. Third, patients did not enter this study at a true “time origin” entry point with regard to MSK pain onset which is typical of an inception cohort study. This decision was made to aid in patient recruitment.
Conclusions
The Swiss ChiCo pilot study demonstrates feasibility for nationwide longitudinal patient data capture from a sub-study-based PBRN. The project was guided by stakeholder engagement activities conducted with clinicians, patients, and organizational partners. Similar to other practice-based studies, consecutive recruitment and participant retention over time was challenged.
Data availability
Data from the Swiss Chiropractic PBRN and the Swiss ChiCo pilot study will be made available for research purposes. Requests, including a synopsis of the study plan, can be addressed to the corresponding author.
References
Green LA, Hickner J (2006) A short history of primary care practice-based research networks: from concept to essential research laboratories. J Am Board Fam Med 19(1):1–10. https://doi.org/10.3122/jabfm.19.1.1
Agency for Healthcare Research and Quality, Rockville, MD. Primary care practice-based research networks. Published October 2018. Accessed September 20, 2021. https://www.ahrq.gov/research/findings/factsheets/primary/pbrn/index.html
Chmiel C, Bhend H, Senn O et al (2011) The FIRE project: a milestone for research in primary care in Switzerland. Swiss Med Wkly 140:w13142. https://doi.org/10.4414/smw.2011.13142
Adams J, Steel A, Chang S et al (2015) Helping address the national research and research capacity needs of Australian chiropractic: introducing the Australian chiropractic research network (ACORN) project. Chiropr Man Ther 23(1):12. https://doi.org/10.1186/s12998-015-0057-8
Adams J, Peng W, Steel A et al (2017) A cross-sectional examination of the profile of chiropractors recruited to the Australian chiropractic research network (ACORN): a sustainable resource for future chiropractic research. BMJ Open 7(9):e015830. https://doi.org/10.1136/bmjopen-2017-015830
Adams J, Steel A, Moore C et al (2016) Establishing the ACORN national practitioner database: strategies to recruit practitioners to a national practice-based research network. J Manipulative Physiol Ther 39(8):594–602. https://doi.org/10.1016/j.jmpt.2016.08.006
Australian Chiropractors Association. Australian Chiropractic Research Network (ACORN). ACORN project. Accessed May 9, 2023. https://www.chiropractors.org.au/resources/research/acorn-project
Steel A, Peng W, Sibbritt D et al (2020) Introducing national osteopathy practice-based research networks in Australia and New Zealand: an overview to inform future osteopathic research. Sci Rep 10(1):846. https://doi.org/10.1038/s41598-020-57918-7
Steel A, Sibbritt D, Schloss J et al (2017) An overview of the Practitioner Research and Collaboration Initiative (PRACI): a practice-based research network for complementary medicine. BMC Complement Altern Med 17(1):87. https://doi.org/10.1186/s12906-017-1609-3
Lalji R, Hofstetter L, Kongsted A et al (2022) Swiss chiropractic practice-based research network and musculoskeletal pain cohort pilot study: protocol of a nationwide resource to advance musculoskeletal health services research. BMJ Open 12(7):e059380. https://doi.org/10.1136/bmjopen-2021-059380
Lalji R, Hofstetter L, Kongsted A et al (2023) The Swiss chiropractic practice-based research network: a population-based cross-sectional study to inform future musculoskeletal research. Sci Rep 13(1):5655. https://doi.org/10.1038/s41598-023-32437-3
Thabane L, Ma J, Chu R et al (2010) A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol 10(1):1. https://doi.org/10.1186/1471-2288-10-1
von Elm E, Altman DG, Egger M et al (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335(7624):806–808. https://doi.org/10.1136/bmj.39335.541782.AD
Eldridge SM, Chan CL, Campbell MJ et al. (2016) CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. i5239. https://doi.org/10.1136/bmj.i5239
Lancaster GA, Thabane L (2019) Guidelines for reporting non-randomised pilot and feasibility studies. Pilot Feasibility Stud 5(1):114. https://doi.org/10.1186/s40814-019-0499-1
Humphreys BK, Peterson CK, Muehlemann D et al (2010) Are Swiss chiropractors different than other chiropractors? Results of the job analysis survey 2009. J Manip Physiol Ther 33(7):519–535. https://doi.org/10.1016/j.jmpt.2010.08.003
Kongsted A, Nielsen OL, Christensen HW et al (2020) The Danish chiropractic low back pain cohort (ChiCo): description and summary of an available data source for research collaborations. Clin Epidemiol 12:1015–1027. https://doi.org/10.2147/CLEP.S266220
Krebs EE, Lorenz KA, Bair MJ et al (2009) Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med 24(6):733–738. https://doi.org/10.1007/s11606-009-0981-1
Hill JC, Kang S, Benedetto E et al (2016) Development and initial cohort validation of the arthritis research UK musculoskeletal health questionnaire (MSK-HQ) for use across musculoskeletal care pathways. BMJ Open 6(8):e012331. https://doi.org/10.1136/bmjopen-2016-012331
Patridge EF, Bardyn TP (2018) Research electronic data capture (REDCap). J Med Libr Assoc 106(1):142–144. https://doi.org/10.5195/JMLA.2018.319
Federal Office of Public Health (FOPH), Bundesamt für Gesundheit. Register of medical professions. Accessed May 1, 2022. https://www.bag.admin.ch/bag/en/home/berufe-im-gesundheitswesen/medizinalberufe/medizinalberuferegister-medreg.html
Broadbent E, Petrie KJ, Main J et al (2006) The brief illness perception questionnaire. J Psychosom Res 60(6):631–637. https://doi.org/10.1016/j.jpsychores.2005.10.020
Linton SJ, Nicholas M, MacDonald S (2011) Development of a short form of the Örebro musculoskeletal pain screening questionnaire. Spine 36(22):1891–1895. https://doi.org/10.1097/BRS.0b013e3181f8f775
Kamper SJ, Maher CG, Mackay G (2009) Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther 17(3):163–170. https://doi.org/10.1179/jmt.2009.17.3.163
Walters SJ, dos BonachoAnjosHenriques-Cadby I, Bortolami O et al (2017) Recruitment and retention of participants in randomised controlled trials: a review of trials funded and published by the United Kingdom health technology assessment programme. BMJ Open 7(3):5276. https://doi.org/10.1136/bmjopen-2016-015276
Hestbaek L, Munck A, Hartvigsen L et al (2014) Low back pain in primary care: a description of 1250 patients with low back pain in danish general and chiropractic practice. Int J Family Med 2014:1–7. https://doi.org/10.1155/2014/106102
Wall TC, Mian MAH, Ray MN et al (2005) Improving physician performance through internet-based interventions: who will participate? J Med Internet Res 7(4):e48. https://doi.org/10.2196/jmir.7.4.e48
Fletcher B, Gheorghe A, Moore D et al (2012) Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open 2(1):e000496. https://doi.org/10.1136/bmjopen-2011-000496
Moffat KR, Shi W, Cannon P et al (2023) Factors associated with recruitment to randomised controlled trials in general practice: a systematic mixed studies review. Trials 24(1):90. https://doi.org/10.1186/s13063-022-06865-x
Fletcher K, Mant J, Roalfe A, Hobbs F (2010) Impact of study design on recruitment of patients to a primary care trial: an observational time series analysis of the Birmingham atrial fibrillation treatment of the aged (BAFTA) Study. Fam Pract 27(6):691–697. https://doi.org/10.1093/fampra/cmq050
Grimes DA, Schulz KF (2002) Cohort studies: marching towards outcomes. Lancet 359(9303):341–345. https://doi.org/10.1016/S0140-6736(02)07500-1
Gustavson K, von Soest T, Karevold E et al (2012) Attrition and generalizability in longitudinal studies: findings from a 15-year population-based study and a Monte Carlo simulation study. BMC Public Health 12(1):918. https://doi.org/10.1186/1471-2458-12-918
De Brouwer W, Patel CJ, Manrai AK et al (2021) Empowering clinical research in a decentralized world. NPJ Digit Med 4(1):102. https://doi.org/10.1038/s41746-021-00473-w
Goodson N, Wicks P, Morgan J et al (2022) Opportunities and counterintuitive challenges for decentralized clinical trials to broaden participant inclusion. NPJ Digit Med 5(1):58. https://doi.org/10.1038/s41746-022-00603-y
Teague S, Youssef GJ, Macdonald JA et al (2018) Retention strategies in longitudinal cohort studies: a systematic review and meta-analysis. BMC Med Res Methodol 18(1):151. https://doi.org/10.1186/s12874-018-0586-7
Acknowledgements
The authors would like to acknowledge the Swiss Chiropractic Association (ChiroSuisse), Pro Chiropractic Switzerland, and the Swiss chiropractic clinicians involved in this project for their participatory engagement and support. Group Authorship Members (Swiss ChiCo Clinicians Group): Ascona Chiropratica, Ascona, Switzerland: William Jardine (Clinician advisor and recruitment); Balgrist University Hospital, Department of Chiropractic Medicine, Zurich, Switzerland: Astrid Kurmann (Recruitment), Cesar A. Hincapié (Recruitment), Léonie Hofstetter (Recruitment), Lorene Rabold (Recruitment), Luana Nyirö (Recruitment), Malin Mühlemann (Recruitment), and Melanie Häusler (Recruitment); Cabinet aux 4 mains, Murten, Switzerland: Martine Randoll Schmutz (Recruitment), Nina Yerly (Recruitment), and Thierry Schmutz (Recruitment); Cabinet chiropratique Carole Beetschen, Geneva, Switzerland: Carole Beetschen (Recruitment); Cabinet chiropratique Marie-Pierre Roy, Fribourg, Switzerland: Marie-Pierre Roy (Recruitment); Cabinet chiropratique Parc. 137, La Chaux-de-Fonds, Switzerland: Nicole Schläppi (Recruitment), Rebecca Duvanel Austinat (Recruitment), and Seraina Francey (Recruitment); Cabinet Dr. Jérémie Baret, Lausanne, Switzerland: Jérémie Baret (Recruitment); Cabinet Houweling, Neuchâtel, Switzerland: Kirsten Olesen (Recruitment); Centre chiropratique Caves du Palais, Neuchâtel, Switzerland: Christian Chervet (Recruitment), Nils Osseiran (Recruitment), Patrick Ryser (Recruitment), Rebecca Duvanel Austinat (Recruitment), Romain Clerc (Recruitment), and Seraina Francey (Recruitment); Centre Médical de Vidy, consultation chiropratique, médecine du sport, Lausanne, Switzerland: Emilie Léonard (Clinician advisor and recruitment), Laure Béranger (Recruitment), and Vincent Billa (Recruitment); Chiro-Aarau, Aarau, Switzerland: Corinne R. Minder (Recruitment), Nicole Aeschlimann Kibler (Recruitment), and Peter Keller (Recruitment); Chiropractic Medicine Orthopaedic Sonnenhof, Bern, Switzerland: Jean-Pierre Cordey (Recruitment); ChirOlten, Olten, Switzerland: Dominic Strauss (Recruitment); ChiroMed am Stauffacher, Zurich, Switzerland: Christina Padua (Recruitment); ChiroNOIRAT, Lausanne, Switzerland: Aline Bidlingmeyer (Recruitment), Clarisse Noirat-Berdat (Recruitment), Marielle Hoarau (Recruitment), Roland Noirat (Recruitment), and Vincent Billa (Recruitment); Chiropraktik am Schaffhauserplatz, Zurich, Switzerland: Christof Schmid (Recruitment) and Serafin Leemann (Clinician advisor and recruitment); Chiropraktik am Stadelhofen, Zurich, Switzerland: Bernhard Pulver (Recruitment), Marcel Arioli (Recruitment), Simone Müller (Recruitment), Stephanie Zimmermann (Recruitment), and Thomas Lüthy (Recruitment); Chiropraktik Bad Ragaz, Bad Ragaz, Switzerland: Roy Bösiger (Recruitment) and Samuel Kosewähr (Recruitment); Chiropraktik Fribourg, Fribourg, Switzerland: Michel Aymon (Recruitment) and Peter Bon (Recruitment); Chiropraktik Gossau, Gossau, Switzerland: Lea Rohner (Recruitment), Martina Uffer (Recruitment); Chiropraktik Grenchen, Grenchen, Switzerland: Sonja Nardini (Recruitment); Chiropraktik Langenthal, Langenthal, Switzerland: Anja Maire (Recruitment), Mireille Schläppi (Recruitment), Sibylle Nebiker (Recruitment); Chiropraktik Schaffhausen, Schaffhausen, Switzerland: Urs Zahner (Recruitment), Astrid Kurmann (Recruitment); Chiropraktik Seeland, Biel/Bienne, Switzerland: Kirsten Olesen (Recruitment); Chiropraktik St. Moritz, St. Moritz, Switzerland: Sara Meier (Recruitment); Chiropraktik Wallisellen, Wallisellen, Switzerland: Stefan Rauber (Recruitment); Chiropraktik Zentrum Merz, St. Gallen, Switzerland: Antonia Gassner (Recruitment), Martin Merz (Recruitment), Noemi Amrhein (Recruitment); Chiropraktik Zimmerwald, Zimmerwald, Switzerland: Nadia Faigaux (Recruitment); Chiropraxis Knonaueramt, Affoltern am Albis, Switzerland: Corinne R. Minder (Recruitment), Patric Beereuter (Recruitment); Dr. Colette Faas Chiropraktik-Praxis, Schaffhausen, Switzerland: Colette Faas (Recruitment); Chiropraktik Willisau, Willisau, Switzerland: Fabienne Fehr Leu (Clinician Advisor and recruitment); Holbeinpraxis - Center for Chiropractic Medicine Basel, Basel, Switzerland: Damien Mauron (Clinician advisor); Institut Chiropratique Genéve, Geneva, Switzerland: Claude Illi (Recruitment), Tom Leleu (Recruitment); Praxis INTEGRI Bern, Bern, Switzerland: Andreas Fingal (Recruitment), Elisabeth Fingal (Recruitment), Ilona Salzmann (Recruitment), Jeanne Waldner (Recruitment), Malin Bengtsdotter Thurnherr (Recruitment), Nadia Graf (Recruitment), Sarah Filliez (Recruitment), Thomas Thurnherr (Recruitment); Praxis INTEGRI Thun, Thun, Switzerland: Federica Gianola (Recruitment), Nicholas Schenk (Recruitment), Michael Renfer (Recruitment); Studio Chiropratico Bianchi, Mendriso, Switzerland: Matilde A. Bianchi (Clinician advisor and recruitment).
Funding
Open access funding provided by University of Zurich. This work was internally supported with a grant to the University of Zurich from the Foundation for the Education of Chiropractors in Switzerland. This project was also supported by a grant from the Swiss chiropractic patient association (Pro Chiropractic Switzerland). The funders had no role in study conceptualization and design, or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
CAH, RL, LH, MAP, VvW, and AK conceived and participated in the design of the study. CAH obtained funding and was the principal investigator. CAH and MAP provided study resources and supervision. RL, LH, and CAH developed the electronic data collection forms. LH, RL, and CAH developed and implemented the clinician and patient report forms. RL and CAH led the execution of the study. RL, JB, and CAH participated in the statistical analysis for this manuscript. JB was the consulting biostatistician for this project. RL produced the first draft of this manuscript. All authors contributed to the writing and approval of the final manuscript. CAH had final responsibility for the decision to submit for publication. All authors had full access to all the data in the study and approved the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval
The Swiss ChiCo pilot study was approved by the independent research ethics committee of Canton Zurich (BASEC-Nr: 2021–01479) and complies with international ethical standards as outlined by the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lalji, R., Hofstetter, L., Kongsted, A. et al. Swiss chiropractic cohort (Swiss ChiCo) pilot study: feasibility for a musculoskeletal cohort study conducted within a nationwide practice-based research network. Eur Spine J 33, 2068–2078 (2024). https://doi.org/10.1007/s00586-024-08175-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-024-08175-z