Abstract
Purpose
While the etiopathogenesis of adolescent idiopathic scoliosis (AIS) remains unclear, it is assumed that muscular asymmetries contribute to curve progression. As previous studies have found asymmetries of the thoracic paraspinal muscles in AIS patients, our study’s aim was to analyze differences in the erector spinae, multifidus, quadratus lumborum, and psoas muscles of the lumbar spine depending on the curve’s radiographic characteristics.
Methods
We retrospectively included all patients who received posterior reposition spondylodesis for AIS treatment at our institution. Patients were classified according to the Lenke classification. Muscle cross-sectional areas were obtained from magnetic resonance imaging of the lumbar spine. Data were analyzed with the Wilcoxon rank sum test, the Kruskal–Wallis test with post hoc testing, or the Spearman’s correlation coefficient.
Results
Seventy-four (14 males and 60 females) AIS patients with a median age of 16 (IQR ± 4) years and a mean Cobb angle of 56.0° (± 18.0°) were included. In curve types Lenke 1 and 2 (n = 45), the erector spinae (p < 0.001) and multifidus (p < 0.001) muscles had a significantly larger cross-sectional area on the convex side, whereas the quadratus lumborum (p = 0.034) and psoas (p < 0.001) muscles each had a significantly larger cross-sectional area on the lumbar contralateral side.
Conclusion
Our results show an asymmetry of the lumbar spine’s muscles which depends on both the convexity and the extent of the scoliotic curve. While our results cannot prove whether these differences are the deformity’s cause or effect, they may contribute to a better understanding of AIS pathogenesis and may allow for more specific preoperative physiotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is defined as a three-dimensional structural deformity of the spine with a lateral curvature of at least 10° which occurs in apparently healthy children around puberty and makes up about 80% of scoliosis cases. Females are more frequently affected than males [1, 2].
To date, there is no consensus on AIS treatment, which is long-lasting and mostly starts as conservative treatment to correct the curve and prevent its progression during growth. Conservative treatment options include physiotherapy, physiotherapeutic scoliosis-specific exercises (PSSEs), and other types of physical therapy as well as bracing [3]. If the curve is more severe, surgical correction in terms of spinal stabilization and fusion may be necessary.
While the etiopathogenesis remains unclear, a multifactorial origin is assumed. Asymmetries and imbalance of the paraspinal and trunk muscles have been suggested to be a contributing factor [4, 5]. Most studies in this regard have been performed using surface electromyography (EMG) and/or histological differences. Several studies have reported a higher EMG activity on the convex curve side [6,7,8,9,10], while there are also contradictory results as reported by de Oliveira et al. [11].
As a muscle’s force production in terms of stabilization or generation of movement is proportional to its cross-sectional area, measuring the cross-sectional area of trunk muscles allows an analysis of their force-generating capacity. In doing so, Watanabe et al. found that in major AIS curves over 30° at skeletal maturity, a lower trunk muscle volume correlates with a greater progression of thoraco-lumbar or lumbar major curves during adulthood. They hypothesize that the decrease in muscle strength decreases spinal stability, which in turn results in curve progression [12].
However, little is known about differences in trunk and paraspinal muscles’ cross-sectional area associated with curve characteristics in adolescent patients with idiopathic scoliosis. Jiang et al. found muscular asymmetries of the paraspinal muscles in all levels of the thoracic spine, thus concluding that the muscular asymmetry is not restricted to the curve’s apex [13]. Our study’s aim therefore was to analyze whether in addition to the thoracic differences reported in the literature, there are differences in the erector spinae, multifidus, quadratus lumborum, and psoas muscles of the lumbar spine depending on the curve’s radiographic characteristics.
Materials and methods
Patient inclusion
This study was performed as a retrospective cross-sectional study and was approved by the institutional ethics committee (EA2/049/22). Patient informed consent was waived due to the retrospective study design. The study was carried out according to the declaration of Helsinki. We included patients who underwent posterior reposition spondylodesis for the treatment of idiopathic scoliosis from January 2011 to December 2021. At our center, the indication for a posterior reposition spondylodesis is given when the curve’s Cobb angle exceeds 40° with ongoing curve progression and the patient has reached skeletal maturity. Exclusion criteria were prior spinal surgery and incomplete imaging (preoperative magnetic resonance (MR) imaging, full spinal radiographs, and bending radiographs). One-hundred patients met the inclusion criteria, and 24 were excluded due to missing imaging and two due to prior spinal surgery. An overview of patient selection is shown in Fig. 1.
All radiological measurements were taken by an orthopedic surgery resident specifically trained in the classification according to Lenke as well as MRI muscle measurements.
Classification
Patient data were collected from electronic medical reports. Patients were classified according to the Lenke classification [14]. Curves were categorized into structural and compensatory with structural curvatures defined as a persisting curvature over 25° Cobb angle in bending radiographs and compensatory curvatures as redressable curvatures of less than 25° Cobb angle. Classification criteria are given in Table 1. All measurements were performed using the Phönix-PACS software (Phönix-PACS GmbH, Freiburg im Breisgau, Germany).
Measurements
The maximal lumbar and thoracic Cobb angles were measured on anterior–posterior full spine radiographs at the upper and lower most tilted vertebrae of both the lumbar and thoracic curvature.
For muscle measurements, multiplanar reconstructions of the MR images were performed. For each lumbar vertebra, a slice parallel to the endplate, including the middle of both pedicles, was set (Fig. 2). The cross-sectional areas of the psoas, quadratus lumborum, multifidus, and erector spinae muscles were manually measured on both the right and left sides (Fig. 2).
Statistical analysis
Statistical analyses were performed using SPSS version 27 (IBM Corporation, New York, USA). For paired data with pairwise samples, the Wilcoxon rank sum test was used. The Kruskal–Wallis test with Bonferroni correction for post hoc testing was used for data with more than two locations. Correlations were examined using Spearman’s correlation coefficient. The significance level was set at p < 0.05 for all tests.
Results
Patient characteristics
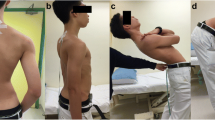
We included a total of 74 patients with idiopathic scoliosis. They had a median age of 16.0 years (IQR ± 4), height of 163.0 cm (± 11.0 cm), weight of 54.0 kg (± 18.0 kg), body mass index (BMI) of 19.2 kg/m2 (± 4.7 kg/m2), a thoracic Cobb angle of 59.1° (± 19.7°), and a lumbar curvature with a Cobb angle of 37.9° (± 14.1°). Fourteen males and 60 females were included. The distribution of idiopathic scolioses according to the Lenke classification is shown in Table 2. In all patients, the principal thoracic curve’s apex was located on the right side.
Effect of idiopathic scoliosis with functional lumbar scoliosis on lumbar muscle symmetry
The structural single or double thoracic curve in Lenke 1 and Lenke 2 scolioses had a significant effect on the symmetry of the lumbar musculature. While the autochthonous lumbar back muscles including the erector spinae and the multifidus muscles had a significantly larger cross-sectional area on the convex right side of the thoracic curvature, the quadratus lumborum and psoas muscles each had a significantly larger cross-sectional area on the lumbar contralateral side (Table 3; Fig. 3).
Segmental and overall lumbar muscle asymmetries. The graphs show the median with interquartile range based on each lumbar segment between the left and the right sides as well as L1–L5 of the psoas, quadratus lumborum, erector spinae, and L1–L4 for multifidus muscles. Significant differences were evaluated by Wilcoxon rank sum test and are marked with a *
The thoracic curve’s magnitude correlated negatively with the cross-sectional area of the erector spinae muscle on both sides (convex p = 0.007, r = − 0.265; concave p = 0.031, r = -0.213) and the left quadratus lumborum muscle (p = 0.013, r = − 0.265). No correlation with the cross-sectional area of the psoas, right quadratus lumborum, or multifidus muscles was detected. The functional lumbar curve’s magnitude in upright standing showed a significant correlation with the cross-sectional area of the right quadratus lumborum (p = 0.009, r = 0.204) and the erector spinae muscles (right p = 0.007, r = − 0.266; left p = 0.021, r = − 0.227), while no correlation was observed with the psoas, left quadratus lumborum, or multifidus muscles.
Relationship of the lumbar modifier with the muscular cross-sectional area in functional lumbar curvatures
Regarding the lumbar modifier in Lenke types 1 and 2, the cross-sectional areas of the psoas (right p = 0.336, left p = 0.397), quadratus lumborum (right p = 0.331, left p = 0.536), multifidus (right p = 0.607, left p = 0.541), and left erector spinae (p = 0.541) muscles did not differ significantly. For the right erector spinae muscle, a significant influence of the lumbar modifier was detected (p = 0.033) and a difference without post hoc testing between patients with lumbar modifier A and C was seen (p = 0.024); however, after Bonferroni correction no differences were detected (p = 0.074).
Differences between structural and functional lumbar curvature on the lumbar musculature
Comparing patients with structural (Lenke types 3–6) to patients with functional lumbar curvature (Lenke types 1 and 2), the right quadratus lumborum muscle was significantly larger in patients with Lenke types 3–6 (p = 0.007). For the left quadratus lumborum (p = 0.242) and the psoas (right p = 0.803, left p = 0.717), erector spinae (right p = 0.095, left p = 0.157), and multifidus (right p = 0.918, left p = 0.867) muscles, no significant differences were found.
Discussion
We found a larger cross-sectional area of the lumbar erector spinae and multifidus muscles on the convex side of the thoracic curvature of idiopathic scolioses types Lenke 1 and 2. In these types, a larger thoracic curve was associated with larger cross-sectional areas of the lumbar erector spinae and left quadratus lumborum muscles, while a larger lumbar curve was associated with larger cross-sectional areas of the lumbar erector spinae and right quadratus lumborum muscles.
The paraspinal muscles play a crucial role in maintaining spinal stability and postural control, which is why there is the hypothesis that they are significant in the development and progression of AIS [5, 15]. While several previous studies have already shown asymmetrical muscle behavior in AIS, in most of them EMG and histological analyses were used. These studies found increased EMG activity on the convex side of the scoliotic curve [6,7,8,9,10]. In addition to this increased EMG activity, both Stetkarova et al. and Shao et al. showed a predominance of type I muscle fibers in the paraspinal muscles of the scoliotic curve’s convexity [8, 16]. Furthermore, in their study a higher progression of AIS curve correlated significantly with an increase in type I fibers on the curve’s convexity. They concluded that these differences were most likely a sign of secondary adaptation to the higher load demand on the convex curve side [8]. Similarly, Shahidi et al. found muscle fibers or paraspinal muscles to be significantly larger on the curve’s convex side [17]. These asymmetries have been thought to be a sign of muscular weakness or of stretching of the erector spinae muscles on the convex side of the curve or may even be biomechanically necessary to balance the spine [6, 18, 19]. Lu et al. also found an imbalanced EMG activity of paraspinal muscles in patients with AIS, which was diminished by spine fusion [20]. While other studies have found conflicting results with no asymmetrical EMG behavior of the paraspinal muscles, this may be due to methodological differences in study design [11]. However, it is important to note that a muscle’s functionality may not be represented by its activation in terms of EMG behavior, position relative to the spine, or cross-sectional area in isolation but is a result of all three factors.
In contrast to EMG studies, there are only few studies investigating MRI-based muscle measurements and their relationship with radiographic scoliosis parameters. Jiang et al. found an increased volume of the thoracic erector spinae muscle on the convex side of the curve [13]. In accordance with those findings, Yeung et al. showed a significantly higher fatty infiltration of the paraspinal muscles at the curve’s concavity compared with healthy controls [15]. However, studies investigating the association between asymmetries in trunk and paraspinal muscles of the lumbar spine with scoliotic curve characteristic in AIS patients are lacking. In accordance with the abovementioned studies showing an increase in muscle activity and volume of the thoracic spine, we found an increased cross-sectional area of both the lumbar erector spinae and the multifidus muscles on the convex side of the scoliotic thoracic curve which may be due to the increased stretching of these muscles caused by the convexity. This is also supported by the fact that a larger extent of both the structural thoracic and the flexible lumbar curves was associated with a larger cross-sectional area of the erector spinae muscles. In all muscle measurements, it is, however, important to note that MR images were acquired in the horizontal position and thus the muscle tonus’ influence on muscle cross-sectional areas was not assessed [21].
Interestingly, in our study the quadratus lumborum and psoas muscles showed opposite behavior as they had significantly larger cross-sectional areas on the left side. This may be explained by the lumbar counter-curve as both the quadratus lumborum and psoas muscles are restricted to the lumbar spine and therefore may be less affected by the thoracic curve in contrast to the paraspinal muscles.
While we did not include patients with curves not requiring surgical correction, we did find a negative correlation between a larger structural thoracic curve and the cross-sectional area of both the erector spinae and the left quadratus lumborum muscles. Furthermore, in Lenke 1 und 2 scolioses, a larger lumbar curve was not associated with a larger cross-sectional area of the erector spinae muscles but with a larger cross-sectional area of the right quadratus lumborum muscle. Thus, the deformity’s extent seems to influence paraspinal muscle growth. While our results do not allow for a conclusion regarding the influence of curve progression, they may support the theory that the paraspinal muscles attempt to compensate the thoracic curve and to stabilize the spinal column [5].
Furthermore, while in degenerative lumbar diseases multiple studies investigating the effect of so-called prehabilitative measures including physiotherapy have been published, the literature for AIS in this regard is lacking to date [22]. As it seems plausible that physical preparation of the functional curve may contribute to an improved postoperative outcome in the surgical treatment of AIS as well, preoperative conditioning of patients undergoing spinal fusion for AIS should be investigated in future studies. This may not only influence the patients’ outcome in terms of curve correction but also quality of life, which is especially important as to date there is no conclusive evidence showing that Cobb angle correction correlates with other long-term outcomes such as function or quality of life [23].
Some limitations need to be discussed. First, as this was a retrospective study, MRIs were not performed with a standardized protocol. Second, to ensure comparability, we performed analyses of similar Lenke types only, thus rendering smaller sample sizes. Third, we only included patients who were treated surgically, which is why our results cannot be applied to AIS patients with less severe curves. As only one preoperative MRI was available in each of the included patients, we cannot make any statements regarding the influence of muscle asymmetries on curve progression. Furthermore, the MRIs were acquired under horizontal conditions which is why we cannot provide any data on muscle tonus. Lastly, it remains unclear whether the differences in muscles are cause or effect of the deformity.
Our results show an asymmetry of the lumbar spine’s muscles which depends on both the convexity and the extent of the scoliotic curve. While the paraspinal muscles show higher cross-sectional areas on the convex side of the main curve, the quadratus lumborum and psoas muscles show higher cross-sectional areas on the contralateral side. As previous work has focused on differences in the thoracic spine’s paraspinal muscles, our study provides evidence that muscle asymmetries do not only occur in proximity to the curve’s apex but are also found in the lumbar spine. While our results do not allow for any conclusions whether these differences are cause or effect of the deformity, they may contribute to a better understanding of the pathogenesis and mechanisms of progression in AIS patients. Furthermore, our results may provide the basis for future studies analyzing specific preoperative physiotherapy as part of a prehabilitative concept as increasingly performed in other spinal disorders.
Availability of data and materials
All data generated or analyzed during this study may be obtained from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371:1527–1537. https://doi.org/10.1016/s0140-6736(08)60658-3
Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, Diers H, Grivas TB, Knott P, Kotwicki T, Lebel A, Marti C, Maruyama T, O’Brien J, Price N, Parent E, Rigo M, Romano M, Stikeleather L, Wynne J, Zaina F (2018) 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scol Spinal Disord 13:3. https://doi.org/10.1186/s13013-017-0145-8
Romano M, Minozzi S, Zaina F, Saltikov JB, Chockalingam N, Kotwicki T, Hennes AM, Negrini S (2013) Exercises for adolescent idiopathic scoliosis: a Cochrane systematic review. Spine (Phila Pa 1976) 38:E883–E893. https://doi.org/10.1097/BRS.0b013e31829459f8
Modi HN, Suh SW, Yang JH, Hong JY, Venkatesh K, Muzaffar N (2010) Spontaneous regression of curve in immature idiopathic scoliosis - does spinal column play a role to balance? An observation with literature review. J Orthop Surg Res 5:80. https://doi.org/10.1186/1749-799x-5-80
Wong C (2015) Mechanism of right thoracic adolescent idiopathic scoliosis at risk for progression; a unifying pathway of development by normal growth and imbalance. Scoliosis 10:2. https://doi.org/10.1186/s13013-015-0030-2
Cheung J, Halbertsma JPK, Veldhuizen AG, Sluiter WJ, Maurits NM, Cool JC, van Horn JR (2005) A preliminary study on electromyographic analysis of the paraspinal musculature in idiopathic scoliosis. Eur Spine J 14:130–137. https://doi.org/10.1007/s00586-004-0780-7
Farahpour N, Ghasemi S, Allard P, Saba MS (2014) Electromyographic responses of erector spinae and lower limb’s muscles to dynamic postural perturbations in patients with adolescent idiopathic scoliosis. J Electromyogr Kinesiol 24:645–651. https://doi.org/10.1016/j.jelekin.2014.05.014
Stetkarova I, Zamecnik J, Bocek V, Vasko P, Brabec K, Krbec M (2016) Electrophysiological and histological changes of paraspinal muscles in adolescent idiopathic scoliosis. Eur Spine J 25:3146–3153. https://doi.org/10.1007/s00586-016-4628-8
Park Y, Ko JY, Jang JY, Lee S, Beom J, Ryu JS (2021) Asymmetrical activation and asymmetrical weakness as two different mechanisms of adolescent idiopathic scoliosis. Sci Rep 11:17582. https://doi.org/10.1038/s41598-021-96882-8
Liang R, Yip J, Fan Y, Cheung JPY, To KM (2022) Electromyographic analysis of paraspinal muscles of scoliosis patients using machine learning approaches. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph19031177
de Oliveira AS, Gianini PE, Camarini PM, Bevilaqua-Grossi D (2011) Electromyographic analysis of paravertebral muscles in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 36:E334-339. https://doi.org/10.1097/BRS.0b013e3181f516cd
Watanabe K, Ohashi M, Hirano T, Katsumi K, Shoji H, Mizouchi T, Endo N, Hasegawa K (2018) The influence of lumbar muscle volume on curve progression after skeletal maturity in patients with adolescent idiopathic scoliosis: a long-term follow-up study. Spine Deform 6:691–698. https://doi.org/10.1016/j.jspd.2018.04.003
Jiang J, Meng Y, Jin X, Zhang C, Zhao J, Wang C, Gao R, Zhou X (2017) Volumetric and fatty infiltration imbalance of deep paravertebral muscles in adolescent idiopathic scoliosis. Med Sci Monit 23:2089–2095. https://doi.org/10.12659/msm.902455
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83:1169–1181
Yeung KH, Man GCW, Shi L, Hui SCN, Chiyanika C, Lam TP, Ng BKW, Cheng JCY, Chu WCW (2019) Magnetic resonance imaging-based morphological change of paraspinal muscles in girls with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 44:1356–1363. https://doi.org/10.1097/brs.0000000000003078
Shao X, Chen J, Yang J, Sui W, Deng Y, Huang Z, Hu P, Yang J (2020) Fiber type-specific morphological and cellular changes of paraspinal muscles in patients with severe adolescent idiopathic scoliosis. Med Sci Monit 26:924415. https://doi.org/10.12659/msm.924415
Shahidi B, Yoo A, Farnsworth C, Newton PO, Ward SR (2021) Paraspinal muscle morphology and composition in adolescent idiopathic scoliosis: a histological analysis. JOR Spine 4:e1169. https://doi.org/10.1002/jsp2.1169
Butterworth TR Jr, James C (1969) Electromyographic studies in idiopathic scoliosis. South Med J 62:1008–1010. https://doi.org/10.1097/00007611-196908000-00026
Reuber M, Schultz A, McNeill T, Spencer D (1983) Trunk muscle myoelectric activities in idiopathic scoliosis. Spine (Phila Pa 1976) 8:447–456. https://doi.org/10.1097/00007632-198307000-00002
Lu WW, Hu Y, Luk KD, Cheung KM, Leong JC (2002) Paraspinal muscle activities of patients with scoliosis after spine fusion: an electromyographic study. Spine (Phila Pa 1976) 27:1180–1185. https://doi.org/10.1097/00007632-200206010-00009
Shaikh N, Zhang H, Brown SHM, Shewchuk JR, Vawda Z, Zhou H, Street J, Wilson DR, Oxland TR (2020) The effect of posture on lumbar muscle morphometry from upright MRI. Eur Spine J 29:2306–2318. https://doi.org/10.1007/s00586-020-06409-4
Eubanks JE, Carlesso C, Sundaram M, Bejarano G, Smeets R, Skolasky R, Vanushkina M, Turner R, Schneider MJ (2023) Prehabilitation for spine surgery: a scoping review. Pm r. https://doi.org/10.1002/pmrj.12956
Joarder I, Taniguchi S, Mendoza A, Snow ME (2023) Defining “successful” treatment outcomes in adolescent idiopathic scoliosis: a scoping review. Eur Spine J. https://doi.org/10.1007/s00586-023-07592-w
Funding
Open Access funding enabled and organized by Projekt DEAL. Not applicable.
Author information
Authors and Affiliations
Contributions
MP, LB, and FS were involved in conceptualization and project administration. ZL, ZW, LB, FS, and MP were involved in data curation. LB and FS were involved in formal analysis, methodology, and writing—original draft. FS, LB, and MP were involved in investigation, validation, and supervision. MP was involved in resources. FS, LB, MP, ZL, and ZW were involved in writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
There are no relevant conflicts nor competing interests.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Charité—University Medicine Berlin approved this study.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Becker, L., Li, Z., Wang, Z. et al. Adolescent idiopathic scoliosis is associated with muscle area asymmetries in the lumbar spine. Eur Spine J 32, 3979–3986 (2023). https://doi.org/10.1007/s00586-023-07921-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07921-z