Abstract
Background
The goal of this study was to better understand the variation of femoral neck version according to spinopelvic and lower limb 3D alignment using biplanar X-rays in standing position.
Methods
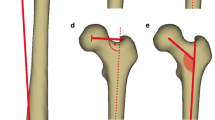
This multicentric study retrospectively included healthy subjects from previous studies who had free-standing position biplanar radiographs. Subjects were excluded if they presented spinal or any musculo-skeletal deformity, and reported pain in the spine, hip or knee. Age, sex, and the following 3D-reconstructed parameters were collected: spinal curvatures, pelvic parameters, sagittal vertical axis (SVA), T1 pelvic angle (TPA), spino-sacral angle (SSA), femoral torsion angle (FTA), sacro-femoral angle (SFA), knee flexion angle (KA), ankle angle (AA), pelvic shift (PS) and ankle distance. Femoral neck version angle (FVA) was calculated between horizontal plane projection of the bi-coxo-femoral axis and the line passing through the femoral neck barycenter and femoral head center. Analysis according to age subsets was performed.
Results
A total of 400 subjects were included (219 females); mean age was 29 ± 18 years (range: 4–83). Subjects with high pelvic tilt values presented significantly higher FVA than average and low-PT individuals, respectively, 7.8 ± 7.1°, 2 ± 9° and 2.1 ± 9.5° (p < 0.001). These subjects also presented lower lumbar lordosis values and higher acetabulum anteversion in the horizontal plane than the two other groups. SVA correlation with FVA was weaker (r = 0.1, p = 0.03) than SSA and TPA (r = − 0.3 and r = 0.3, respectively, p < 0.001). A strong correlation was found with femoral torsion (r = 0.5, p < 0.001). SFA (r = − 0.3, p < 0.001), pelvic shift (r = 0.2, p < 0.001) and ankle distance (r = 0.3, p < 0.001) were also significantly correlated. Multivariate analysis confirmed significant association of age, pelvic tilt, lumbar lordosis, pelvic shift, ankle distance and femoral torsion with FVA.
Conclusion
Patients with lower lumbar lordosis present pelvic retroversion which induces a higher femoral neck version. This finding may help positioning implants in total hip replacement procedures. Higher pelvic shift, age, male gender and increased femoral torsion were also correlated with higher FVA.
Level of evidence
II (Diagnostic: individual cross-sectional studies with consistently applied reference standard and blinding).





Similar content being viewed by others
References
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103. https://doi.org/10.1007/s005860050038
Laouissat F, Sebaaly A, Gehrchen M, Roussouly P (2018) Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J 27:2002–2011. https://doi.org/10.1007/s00586-017-5111-x
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30:346–353
Terran J, Schwab F, Shaffrey CI et al (2013) The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery 73:559–568. https://doi.org/10.1227/NEU.0000000000000012
Celestre PC, Dimar JR, Glassman SD (2018) Spinopelvic parameters: lumbar lordosis, pelvic incidence, pelvic tilt, and sacral slope: what does a spine surgeon need to know to plan a lumbar deformity correction? Neurosurg Clin N Am 29:323–329. https://doi.org/10.1016/j.nec.2018.03.003
Beyer G, Khalifé M, Lafage R et al (2020) Pelvic compensation in sagittal malalignment: how much retroversion can the pelvis accommodate? Spine (Phila Pa 1976) 45:E203–E209. https://doi.org/10.1097/BRS.0000000000003228
Barrey C, Roussouly P, Le Huec J-C et al (2013) Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 22(Suppl 6):S834–S841. https://doi.org/10.1007/s00586-013-3030-z
Zhu W, Kong C, Zhang S et al (2020) Different acute behaviors of pelvic incidence after long fusion to sacrum between elderly patients with severe and minor sagittal deformity: a retrospective radiographic study on 102 cases. Eur Spine J 29:1379–1387. https://doi.org/10.1007/s00586-020-06395-7
Lee BH, Moon SH, Lee HM et al (2012) Prevalence of hip pathology in patients over age 50 with spinal conditions requiring surgery. Indian J Orthop 46:291–296. https://doi.org/10.4103/0019-5413.96386
Offierski CM, MacNab I (1983) Hip-spine syndrome. Spine (Phila Pa 1976) 8:316–321. https://doi.org/10.1097/00007632-198304000-00014
Chavarria JC, Douleh DG, York PJ (2021) The hip-spine challenge. J Bone Jt Surg Am 103:1852–1860. https://doi.org/10.2106/JBJS.20.01728
Mekhael M, Kawkabani G, Saliby RM et al (2021) Toward understanding the underlying mechanisms of pelvic tilt reserve in adult spinal deformity: the role of the 3D hip orientation. Eur Spine J 30:2495–2503. https://doi.org/10.1007/s00586-021-06778-4
Morimoto T, Kitajima M, Tsukamoto M et al (2018) Sagittal spino-pelvic alignment in rapidly destructive coxarthrosis. Eur Spine J 27:475–481. https://doi.org/10.1007/s00586-017-5282-5
Ouchida J, Nakashima H, Kanemura T et al (2022) Impact of the hip joint mobility on whole-body sagittal alignment: prospective analysis in case with hip arthroplasty. Eur Spine J. https://doi.org/10.1007/s00586-022-07251-6
Kim Y, Pour AE, Lazennec JY (2020) How do global sagittal alignment and posture change after total hip arthroplasty? Int Orthop 44:267–273. https://doi.org/10.1007/s00264-019-04363-5
Gómez-Hoyos J, Schröder R, Reddy M et al (2016) Femoral neck anteversion and lesser trochanteric retroversion in patients with ischiofemoral impingement: a case-control magnetic resonance imaging study. Arthroscopy 32:13–18. https://doi.org/10.1016/j.arthro.2015.06.034
Tönnis D, Heinecke A (1999) Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Jt Surg Am 81:1747–1770. https://doi.org/10.2106/00004623-199912000-00014
Ferrero E, Lafage R, Challier V et al (2015) Clinical and stereoradiographic analysis of adult spinal deformity with and without rotatory subluxation. Orthop Traumatol Surg Res 101:613–618. https://doi.org/10.1016/j.otsr.2015.04.008
Newton PO, Fujimori T, Doan J et al (2015) Defining the “three-dimensional sagittal plane” in thoracic adolescent idiopathic scoliosis. J Bone Jt Surg Am 97:1694–1701. https://doi.org/10.2106/JBJS.O.00148
Courvoisier A, Vialle R, Skalli W (2014) EOS 3D imaging: assessing the impact of brace treatment in adolescent idiopathic scoliosis. Expert Rev Med Dev 11:1–3. https://doi.org/10.1586/17434440.2014.848166
Sandoz B, Laporte S, Skalli W, Mitton D (2010) Subject-specific body segment parameters’ estimation using biplanar X-rays: a feasibility study. Comput Methods Biomech Biomed Eng 13:649–654. https://doi.org/10.1080/10255841003717608
Chaibi Y, Cresson T, Aubert B et al (2012) Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput Methods Biomech Biomed Eng 15:457–466. https://doi.org/10.1080/10255842.2010.540758
Humbert L, De Guise JA, Aubert B et al (2009) 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 31:681–687. https://doi.org/10.1016/j.medengphy.2009.01.003
Amabile C, Pillet H, Lafage V et al (2016) A new quasi-invariant parameter characterizing the postural alignment of young asymptomatic adults. Eur Spine J 25:3666–3674. https://doi.org/10.1007/s00586-016-4552-y
Lewinnek GE, Lewis JL, Tarr R et al (1978) Dislocations after total hip-replacement arthroplasties. J Bone Jt Surg Am 60:217–220
Scorcelletti M, Reeves ND, Rittweger J, Ireland A (2020) Femoral anteversion: significance and measurement. J Anat 237:811–826. https://doi.org/10.1111/joa.13249
Passias PG, Jalai CM, Diebo BG et al (2019) Full-body radiographic analysis of postoperative deviations from age-adjusted alignment goals in adult spinal deformity correction and related compensatory recruitment. Int J Spine Surg 13:205–214. https://doi.org/10.14444/6028
Vialle R, Levassor N, Rillardon L et al (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Jt Surg Am 87:260–267. https://doi.org/10.2106/JBJS.D.02043
Perdriolle R (1979) La scoliose: son étude tridimensionnelle
Skalli W, Lavaste F, Descrimes JL (1995) Quantification of three-dimensional vertebral rotations in scoliosis: what are the true values? Spine (Phila Pa 1976) 20:546–553. https://doi.org/10.1097/00007632-199503010-00008
Fuller CB, Farnsworth CL, Bomar JD et al (2018) Femoral version: comparison among advanced imaging methods. J Orthop Res 36:1536–1542. https://doi.org/10.1002/jor.23785
Chen C, Min L, Sun M et al (2021) Abnormal femur rotation in patients with recurrent patellar dislocation: a study on upright standing three-dimensionally reconstructed EOS images. Knee 32:131–139. https://doi.org/10.1016/j.knee.2021.08.011
Westermann RW, Willey MC (2021) Femoral version in hip arthroscopy: does it matter? Sports Med Arthrosc 29:28–34. https://doi.org/10.1097/JSA.0000000000000299
Le Huec JC, Thompson W, Mohsinaly Y et al (2019) Sagittal balance of the spine. Eur Spine J 28:1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Funding
No funding was used for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Khalifé: Holds share of the NovaSpine company, which presents no competing interests with the present study. Skalli: Personal royalties from EOS imaging. No other conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalifé, M., Vergari, C., Rebeyrat, G. et al. Femoral neck version in the spinopelvic and lower limb 3D alignment: a full-body EOS® study in 400 healthy subjects. Eur Spine J (2023). https://doi.org/10.1007/s00586-023-07915-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-023-07915-x