Abstract
Objective
To evaluate the validity of intraoperative evoked potential (EP) including motor evoked potential (MEP) and somatosensory evoked potentials (SEP) as a biomarker for predicting neural function changes after thoracic spinal decompression (TSD) surgery.
Method
A consecutive series of 336 TSD surgeries were reviewed between 2010 and 2021 from four spine center. All patients with TSD were divided into 3 groups according to different intraoperative EP results: group 1, EP alerts; group 2, no obvious EP deterioration; group 3, EP improvement compared with baselines. The lower limb Japanese Orthopedic Association (JOA) scores (as well as early and long-term JOA recovery rate) were utilized to quantitatively assess pre- and postoperative neural function change.
Results
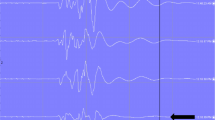
Among the 3 subgroups according to the different EP changes, the early JOA recovery rate (RR%) in the EP improvement group was significantly better than the other two groups (51.3 ± 58.6* vs. 27.5 ± 31.2 and 33.3 ± 43.1; p < 0.01) after 3-month follow-up. The mean MEP and SEP amplitude were from 116 ± 57 µV to 347 ± 71 µV (p < 0.01) and from 1.86 ± 0.24 µV to 2.65 ± 0.29 µV (p < 0.01) between spinal cord pre-decompression and post-decompression. Moreover, multivariate logistic regression analysis revealed that risk factors of EP improvement were duration of symptom (p < 0.001, OR 10.9) and Preop. neurologic deficit degree (p = 0.013, OR 7.46).
Conclusion
The intraoperative EP can predict postoperative neural function changes as a biomarker during TSD. Patient with EP improvement probably has better prognosis for early neural function recovery. The duration of symptom and preoperative neurologic deficit degree may be related to intraoperative EP improvement.


Similar content being viewed by others
References
Macdonald DB, Skinner S, Shils J, Yingling C, American Society of Neurophysiological M (2013) Intraoperative motor evoked potential monitoring—a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol 124:2291–2316. https://doi.org/10.1016/j.clinph.2013.07.025
Taher F, Lebl DR, Cammisa FP, Pinter DW, Sun DY, Girardi FP (2013) Transient neurological deficit following midthoracic decompression for severe stenosis: a series of three cases. Eur Spine J: Off Pub Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22:2057–2061. https://doi.org/10.1007/s00586-013-2829-y
Eggspuehler A, Sutter MA, Grob D, Porchet F, Jeszenszky D, Dvorak J (2007) Multimodal intraoperative monitoring (MIOM) during surgical decompression of thoracic spinal stenosis in 36 patients. Eur Spine J: Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 16(Suppl 2):S216-220. https://doi.org/10.1007/s00586-007-0425-8
Kaneko K, Sakamoto S, Toyoda K, Kato Y, Taguchi T (2006) False negative in spinal cord monitoring using spinal cord–evoked potentials following spinal cord stimulation during surgery for thoracic OPLL and OLF. J Spinal Disord Tech 19:142–144. https://doi.org/10.1097/01.bsd.0000171628.93245.13
Clark AJ, Ziewacz JE, Safaee M, Lau D, Lyon R, Chou D, Weinstein PR, Ames CP, Clark JP 3rd, Mummaneni PV (2013) Intraoperative neuromonitoring with MEPs and prediction of postoperative neurological deficits in patients undergoing surgery for cervical and cervicothoracic myelopathy. Neurosurg Focus 35:E7. https://doi.org/10.3171/2013.4.FOCUS13121
Wang S, Zhang J, Tian Y, Shen J, Zhao Y, Zhao H, Li S, Yu B, Weng X (2017) Intraoperative motor evoked potential monitoring to patients with preoperative spinal deficits: judging its feasibility and analyzing the significance of rapid signal loss. Spine J: Off J North Am Spine Soc 17:777–783. https://doi.org/10.1016/j.spinee.2015.09.028
Jarvis JG, Strantzas S, Lipkus M, Holmes LM, Dear T, Magana S, Lebel DE, Lewis SJ (2013) Responding to neuromonitoring changes in 3-column posterior spinal osteotomies for rigid pediatric spinal deformities. Spine 38:E493-503. https://doi.org/10.1097/BRS.0b013e3182880378
Hilibrand AS, Schwartz DM, Sethuraman V, Vaccaro AR, Albert TJ (2004) Comparison of transcranial electric motor and somatosensory evoked potential monitoring during cervical spine surgery. J Bone Jt Surg Am 86(6):1248–1253
Quraishi NA, Lewis SJ, Kelleher MO, Sarjeant R, Rampersaud YR, Fehlings MG (2009) Intraoperative multimodality monitoring in adult spinal deformity analysis of a prospective series of one hundred two cases with independent evaluation. Spine 34:1504–1512. https://doi.org/10.1097/Brs.0b013e3181a87b66
Lieberman JA, Lyon R, Feiner J, Hu SS, Berven SH (2008) The efficacy of motor evoked potentials in fixed sagittal imbalance deformity correction surgery. Spine 33:E414–E424. https://doi.org/10.1097/BRS.0b013e318175c292
Currier BL, Eismont FJ, Green BA (1994) Transthoracic disc excision and fusion for herniated thoracic disks. Spine 19:323–328. https://doi.org/10.1097/00007632-199402000-00012
Akhaddar A, Mansouri A, Zrara I, Gazzaz M, Maftah M, Mostarchid B, Benomar S, Boucetta M (2002) Thoracic spinal cord compression by ligamentum flavum ossifications. Jt Bone Spine 69:319–323. https://doi.org/10.1016/S1297-319x(02)00400-1
He BR, Yan L, Xu ZW, Guo H, Liu TJ, Hao DJ (2014) Treatment strategies for the surgical complications of thoracic spinal stenosis: a retrospective analysis of two hundred and eighty three cases. Int Orthop 38:117–122. https://doi.org/10.1007/s00264-013-2103-2
Chen ZY, Wong HK, Chan YH (2004) Variability of somatosensory evoked potential monitoring during scoliosis surgery. J Spinal Disord Tech 17:470–476. https://doi.org/10.1097/01.bsd.0000133465.89618.c8
Hong JY, Suh SW, Modi HN, Hur CY, Song HR, Park JH (2010) False negative and positive motor evoked potentials in one patient: is single motor evoked potential monitoring reliable method? A case report and literature review. Spine 35:E912–E916. https://doi.org/10.1097/BRS.0b013e3181d8fabb
Modi HN, Suh SW, Yang JH, Yoon JY (2009) False-negative transcranial motor-evoked potentials during scoliosis surgery causing paralysis: a case report with literature review. Spine 34:E896-900. https://doi.org/10.1097/BRS.0b013e3181b40d4f
Lee KS, Shim JJ, Doh JW, Yoon SM, Bae HG, Yun IG (2004) Transient paraparesis after laminectomy in a patient with multi-level ossification of the spinal ligament. J Korean Med Sci 19:624–626
Sugawara T, Chan PH (2003) Reactive oxygen radicals and pathogenesis of neuronal death after cerebral ischemia. Antioxid Redox Signal 5:597–607. https://doi.org/10.1089/152308603770310266
Hasegawa K, Homma T, Chiba Y (2007) Upper extremity palsy following cervical decompression surgery results from a transient spinal cord lesion. Spine 32:E197-202. https://doi.org/10.1097/01.brs.0000257576.84646.49
Park MK, Lee SJ, Kim SB, Lee KW, Lee HJ, Han EY, Kim BR (2018) The effect of positive changes during intraoperative monitoring of the functional improvement in patients with cervical compressive myelopathy. Clin Interv Aging 13:1211–1218. https://doi.org/10.2147/CIA.S163467
Bouchard JA, Bohlman HH, Biro C (1996) Intraoperative improvements of somatosensory evoked potentials: correlation to clinical outcome in surgery for cervical spondylitic myelopathy. Spine 21:589–594. https://doi.org/10.1097/00007632-199603010-00011
Bhattacharyya S (2018) Spinal cord disorders: myelopathy. Am J Med 131:1293–1297. https://doi.org/10.1016/j.amjmed.2018.03.009
Onishi E, Yasuda T, Yamamoto H, Iwaki K, Ota S (2016) Outcomes of surgical treatment for thoracic myelopathy: a single-institutional study of 73 patients. Spine 41:E1356–E1363. https://doi.org/10.1097/BRS.0000000000001622
Visser J, Verra WC, Kuijlen JM, Horsting PP, Journee HL (2014) Recovery of TES-MEPs during surgical decompression of the spine: a case series of eight patients. J Clin Neurophysiol 31:568–574. https://doi.org/10.1097/WNP.0000000000000099
Zhao M, Zhang Y, Liu L, Liu Y, Liao W (1997) Somatosensory- and motor-evoked potentials in a rabbit model of spinal cord ischemia and reperfusion injury. Spine 22:1013–1017
Chen Q, Li F, Wu W (2012) Risk factors of iatrogenic spinal cord injury in spinal surgery: a multicenter retrospective study. Int J Neurosci 122:606–610. https://doi.org/10.3109/00207454.2012.700660
Aoyama T, Hida K, Akino M, Yano S, Iwasaki Y, Saito H (2007) Ultra-early MRI showing no abnormality in a fall victim presenting with tetraparesis. Spinal Cord 45:695–699. https://doi.org/10.1038/sj.sc.3102014
Olmsted ZT, Ryu B, Phayal G, Green R, Lo SL, Sciubba DM, Silverstein JW, D’Amico RS (2023) Direct wave intraoperative neuromonitoring for spinal tumor resection: a focused review. World Neurosurg X 17:100139. https://doi.org/10.1016/j.wnsx.2022.100139
Costa P, Peretta P, Faccani G (2013) Relevance of intraoperative D wave in spine and spinal cord surgeries. Eur Spine J: Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22:840–848. https://doi.org/10.1007/s00586-012-2576-5
Ghadirpour R, Nasi D, Iaccarino C, Romano A, Motti L, Sabadini R, Valzania F, Servadei F (2018) Intraoperative neurophysiological monitoring for intradural extramedullary spinal tumors: predictive value and relevance of D-wave amplitude on surgical outcome during a 10-year experience. J Neurosurg Spine 30:259–267. https://doi.org/10.3171/2018.7.SPINE18278
Shigematsu H, Ando M, Kobayashi K, Yoshida G, Funaba M, Morito S, Takahashi M, Ushirozako H, Kawabata S, Yamada K, Kanchiku T, Fujiwara Y, Taniguchi S, Iwasaki H, Tadokoro N, Wada K, Yamamoto N, Yasuda A, Hashimoto J, Tani T, Ando K, Machino M, Takatani T, Matsuyama Y, Imagama S (2022) Efficacy of D-Wave monitoring combined with the transcranial motor-evoked potentials in high-risk spinal surgery: a retrospective multicenter study of the monitoring committee of the japanese society for spine surgery and related research. Glob Spine J. https://doi.org/10.1177/21925682221084649
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, S., Lin, X., Guo, L. et al. Validity of evoked potential as biomarker for predicting early neural function changes after thoracic spinal decompression surgery in patients with neurological deficits. Eur Spine J 33, 924–931 (2024). https://doi.org/10.1007/s00586-023-07893-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07893-0