Abstract
Purpose
Adjacent segment disease (ASD) is a common complication in fusion surgery. In the event of solid segmental fusion, previous implants can be removed or preserved during fusion extension for ASD. To compare the surgical outcomes of patients with and without implants and analyzes the risk factors for postoperative mechanical complications.
Methods
Patients who underwent fusion extension for lumbar ASD from 2011 to 2019 with a minimum 2 year follow-up were retrospectively reviewed. Spinopelvic parameters were measured preoperatively and postoperatively. Clinical outcomes and surgical complications were compared between groups with implants preserved and removed. Risk factors for mechanical complications, including clinical, surgical, and radiographic factors were analyzed.
Results
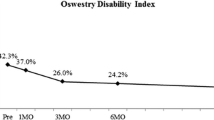
Sixty-nine patients (mean age, 69.9 ± 6.9 years) were included. The mean numbers of initial and extended fused segments were 2.8 ± 0.7 and 2.7 ± 0.7, respectively. Previous implants were removed in 43 patients (R group) and preserved in 26 patients (P group). Both groups showed an improvement in clinical outcomes without between-group differences. The operation time was significantly longer in R group (260 vs 207 min, p < 0.001). Mechanical complications occurred in 13 patients (12 in R group and 1 in P group) and reoperation was needed in 3 patients (R group). Implant removal, index fusion surgery including L5-S1, and postoperative sagittal malalignment were risk factors for mechanical complications.
Conclusion
Implant removal was a risk factor for mechanical complications. Index fusion surgery including L5-S1 and postoperative sagittal malalignment were also risk factors for mechanical complications.




Similar content being viewed by others
References
Okuda S, Nagamoto Y, Matsumoto T, Sugiura T, Takahashi Y, Iwasaki M (2018) Adjacent segment disease after single segment posterior lumbar interbody fusion for degenerative spondylolisthesis: minimum 10 years follow-up. Spine 43:E1384-e1388. https://doi.org/10.1097/brs.0000000000002710
Lang Z, Li JS, Yang F, Yu Y, Khan K, Jenis LG, Cha TD, Kang JD, Li G (2019) Reoperation of decompression alone or decompression plus fusion surgeries for degenerative lumbar diseases: a systematic review. Eur Spine J 28:1371–1385. https://doi.org/10.1007/s00586-018-5681-2
Ryu DS, Park JY, Kuh SU, Chin DK, Kim KS, Cho YE, Kim KH (2018) Surgical outcomes after segmental limited surgery for adjacent segment disease: the consequences of makeshift surgery. World Neurosurg 110:e258–e265. https://doi.org/10.1016/j.wneu.2017.10.150
Teles AR, Yavin D, Zafeiris CP, Thomas KC, Lewkonia P, Nicholls FH, Swamy G, Jacobs WB (2018) Fractures after removal of spinal instrumentation: revisiting the stress-shielding effect of instrumentation in spine fusion. World Neurosurg 116:e1137–e1143. https://doi.org/10.1016/j.wneu.2018.05.187
Ha KY, Kim YH, Park HY, Min HK, Kim SI (2019) Lumbar disc herniation within solid fused segments after removal of pedicle screws: a case report. JBJS Case Connect 9:e0071. https://doi.org/10.2106/jbjs.Cc.19.00071
Kwon JW, Moon SH, Park SY, Park SJ, Park SR, Suk KS, Kim HS, Lee BH (2022) Lumbar spinal stenosis: review update 2022. Asian Spine J. https://doi.org/10.31616/asj.2022.0366
Kim GU, Park WT, Chang MC, Lee GW (2022) Diagnostic technology for spine pathology. Asian Spine J. https://doi.org/10.31616/asj.2022.0374
Lee GW, Shin JH (2018) Comparative study of two surgical techniques for proximal adjacent segment pathology after posterior lumbar interbody fusion with pedicle screws: fusion extension using conventional pedicle screw vs cortical bone trajectory-pedicle screw (cortical screw). World Neurosurg 117:e154–e161. https://doi.org/10.1016/j.wneu.2018.05.218
Tan QC, Wang D, Yang Z, Zhao XL, Zhang Y, Yan YB, Feng YF, Lei W, Zhao X, Wu ZX (2021) Implant preservation versus implant replacement in revision surgery for adjacent segment disease after thoracolumbar instrumentation: a retrospective study of 43 patients. World Neurosurg 150:e511–e519. https://doi.org/10.1016/j.wneu.2021.03.046
Ha KY, Schendel MJ, Lewis JL, Ogilvie JW (1993) Effect of immobilization and configuration on lumbar adjacent-segment biomechanics. J Spinal Disord 6:99–105
Kim HJ, Chun HJ, Moon SH, Kang KT, Kim HS, Park JO, Moon ES, Sohn JS, Lee HM (2010) Analysis of biomechanical changes after removal of instrumentation in lumbar arthrodesis by finite element analysis. Med Biol Eng Comput 48:703–709. https://doi.org/10.1007/s11517-010-0621-2
Totoribe K, Chosa E, Tajima N (2004) A biomechanical study of lumbar fusion based on a three-dimensional nonlinear finite element method. J Spinal Disord Tech 17:147–153. https://doi.org/10.1097/00024720-200404000-00012
Hsieh YY, Chen CH, Tsuang FY, Wu LC, Lin SC, Chiang CJ (2017) Removal of fixation construct could mitigate adjacent segment stress after lumbosacral fusion: a finite element analysis. Clin Biomech (Bristol, Avon) 43:115–120. https://doi.org/10.1016/j.clinbiomech.2017.02.011
Sedney CL, Daffner SD, Stefanko JJ, Abdelfattah H, Emery SE, France JC (2016) Fracture of fusion mass after hardware removal in patients with high sagittal imbalance. J Neurosurg Spine 24:639–643. https://doi.org/10.3171/2015.7.Spine15153
McAfee PC, Farey ID, Sutterlin CE, Gurr KR, Warden KE, Cunningham BW (1991) The effect of spinal implant rigidity on vertebral bone density a canine model. Spine 16:S190–S1197. https://doi.org/10.1097/00007632-199106001-00003
Benditz A, Auer S, Spörrer JF, Wolkerstorfer S, Grifka J, Suess F, Dendorfer S (2018) Regarding loads after spinal fusion, every level should be seen separately: a musculoskeletal analysis. Eur Spine J 27:1905–1910. https://doi.org/10.1007/s00586-018-5476-5
Galbusera F, Wilke HJ, Brayda-Bruno M, Costa F, Fornari M (2013) Influence of sagittal balance on spinal lumbar loads: a numerical approach. Clin Biomech (Bristol, Avon) 28:370–377. https://doi.org/10.1016/j.clinbiomech.2013.02.006
Hashimoto K, Aizawa T, Kanno H, Itoi E (2019) Adjacent segment degeneration after fusion spinal surgery-a systematic review. Int Orthop 43:987–993. https://doi.org/10.1007/s00264-018-4241-z
Park WM, Choi DK, Kim K, Kim YJ, Kim YH (2015) Biomechanical effects of fusion levels on the risk of proximal junctional failure and kyphosis in lumbar spinal fusion surgery. Clin Biomech (Bristol, Avon) 30:1162–1169. https://doi.org/10.1016/j.clinbiomech.2015.08.009
Patwardhan AG, Sielatycki JA, Havey RM, Humphreys SC, Hodges SD, Blank KR, Muriuki MG (2021) Loading of the lumbar spine during transition from standing to sitting: effect of fusion versus motion preservation at L4–L5 and L5–S1. Spine J 21:708–719. https://doi.org/10.1016/j.spinee.2020.10.032
Acknowledgements
The author wishes to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2022.
Funding
The author wishes to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2022.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, YH., Ha, KY., Ahn, J. et al. Risk factors for mechanical complications after fusion extension surgery for lumbar adjacent segment disease. Eur Spine J 33, 324–331 (2024). https://doi.org/10.1007/s00586-023-07880-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07880-5