Abstract
Purpose
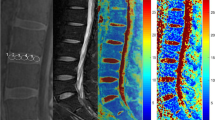
Using ultrashort echo time (UTE) MRI, we determined prevalence of abnormal cartilaginous endplate (CEP), and the relationship between CEP and disc degeneration in human lumbar spines.
Materials and methods
Lumbar spines from 71 cadavers (age 14–74 years) were imaged at 3 T using sagittal UTE and spin echo T2 map sequences. On UTE images, CEP morphology was defined as “normal” with linear high signal intensity or “abnormal” with focal signal loss and/or irregularity. On spin echo images, disc grade and T2 values of the nucleus pulposus (NP) and annulus fibrosus (AF) were determined. 547 CEPs and 284 discs were analysed. Effects of age, sex, and level on CEP morphology, disc grade, and T2 values were determined. Effects of CEP abnormality on disc grade, T2 of NP, and T2 of AF were also determined.
Results
Overall prevalence of CEP abnormality was 33% and it tended to increase with older ages (p = 0.08) and at lower spinal levels of L5 than L2 or L3 (p = 0.001). Disc grades were higher and T2 values of the NP were lower in older spines (p < 0.001) and at lower disc level of L4-5 (p < 0.05). We found significant association between CEP and disc degeneration; discs adjacent to abnormal CEPs had high grades (p < 0.01) and lower T2 values of the NP (p < 0.05).
Conclusion
These results suggest that abnormal CEPs are frequently found, and it associates significantly with disc degeneration, suggesting an insight into pathoetiology of disc degeneration.





Similar content being viewed by others
References
Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS (2009) The rising prevalence of chronic low back pain. Arch Intern Med 169:251–258. https://doi.org/10.1001/archinternmed.2008.543
An HS, Anderson PA, Haughton VM, Iatridis JC, Kang JD, Lotz JC, Natarajan RN, Oegema TR Jr, Roughley P, Setton LA, Urban JP, Videman T, Andersson GB, Weinstein JN (2004) Introduction: disc degeneration: summary. Spine 29:2677–2678
Moneta GB, Videman T, Kaivanto K, Aprill C, Spivey M, Vanharanta H, Sachs BL, Guyer RD, Hochschuler SH, Raschbaum RF et al (1994) Reported pain during lumbar discography as a function of anular ruptures and disc degeneration. A re-analysis of 833 discograms. Spine (Phila Pa 1976) 19:1968–1974
Abu-Ghanem S, Ohana N, Abu-Ghanem Y, Kittani M, Shelef I (2013) Acute schmorl node in dorsal spine: an unusual cause of a sudden onset of severe back pain in a young female. Asian Spine J 7:131–135. https://doi.org/10.4184/asj.2013.7.2.131
Bogduk N, Endres SM (2005) Clinical anatomy of the lumbar spine and sacrum. Clinical anatomy of the lumbar spine and sacrum, 4th edn. Elsevier/Churchill Livingstone, New York
Crock HV, Goldwasser M (1984) Anatomic studies of the circulation in the region of the vertebral end-plate in adult Greyhound dogs. Spine 9:702–706. https://doi.org/10.1097/00007632-198410000-00009
Urban JP, Holm S, Maroudas A (1978) Diffusion of small solutes into the intervertebral disc: as in vivo study. Biorheology 15:203–221. https://doi.org/10.3233/bir-1978-153-409
Siemionow K, An H, Masuda K, Andersson G, Cs-Szabo G (2011) The effects of age, sex, ethnicity, and spinal level on the rate of intervertebral disc degeneration: a review of 1712 intervertebral discs. Spine 36:1333–1339. https://doi.org/10.1097/BRS.0b013e3181f2a177
Joe E, Lee JW, Park KW, Yeom JS, Lee E, Lee GY, Kang HS (2015) Herniation of cartilaginous endplates in the lumbar spine: MRI findings. AJR Am J Roentgenol 204:1075–1081. https://doi.org/10.2214/AJR.14.13319
Robson MD, Gatehouse PD, Bydder M, Bydder GM (2003) Magnetic resonance: an introduction to ultrashort TE (UTE) imaging. J Comput Assist Tomogr 27:825–846. https://doi.org/10.1097/00004728-200311000-00001
Bae WC, Biswas R, Chen K, Chang EY, Chung CB (2014) UTE MRI of the osteochondral junction. Curr Radiol Rep 2:35. https://doi.org/10.1007/s40134-013-0035-7
Chen KC, Tran B, Biswas R, Statum S, Masuda K, Chung CB, Bae WC (2016) Evaluation of the disco-vertebral junction using ultrashort time-to-echo magnetic resonance imaging: inter-reader agreement and association with vertebral endplate lesions. Skeletal Radiol 45:1249–1256. https://doi.org/10.1007/s00256-016-2413-8
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26:1873–1878
Marinelli NL, Haughton VM, Munoz A, Anderson PA (2009) T2 relaxation times of intervertebral disc tissue correlated with water content and proteoglycan content. Spine (Phila Pa 1976) 34:520–524. https://doi.org/10.1097/BRS.0b013e318195dd44
Berg-Johansen B, Han M, Fields AJ, Liebenberg EC, Lim BJ, Larson PE, Gunduz-Demir C, Kazakia GJ, Krug R, Lotz JC (2018) Cartilage endplate thickness variation measured by ultrashort echo-time MRI is associated with adjacent disc degeneration. Spine 43:E592–E600. https://doi.org/10.1097/BRS.0000000000002432
Law T, Anthony MP, Chan Q, Samartzis D, Kim M, Cheung KM, Khong PL (2013) Ultrashort time-to-echo MRI of the cartilaginous endplate: technique and association with intervertebral disc degeneration. J Med Imaging Radiat Oncol 57:427–434. https://doi.org/10.1111/1754-9485.12041
Bae WC, Statum S, Zhang Z, Yamaguchi T, Wolfson T, Gamst AC, Du J, Bydder GM, Masuda K, Chung CB (2013) Morphology of the cartilaginous endplates in human intervertebral disks with ultrashort echo time MR imaging. Radiology 266:564–574. https://doi.org/10.1148/radiol.12121181
Obata S, Akeda K, Imanishi T, Masuda K, Bae W, Morimoto R, Asanuma Y, Kasai Y, Uchida A, Sudo A (2012) Effect of autologous platelet-rich plasma-releasate on intervertebral disc degeneration in the rabbit anular puncture model: a preclinical study. Arthritis Res Ther 14:R241. https://doi.org/10.1186/ar4084
Marinelli NL, Haughton VM, Anderson PA (2010) T2 relaxation times correlated with stage of lumbar intervertebral disk degeneration and patient age. AJNR Am J Neuroradiol 31:1278–1282. https://doi.org/10.3174/ajnr.A2080
Roberts S, Menage J, Urban JP (1989) Biochemical and structural properties of the cartilage end-plate and its relation to the intervertebral disc. Spine (Phila Pa 1976) 14:166–174
van der Werf M, Lezuo P, Maissen O, van Donkelaar CC, Ito K (2007) Inhibition of vertebral endplate perfusion results in decreased intervertebral disc intranuclear diffusive transport. J Anat 211:769–774. https://doi.org/10.1111/j.1469-7580.2007.00816.x
Urban MR, Fairbank JC, Etherington PJ, Loh FL, Winlove CP, Urban JP (2001) Electrochemical measurement of transport into scoliotic intervertebral discs in vivo using nitrous oxide as a tracer. Spine 26:984–990
Kitano T, Zerwekh JE, Usui Y, Edwards ML, Flicker PL, Mooney V (1993) Biochemical changes associated with the symptomatic human intervertebral disk. Clin Orthop Relat Res 372–377
Bernick S, Cailliet R (1982) Vertebral end-plate changes with aging of human vertebrae. Spine (Phila Pa 1976) 7:97–102
Bae WC, Xu K, Inoue N, Bydder GM, Chung CB, Masuda K (2010) Ultrashort time-to-echo MRI of human intervertebral disc endplate: association with endplate calcification. Proc Int’l Soc Magn Reson Med 18:3218
Calvo E, Palacios I, Delgado E, Sanchez-Pernaute O, Largo R, Egido J, Herrero-Beaumont G (2004) Histopathological correlation of cartilage swelling detected by magnetic resonance imaging in early experimental osteoarthritis. Osteoarthritis Cartilage 12:878–886. https://doi.org/10.1016/j.joca.2004.07.007
Funding
The funding was provided by NIH NIAMS (AR066622, AR073761), RSNA Research and Education Foundation (RF1730), Swiss National Science Foundation (P2SKP3_16412), and Swiss Society of Radiology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest regarding the content of this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Finkenstaedt, T., Siriwananrangsun, P., Masuda, K. et al. Ultrashort time-to-echo MR morphology of cartilaginous endplate correlates with disc degeneration in the lumbar spine. Eur Spine J 32, 2358–2367 (2023). https://doi.org/10.1007/s00586-023-07739-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07739-9