Abstract
Purpose
The aim of this study was to compare the clinical and radiographical outcomes between OLIF and ALIF in treating lumbar degenerative diseases.
Methods
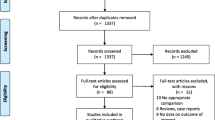
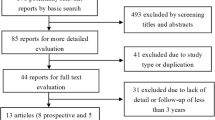
We searched PubMed, Embase, Web of Science, and Cochrane Library for relevant studies. Changes in disc height (DH), segmental lordosis angle (SLA), lumbar lordosis (LL), visual analogue scale (VAS) score, and Oswestry disability index (ODI) between baseline and final follow-up, along with other important surgical outcomes, were assessed and analysed. Data on the global fusion rate and main complications were collected and compared.
Results
Approximately, 2041 patients from 36 studies were included, consisting of 1057 patients who underwent OLIF and 984 patients who underwent ALIF. The results reveal no significant difference in DH, SLA, VAS score, and ODI between the two groups (all P > 0.05). The operation time, estimated blood loss, and length of hospital stay were also comparable between the two groups. Over 90% of the fusion rate was achieved in both groups. The OLIF group showed a higher complication rate than the ALIF group (OLIF 18.83% vs ALIF 7.32%).
Conclusions
OLIF leads to a higher complication rate, with the most notable complication being cage subsidence. Both OLIF and ALIF are effective treatments for degenerative lumbar diseases and have similar therapeutic effects. ALIF was expected to be more expensive for patients because of the necessity of involving vascular surgeons.

Similar content being viewed by others
References
Fan SW, Hu ZJ, Fang XQ, Zhao FD, Huang Y, Yu HJ (2010) Comparison of paraspinal muscle injury in one-level lumbar posterior inter-body fusion: modified minimally invasive and traditional open approaches. Orthop Surg 2:194–200. https://doi.org/10.1111/j.1757-7861.2010.00086.x
Han B, Liang W, Hai Y, Liu Y, Chen Y, Ding H, Yin P (2022) Elucidating the potential mechanisms underlying distraction spinal cord injury-associated neuroinflammation and apoptosis. Front Cell Dev Biol 10:839313. https://doi.org/10.3389/fcell.2022.839313
Allain J, Dufour T (2020) Anterior lumbar fusion techniques: ALIF, OLIF, DLIF, LLIF, IXLIF. Orthop Traumatol Surg Res 106:S149–S157. https://doi.org/10.1016/j.otsr.2019.05.024
Teng I, Han J, Phan K, Mobbs R (2017) A meta-analysis comparing ALIF, PLIF, TLIF and LLIF. J Clin Neurosci 44:11–17. https://doi.org/10.1016/j.jocn.2017.06.013
Manunga J, Alcala C, Smith J, Mirza A, Titus J, Skeik N, Senthil J, Stephenson E, Alexander J, Sullivan T (2021) Technical approach, outcomes, and exposure-related complications in patients undergoing anterior lumbar interbody fusion. J Vasc Surg 73:992–998. https://doi.org/10.1016/j.jvs.2020.06.129
Xi Z, Burch S, Mummaneni PV, Chang CC, Ruan H, Eichler C, Chou D (2020) Supine anterior lumbar interbody fusion versus lateral position oblique lumbar interbody fusion at L5–S1: a comparison of two approaches to the lumbosacral junction. J Clin Neurosci 82:134–140. https://doi.org/10.1016/j.jocn.2020.10.043
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J spine surg 1(1):2
Guerin P, Obeid I, Bourghli A, Masquefa T, Luc S, Gille O, Pointillart V, Vital JM (2012) The lumbosacral plexus: anatomic considerations for minimally invasive retroperitoneal transpsoas approach. Surg Radiol Anat 34:151–157. https://doi.org/10.1007/s00276-011-0881-z
Chung HW, Lee HD, Jeon CH, Chung NS (2021) Comparison of surgical outcomes between oblique lateral interbody fusion (OLIF) and anterior lumbar interbody fusion (ALIF). Clin Neurol Neurosurg 209:106901. https://doi.org/10.1016/j.clineuro.2021.106901
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hrobjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 134:178–189. https://doi.org/10.1016/j.jclinepi.2021.03.001
Rickert M, Fleege C, Papachristos I, Makowski MR, Rauschmann M, Arabmotlagh M (2019) Clinical outcome after anterior lumbar interbody fusion with a new osteoinductive bone substitute material: a randomized clinical pilot study. Clin Spine Surg 32:E319–E325. https://doi.org/10.1097/BSD.0000000000000802
Zeng ZY, Xu ZW, He DW, Zhao X, Ma WH, Ni WF, Song YX, Zhang JQ, Yu W, Fang XQ, Zhou ZJ, Xu NJ, Huang WJ, Hu ZC, Wu AL, Ji JF, Han JF, Fan SW, Zhao FD, Jin H, Pei F, Fan SY, Sui DX (2018) Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg 10:98–106. https://doi.org/10.1111/os.12380
Hung SF, Liao JC, Tsai TT, Li YD, Chiu PY, Hsieh MK, Kao FC (2021) Comparison of outcomes between indirect decompression of oblique lumbar interbody fusion and MIS-TLIF in one single-level lumbar spondylosis. Sci Rep 11:12783. https://doi.org/10.1038/s41598-021-92330-9
Jin C, Jaiswal MS, Jeun SS, Ryu KS, Hur JW, Kim JS (2018) Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J Orthop Surg Res 13:38. https://doi.org/10.1186/s13018-018-0740-2
Shimizu T, Fujibayashi S, Otsuki B, Murata K, Matsuda S (2021) Indirect decompression via oblique lateral interbody fusion for severe degenerative lumbar spinal stenosis: a comparative study with direct decompression transforaminal/posterior lumbar interbody fusion. Spine J 21:963–971. https://doi.org/10.1016/j.spinee.2021.01.025
Wen J, Shi C, Yu L, Wang S, Xi Y, Ye X (2020) Unilateral versus bilateral percutaneous pedicle screw fixation in oblique lumbar interbody fusion. World Neurosurg 134:e920–e927. https://doi.org/10.1016/j.wneu.2019.11.035
Xiao L, Zhao Q, Sun X, Liu C, Zhang Y, Xu H (2020) Relationship between alterations of spinal/pelvic sagittal parameters and clinical outcomes after oblique lumbar interbody fusion. World Neurosurg 133:e156–e164. https://doi.org/10.1016/j.wneu.2019.08.158
Kotani Y, Ikeura A, Tokunaga H, Saito T (2021) Single-level controlled comparison of OLIF51 and percutaneous screw in lateral position versus MIS-TLIF for lumbosacral degenerative disorders: clinical and radiologic study. J Orthop Sci 26:756–764. https://doi.org/10.1016/j.jos.2020.08.005
Miscusi M, Trungu S, Ricciardi L, Forcato S, Ramieri A, Raco A (2020) The anterior-to-psoas approach for interbody fusion at the L5–S1 segment: clinical and radiological outcomes. Neurosurg Focus 49:E14. https://doi.org/10.3171/2020.6.FOCUS20335
Jung J, Lee S, Cho DC, Han IB, Kim CH, Lee YS, Kim KT (2021) Usefulness of oblique lumbar interbody fusion as revision surgery: comparison of clinical and radiological outcomes between primary and revision surgery. World Neurosurg 149:e1067–e1076. https://doi.org/10.1016/j.wneu.2020.12.172
Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kuniyoshi K, Aoki Y, Nakamura J, Miyagi M, Suzuki M, Kubota G, Inage K, Sainoh T, Fujimoto K, Shiga Y, Abe K, Kanamoto H, Inoue G, Takahashi K (2017) Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J 26:671–678. https://doi.org/10.1007/s00586-015-4170-0
DiGiorgio AM, Edwards CS, Virk MS, Mummaneni PV, Chou D (2017) Stereotactic navigation for the prepsoas oblique lateral lumbar interbody fusion: technical note and case series. Neurosurg Focus 43:E14. https://doi.org/10.3171/2017.5.FOCUS17168
Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S (2015) Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine 40:175–182. https://doi.org/10.1097/BRS.0000000000000703
Miscusi M, Ramieri A, Forcato S, Giuffre M, Trungu S, Cimatti M, Pesce A, Familiari P, Piazza A, Carnevali C, Costanzo G, Raco A (2018) Comparison of pure lateral and oblique lateral inter-body fusion for treatment of lumbar degenerative disk disease: a multicentric cohort study. Eur Spine J 27:222–228. https://doi.org/10.1007/s00586-018-5596-y
Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Aoki Y, Nakamura J, Ishikawa T, Miyagi M, Kamoda H, Suzuki M, Kubota G, Sakuma Y, Oikawa Y, Inage K, Sainoh T, Sato J, Fujimoto K, Shiga Y, Abe K, Toyone T, Inoue G, Takahashi K (2015) Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J 56:1051–1059. https://doi.org/10.3349/ymj.2015.56.4.1051
Li R, Shao X, Li X, Liu Y, Jiang W (2021) Comparison of clinical outcomes and spino-pelvic sagittal balance in degenerative lumbar spondylolisthesis: minimally invasive oblique lumbar interbody fusion (OLIF) versus transforaminal lumbar interbody fusion (TLIF). Medicine 100:e23783. https://doi.org/10.1097/MD.0000000000023783
Yang Z, Chang J, Sun L, Chen CM, Feng H (2020) Comparing oblique lumbar interbody fusion with lateral screw fixation and transforaminal full-endoscopic lumbar discectomy (OLIF-TELD) and posterior lumbar interbody fusion (PLIF) for the treatment of adjacent segment disease. Biomed Res Int 2020:4610128. https://doi.org/10.1155/2020/4610128
Malham GM, Parker RM, Blecher CM, Chow FY, Seex KA (2016) Choice of approach does not affect clinical and radiologic outcomes: a comparative cohort of patients having anterior lumbar interbody fusion and patients having lateral lumbar interbody fusion at 24 months. Global Spine J 6:472–481. https://doi.org/10.1055/s-0035-1569055
Bassani R, Morselli C, Querenghi AM, Nuara A, Sconfienza LM, Peretti GM (2020) Functional and radiological outcome of anterior retroperitoneal versus posterior transforaminal interbody fusion in the management of single-level lumbar degenerative disease. Neurosurg Focus 49:E2. https://doi.org/10.3171/2020.6.FOCUS20374
Szadkowski M, d’Astorg H, Bouhali H, Aleksic I, Ramos-Pascual S, Fiere V (2020) Outcomes of stand-alone anterior lumbar interbody fusion of L5–S1 using a novel implant with anterior plate fixation. Spine J 20:1618–1628. https://doi.org/10.1016/j.spinee.2020.05.555
Mobbs RJ, Maharaj M, Rao PJ (2014) Clinical outcomes and fusion rates following anterior lumbar interbody fusion with bone graft substitute i-FACTOR, an anorganic bone matrix/P-15 composite. J Neurosurg Spine 21:867–876. https://doi.org/10.3171/2014.9.SPINE131151
Norotte G, Barrios C (2018) Clinical and radiological outcomes after stand-alone ALIF for single L5–S1 degenerative discopathy using a PEEK cage filled with hydroxyapatite nanoparticles without bone graft. Clin Neurol Neurosurg 168:24–29. https://doi.org/10.1016/j.clineuro.2018.01.037
Pavlov PW, Meijers H, van Limbeek J, Jacobs WC, Lemmens JA, Obradov-Rajic M, de Kleuver M (2004) Good outcome and restoration of lordosis after anterior lumbar interbody fusion with additional posterior fixation. Spine 29:1893–1899. https://doi.org/10.1097/01.brs.0000137067.68630.70
Kim JS, Kim DH, Lee SH, Park CK, Hwang JH, Cheh G, Choi YG, Kang BU, Lee HY (2010) Comparison study of the instrumented circumferential fusion with instrumented anterior lumbar interbody fusion as a surgical procedure for adult low-grade isthmic spondylolisthesis. World Neurosurg 73:565–571. https://doi.org/10.1016/j.wneu.2010.02.057
Kleeman TJ, Ahn UM, Talbot-Kleeman A (2001) Laparoscopic anterior lumbar interbody fusion with rhBMP-2: a prospective study of clinical and radiographic outcomes. Spine 26:2751–2756. https://doi.org/10.1097/00007632-200112150-00026
Shim JH, Kim WS, Kim JH, Kim DH, Hwang JH, Park CK (2011) Comparison of instrumented posterolateral fusion versus percutaneous pedicle screw fixation combined with anterior lumbar interbody fusion in elderly patients with L5–S1 isthmic spondylolisthesis and foraminal stenosis. J Neurosurg Spine 15:311–319. https://doi.org/10.3171/2011.4.SPINE10653
Phan K, Davies S, Rao PJ, Mobbs RJ (2017) Worker’s compensation status and outcomes following anterior lumbar interbody fusion: prospective observational study. World Neurosurg 103:680–685. https://doi.org/10.1016/j.wneu.2017.04.123
Chung SK, Lee SH, Lim SR, Kim DY, Jang JS, Nam KS, Lee HY (2003) Comparative study of laparoscopic L5–S1 fusion versus open mini-ALIF, with a minimum 2-year follow-up. Eur Spine J 12:613–617. https://doi.org/10.1007/s00586-003-0526-y
Moses ZB, Razvi S, Oh SY, Platt A, Keegan KC, Hamati F, Witiw C, David BT, Fontes RBV, Deutsch H, O’Toole JE, Fessler RG (2021) A retrospective comparison of radiographic and clinical outcomes in single-level degenerative lumbar disease undergoing anterior versus transforaminal lumbar interbody fusion. J Spine Surg 7:170–180. https://doi.org/10.21037/jss-20-673
Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7:379–386. https://doi.org/10.3171/SPI-07/10/379
Jaeger A, Giber D, Bastard C, Thiebaut B, Roubineau F, Flouzat Lachaniette CH, Dubory A (2019) Risk factors of instrumentation failure and pseudarthrosis after stand-alone L5–S1 anterior lumbar interbody fusion: a retrospective cohort study. J Neurosurg Spine 31:338–346. https://doi.org/10.3171/2019.3.SPINE181476
Zhang C, Wang K, Jian F, Wu H (2018) Efficacy of oblique lateral interbody fusion in treatment of degenerative lumbar disease. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.11.139
Heo DH, Kim JS (2017) Clinical and radiological outcomes of spinal endoscopic discectomy-assisted oblique lumbar interbody fusion: preliminary results. Neurosurg Focus 43:E13. https://doi.org/10.3171/2017.5.FOCUS17196
Crandall DG, Revella J (2009) Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: three year clinical and radiographic outcomes. Spine 34:2126–2133. https://doi.org/10.1097/BRS.0b013e3181b612db
Yoshida G, Hasegawa T, Yamato Y, Kobayashi S, Shin O, Banno T, Mihara Y, Arima H, Ushirozako H, Yasuda T, Togawa D, Matsuyama Y (2019) Minimum clinically important differences in oswestry disability index domains and their impact on adult spinal deformity surgery. Asian Spine J 13:35–44. https://doi.org/10.31616/asj.2018.0077
Otsuki B, Fujibayashi S, Takemoto M, Kimura H, Shimizu T, Murata K, Matsuda S (2020) Analysis of the factors affecting lumbar segmental lordosis after lateral lumbar interbody fusion. Spine 45:E839–E846. https://doi.org/10.1097/BRS.0000000000003432
Regev GJ, Haloman S, Chen L, Dhawan M, Lee YP, Garfin SR, Kim CW (2010) Incidence and prevention of intervertebral cage overhang with minimally invasive lateral approach fusions. Spine 35:1406–1411. https://doi.org/10.1097/BRS.0b013e3181c20fb5
Watkins RG, Hanna R, Chang D, Watkins RG (2014) Sagittal alignment after lumbar interbody fusion: comparing anterior, lateral, and transforaminal approaches. J Spinal Disord Tech 27:253–256. https://doi.org/10.1097/BSD
Choi MK, Kim SM, Jo DJ (2020) Anterior lumbar interbody fusions combined with posterior column osteotomy in patients who had sagittal imbalance associated with degenerative lumbar flat-back deformity: a retrospective case series. Neurosurg Rev 43:1117–1125. https://doi.org/10.1007/s10143-019-01129-w
Yoshihara H (2017) Indirect decompression in spinal surgery. J Clin Neurosci 44:63–68. https://doi.org/10.1016/j.jocn.2017.06.061
Cho W, Sokolowski MJ, Mehbod AA, Denis F, Garvey TA, Perl J, Transfeldt EE (2013) MRI measurement of neuroforaminal dimension at the index and supradjacent levels after anterior lumbar interbody fusion: a prospective study. Clin Orthop Surg 5:49–54. https://doi.org/10.4055/cios.2013.5.1.49
Rao PJ, Maharaj MM, Phan K, Lakshan Abeygunasekara M, Mobbs RJ (2015) Indirect foraminal decompression after anterior lumbar interbody fusion: a prospective radiographic study using a new pedicle-to-pedicle technique. Spine J 15:817–824. https://doi.org/10.1016/j.spinee.2014.12.019
Kotheeranurak V, Jitpakdee K, Lin GX, Mahatthanatrakul A, Singhatanadgige W, Limthongkul W, Yingsakmongkol W, Kim JS (2021) Subsidence of interbody cage following oblique lateral interbody fusion: an analysis and potential risk factors. Global Spine J. https://doi.org/10.1177/21925682211067210
Funding
This study was supported by grants from the National Key Research and Development Program of China (No.2019YFC0120604), and the Innovation Grant of the National Clinical Research Center for Orthopedics, Sports Medicine & Rehabilitation (No2021-NCRC-CXJJ-PY-34).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Consent to participate
We state that we have consented to participate.
Consent for publication
We state that we have consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, D., Liang, W., Hai, Y. et al. OLIF versus ALIF: Which is the better surgical approach for degenerative lumbar disease? A systematic review. Eur Spine J 32, 689–699 (2023). https://doi.org/10.1007/s00586-022-07516-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07516-0