Abstract
Purpose
Posterior instrumentation is the state-of-the-art surgical treatment for fractures of the thoracic and lumbar spine. Options for pedicle screw placement comprise open or minimally invasive techniques. Open instrumentation causes large approach related muscle detachment, which minimally invasive techniques aim to reduce. However, concerns of accurate pedicle screw placement are still a matter of debate. Beside neurological complications due to pedicle screw malplacement, also affection of the facet joints and thus motion dependent pain is known as a complication. The aim of this study was to assess accuracy of pedicle screw placement concerning facet joint violation (FJV) after open- and minimally invasive posterior instrumentation.
Methods
A retrospective data analysis of postoperative computer tomographic scans of 219 patients (1124 pedicle screws) was conducted. A total of 116 patients underwent open screw insertion (634 screws) and 103 patients underwent minimally invasive, percutaneous screw insertion (490 screws).
Results
In the lumbar spine (segments L3, L4, L5), there were significantly more and higher grade (open = 0.55 vs. percutaneous = 1.2; p = 0.001) FJV’s after percutaneously compared to openly inserted screws. In the thoracic spine, no significant difference concerning rate and grade of FJV was found (p > 0.56).
Conclusion
FJV is more likely to occur in percutaneously placed pedicle screws. Additionally, higher grade FJV’s occur after percutaneous instrumentation. However, in the thoracic spine we didn’t find a significant difference between open and percutaneous technique. Our results suggest a precise consideration concerning surgical technique according to the fractured vertebrae in the light of the individual anatomic structures in the preop CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Posterior instrumentation is the gold standard for the surgical treatment of unstable traumatic fractures of the thoracic and lumbar vertebral columns. Exact anatomical pedicle screw placement is a prerequisite for avoiding complications such as neurological complications and facet joint violation (FJV). FJVs have different clinical and therapeutic consequences that are dependent on the surgical procedure, whether it involves posterior instrumentation and interbody fusion (bone augmentation or cage implantation) or just temporary posterior instrumentation with planned removal of fixation hardware. In patients with posterior instrumentation and interbody fusion, only the most cranial facet joint is therapeutically relevant for FJV. In patients with temporary fixation, however, every facet joint will be affected if FJV is present. FJV can cause pain, instability and adjacent segment degeneration [1, 2]. There are also cases of segment arthrosis due to FJV after posterior instrumentation with later progression of back pain of the initial only temporarily stabilized segments [3].
In addition to the conventional open technique (OT) for pedicle screw insertion, minimally invasive procedures have been established for percutaneous pedicle screw insertion (PT) techniques [4]. OT requires large dissection and muscle retraction to identify the exact entry point of the pedicle screw, which can lead to muscle damage, atrophy and increased blood loss but allows a good overview of the surgical field and landmarks for accurate pedicle screw insertion [4,5,6]. However, cortical perforation rates are reported to occur in up to 40%, and cranial facet joint violation (CFJV) rates are described to be up to 100%, depending on which pedicle insertion technique is used [7]. A cadaveric study with 48 percutaneous screws reported FJV rates up to 58% [8]. However, these data have not been verified when directly compared in clinical appliances with open screw placement.
In the PT, less surgical trauma avoids extended soft tissue damage. Therefore, this may lead to faster recovery, faster remobilization and lower postoperative pain [4, 9,10,11]. On the other hand, limited access and limited view to the surgical field raise the concern of reduced accuracy in pedicle screw placement. Therefore, the insertion of pedicle screws relies on image guidance as the sole means.
Navigation for pedicle screw placement may allow higher accuracy in pedicle screw positioning but has its drawbacks due to cost- and time-intensity [12, 13] as well as reported malplacement [14].
Material and methods
Research question
Facet joint violation in patients undergoing posterior instrumentation of the thoracic or lumbar spine has been described in several studies [7, 15, 16]. However, data in the literature are controversial, especially when comparing open and minimally invasive surgical techniques. We suppose that minimally invasive pedicle screw placement in favor of less surgical morbidity comes with a higher risk of FJV compared to open surgery.
Study design
In this retrospective study, we identified risk factors for FJV and compared the rate and grade of FJV after open and percutaneous posterior instrumentation for traumatic thoracic and lumbar spinal fractures. FJV was determined by postoperative computed tomography scans (CT) and was graded according to a previously published grading system by Babu et al. [17].
Patients and study design
We retrospectively investigated all patients who underwent posterior pedicle screw stabilization for traumatic fractures of the thoracic and/or lumbar spine from April 2014–April 2015. A total of 277 patients were identified, of which 219 received pre- and postoperative CT images and thus were included in this study. The decision about whether a patient was operated on via an open or percutaneous approach was left to the surgeon and was not randomized or blinded.
Surgical technique
All surgical procedures were performed at the authors´ institution by experienced traumatology surgeons. All procedures were performed using the Universal Spinal System USS (DePuy Synthes, Switzerland) or the S4 System (Braun Aesculap, Melsungen, Germany).
For the open group, a classic standard posterior approach was used through a midline incision. After dissection of the fascia, the musculature was detached from the posterior aspects of the spine, and facet joints were exposed. In the thoracic spine, the entry point of the pedicle screw was just below the rim of the upper facet joint and approximately 3 mm lateral to the center of the joint near the base of the transverse process. The screws converged 10° to the midline and 10°–20° caudally, depending on preoperative CT evaluation and intraoperative fluoroscopic guidance. The entry point in the lumbar spine was at the intersection of a vertical line tangential to the lateral border of the superior articular process and a horizontal line bisecting the transverse process. The trajectory of the pedicle screws converged 10° in the upper lumbar spine and 10° in the lower lumbar spine, according to preoperative CT images and intraoperative fluoroscopic guidance. The entry point and progression of pedicle screw insertion were additionally controlled with an image intensifier in 2 planes (AP and lateral view) for all pedicle screws.
For the minimally invasive, percutaneous pedicle screw insertion, skin incisions were made slightly lateral to the pedicles after fluoroscopic identification of the pedicle eye. After dissecting the subcutis and the fascia, a Jamshidi needle was used to penetrate the pedicle at the cranio-lateral third of the pedicle eye under fluoroscopic guidance. Under fluoroscopic guidance, the needle was advanced through the pedicle up to the vertebral body.
The selection of screw diameter was based on preoperative CT measurements. Length was measured using preoperative CT images and was confirmed intraoperatively.
In both techniques, the screw with the largest diameter and the highest length was always targeted.
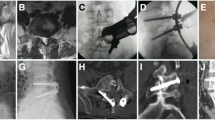
Radiological evaluation
All CT scans were performed using a 64 slice Somatom Sensation 64CT scanner (Siemens, Erlangen Germany). Slices of 1 mm with a pitch factor of 0.75 mm were obtained for axial, sagittal and coronal reconstruction in all CT scans. For image evaluation, IMPAX EE R20 VIII software (Agfa HealthCare, Mortsel, Belgium) was used. FJV was graded according to Babu et al. [17] (Fig. 1).
Grade of FJV according to Babu et al. [17]
The FJV was evaluated in the sagittal and coronal planes. Pedicle screws without any contact with the facet joint were graded as 0. Pedicle screws intruding the border on the lateral, cranial facet joint were graded as 1. Pedicle screws that violated the articular facet joint surface were graded as 2, and screws lying within the facet joint were graded as 3.
Statistical analysis
Data were checked for consistency, and distributions were analyzed for normality, binomial and Poisson distributions. Because several levels of each patient were measured, generalized estimation equation models based on binomial, Poisson and normal distributions together with the identity function were used to analyze the data. Pairwise comparisons were performed, and corresponding 95% confidence intervals were computed for the effects. All reported tests were two-sided, and p values < 0.05 were considered as statistically significant. All statistical analyses in this report were performed using PASW 22 (IBM SPSS Statistics for Windows, Version 21.0., Armonk, NY).
Results
A total of 277 patients were identified, of which 219 received pre- and postoperative computer tomographic (CT) images and thus were included in this study. The overall mean age was 53 ± 19a (16–90) years. Seventy-nine (36.1%) of the patients were women, and 140 (63.9%) were men. A total of 116 (53%) of the patients underwent open- and 103 (47%) percutaneous posterior instrumentation.
The mean age in the OT—group was 50.2 years and 54 years in the PT—group and did not differ significantly (p = 0.13). Overall, 563 vertebrae (OT vs. PT: n = 318 vs. n = 245) were stabilized with 1124 pedicle screws (OT vs. PT: n = 634 vs. n = 490). The surgical indications for stabilization were fracture of a single vertebra in 145 patients (66.2%) and two or more segments in 74 patients (33.8%). Eighty-nine patients (40.6%) were treated for fractures of the thoracic spine and 130 patients (59.4%) for fractures of the lumbar spine.
Overall, in 66% of the patients, 1 vertebral body was fractured, in 25% 2 were fractured, in 7.6% 3 were fractured, in 0.4% 5 were fractured, and in 0.7% 7 vertebrae were fractured.
Four pedicle screws were used in 51% of patients, eight screws were used in 26.6%, six screws were used in 13.9%, ten screws were used in 5%, twelve screws were used in 2%, five screws were used in 1.1% and three screws were used in 0.4%. There was a significant difference between the number of pedicle screws and age. The mean age of patients with 4 pedicle screws was 47.3 years (CI 46.3–52.1), the mean age of patients who received 8 screws was 61.7 years (CI 56.4–67) and the mean age of patients with 12 screws was 81.1 years (CI 79.8–82.5) (p < 0.001).
The number of fracture levels differed significantly (p = 0.001) and was 1.5 (CI 1.4–1.7) in the OT group and 1.2 (CI 1.1–1.3) in the PT group.
In the OT—group, a mean of 5.6 screws (CI 5.22–6.9) were used compared to 4.8 screws (CI 4.5–5.1) in the PT—group (p = 0.001).
Intraoperative screw change due to an incorrect screw position or incorrect screw length was performed in 24 cases (11.0%), with no difference in the change rate between the OT and PT groups (p = 0.18).
FJV occurred in 16.5% (185) of all pedicle screws, [OT: = 84 (13.2%) vs. PT 101 (20.6%); p = 0.04]. The mean grade of FJV was 0.83 (mean, 95% CI 0.65–1.1; range 0–4) for the PT—group and 0.59 (CI 0.48–0.71, range 0–4) for the OT—group (p = 0.033) (Table 1).
In the thoracic spine, there were no significant differences in FJV between the OT and PT groups (p > 0.5). In the lumbar spine, at levels L3, L4, and L5, there were significantly higher grade FJVs in the PT- group than in the OT- group (percutaneous: 1.2 vs. open: 0.55, p = 0.001).
No correlation was found for FJV and patient age, sex or number of screws.
Discussion
In this study, we investigated the FJV rate after open and percutaneous posterior instrumentation. We found an overall FJV rate of 16.5% (OT = 13.2% vs. PT = 20.6%). The results for FJV rates in the literature vary widely. In a study by Chen et al. [7], the authors found superior facet joint violation in 100% of patients treated with the Roy-Camille technique and approximately 25% after the Weinstein technique. In another study by Knox et al. [15], the authors found FJV in approximately 11% of patients after minimally invasive, percutaneous pedicle screw placement in the lumbar spine. In a study by Moshirfar et al. [16], the authors found FJV in 24% of patients and 15% of pedicle screws.
In our study, FJV occurred significantly more often in the percutaneous group. Additionally, significantly higher grade FJV was found in the percutaneous group. A possible explanation for the higher rate of FJVs using the percutaneous technique might be that the skin incision for pedicle screw insertion is often lateral to the border of the pedicle. Therefore, it may be more difficult to find the correct entry point, especially in the lower lumbar vertebrae with higher convergence of pedicles, using the percutaneous technique with restricted vision of the surgical field.
In a recently published quantitative comparative meta-analysis from Wang et al. [18], the authors found no significant difference in the FJV rate between percutaneous and open posterior instrumentation in the lumbar spine in 881 patients and 1755 pedicle screws (OR 0.75, 95% CI 0.24–2.30, p = 0.62). Additionally, they found no difference in the rate of severe violation between the two groups (OR 1.20, 95% CI 0.55–2.62, p = 0.64). The FJV rate was 18% (154/847) in the percutaneous group and 19% (170/918) in the open group, which is concordant with our findings in the PT group of our cohort of trauma patients. However, the number of FJVs in the OT group of the current study was relevantly lower than the reported number by Wang et al. [18] (OT = 13.2% vs. 18.7% and PT = 20.6% vs. 18.2%).
In a study by Jones-Quaidoo et al. [19], the authors found in a comparative study significantly more FJV in the percutaneous group (13.6%) than in an openly operated group (6%, p = 0.005). Park et al. [4] found an incidence of 50% FJV after percutaneously placed pedicle screws in the lumbar spine.
In a study by Babu et al. [17], the authors found that FJV was more likely to occur in the percutaneous group than in the open group. Furthermore, the authors found significantly higher grade FJVs in the percutaneous group according to their classification system than in the open group (0.62 vs. 0.45). However, those numbers are lower than our findings of 0.89 for the percutaneous group and 0.53 for the open group.
Unlike in the lumbar spine, there were no differences in the incidence of FJV in the thoracic spine between the two groups in our study. This might be mainly due to the anatomy of the thoracic spine. The pedicles in the thoracic spine are less convergent and lie more in a vertical line, which makes it easier to identify the correct trajectory, and the facet joints are oriented more medially and thus at lower risk for being affected. Furthermore, there is less risk for clinical consequence due to reduced mobility of the thoracic segments.
There are reports that CT and fluoroscopy-guided navigation systems or robotic spinal surgery increase screw accuracy and reduce operation time as well as radiation exposure during surgery [20, 21]. However, the literature is still nonhomogeneous. In a study published by Ringel et al. [14], robot-assisted spinal surgery of the lumbar and sacral spine had a higher rate of screw malposition and longer screw placement time but equal intraoperative radiation [14]. In a large systematic review by Gelalis, benefits for pedicle screw navigation compared to free-hand pedicle screw placement and fluoroscopy placement were shown [22]. However, navigation systems are not ubiquitously accessible due to their cost and time intensity and have previously mentioned limitations [14].
In a study by Yson et al. [23], the authors investigated FJV between an open and percutaneous group rate in 370 pedicle screws (245 open, 125 percutaneous) using intraoperative 3-D CT (o-arm). The authors found an overall FJV rate of 18.9% and a significantly lower rate of FJVs in the percutaneous group (open 26.5% vs. percutaneous 4%; p < 0.0001) as well as an increasing rate of FJVs from L1 to L5. The authors additionally conducted a literature review and calculated a pooled weighted mean of FJV of 27% for the percutaneous technique and 23% for open pedicle insertion.
The main limitation of this study is its retrospective design and its lack of randomization. Multiple surgeons performed the surgeries, and no analysis of potential risk factors for FJV, such as scoliosis, body mass index or previous surgeries, was performed.
Conclusion
In this study, we found that FJV is more likely to occur in percutaneously placed pedicle screws. Additionally, more severe FJVs occur after percutaneously inserted pedicle screws. However, in the thoracic spine, we did not find a significant difference between the open and percutaneous techniques. Therefore, especially in cases with challenging anatomical aspects, open screw placement should be considered to avoid FJV, especially in the lumbar spine. Navigated percutaneous screw placement might be a beneficial option to use in such challenging cases.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Aota Y, Kumano K, Hirabayashi S (1995) Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord 8:464–473
Krag MH (1991) Biomechanics of thoracolumbar spinal fixation. A review. Spine 16:S84-99
Tromme A, Charles YP, Schuller S, Walter A, Schaeffer M, Steib J-P (2019) Osteoarthritis and spontaneous fusion of facet joints after percutaneous instrumentation in thoracolumbar fractures. Eur Spine J 28:1121–1129. https://doi.org/10.1007/s00586-017-5173-9
Park Y, Ha JW (2007) Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine 32:537–543. https://doi.org/10.1097/01.brs.0000256473.49791.f4
Thomsen K, Christensen FB, Eiskjaer SP et al (1997) 1997 Volvo award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine 22:2813–2822
Kawaguchi Y, Matsui H, Tsuji H (1996) Back muscle injury after posterior lumbar spine surgery: a histologic and enzymatic analysis. Spine 21:941–944
Chen Z, Zhao J, Xu H et al (2008) Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 17:1476–1480. https://doi.org/10.1007/s00586-008-0776-9
Patel RD, Graziano GP, Vanderhave KL et al (2011) Facet violation with the placement of percutaneous pedicle screws. Spine 36:E1749-1752. https://doi.org/10.1097/BRS.0b013e318221a800
Foley KT, Lefkowitz MA (2002) Advances in minimally invasive spine surgery. Clin Neurosurg 49:499–517
Gepstein R, Shabat S, Reichel M et al (2008) Treatment of postdiscectomy low back pain by percutaneous posterior lumbar interbody fusion versus open posterior lumbar fusion with pedicle screws. Spine J Off J North Am Spine Soc 8:741–746. https://doi.org/10.1016/j.spinee.2007.07.393
Kim D-Y, Lee S-H, Chung SK, Lee H-Y (2005) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine 30:123–129
Laine T, Lund T, Ylikoski M et al (2000) Accuracy of pedicle screw insertion with and without computer assistance: a randomized controlled clinical study in 100 consecutive patients. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 9:235–240
Rajasekaran S, Vidyadhara S, Ramesh P, Shetty AP (2007) Randomized clinical study to compare the accuracy of navigated and nonnavigated thoracic pedicle screws in deformity correction surgeries. Spine 32:E56-64. https://doi.org/10.1097/01.brs.0000252094.64857.ab
Ringel F, Stüer C, Reinke A, Preuss A, Behr M, Auer F, Stoffel M, Meyer B (2012) Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine 37(8):E496-501. https://doi.org/10.1097/BRS.0b013e31824b7767
Knox JB, Dai JM, Orchowski JR (2011) Superior segment facet joint violation and cortical violation after minimally invasive pedicle screw placement. Spine J Off J North Am Spine Soc 11:213–217. https://doi.org/10.1016/j.spinee.2011.01.024
Moshirfar A, Jenis LG, Spector LR et al (2006) Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine 31:2624–2629. https://doi.org/10.1097/01.brs.0000240691.35707.e8
Babu R, Park JG, Mehta AI et al (2012) Comparison of superior-level facet joint violations during open and percutaneous pedicle screw placement. Neurosurgery 71:962–970. https://doi.org/10.1227/NEU.0b013e31826a88c8
Wang L, Wang Y, Yu B et al (2015) Comparison of cranial facet joint violation rate between percutaneous and open pedicle screw placement: a systematic review and meta-analysis. Medicine (Baltimore) 94:e504. https://doi.org/10.1097/MD.0000000000000504
Jones-Quaidoo SM, Djurasovic M, Owens RK, Carreon LY (2013) Superior articulating facet violation: percutaneous versus open techniques. J Neurosurg Spine 18:593–597. https://doi.org/10.3171/2013.3.SPINE12829
Kim CW, Lee Y-P, Taylor W et al (2008) Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. Spine J Off J North Am Spine Soc 8:584–590. https://doi.org/10.1016/j.spinee.2006.12.012
von Jako RA, Carrino JA, Yonemura KS et al (2009) Electromagnetic navigation for percutaneous guide-wire insertion: accuracy and efficiency compared to conventional fluoroscopic guidance. Neuroimage 47(Suppl 2):T127-132. https://doi.org/10.1016/j.neuroimage.2009.05.002
Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, Ploumis A, Xenakis TA (2012) Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 21(2):247–255. https://doi.org/10.1007/s00586-011-2011-3
Yson SC, Sembrano JN, Sanders PC et al (2013) Comparison of cranial facet joint violation rates between open and percutaneous pedicle screw placement using intraoperative 3-D CT (O-arm) computer navigation. Spine 38:E251-258. https://doi.org/10.1097/BRS.0b013e31827ecbf1
Funding
Open access funding provided by Paracelsus Medical University.
Author information
Authors and Affiliations
Contributions
MM identified patients to be included, collected and analyzed data, wrote the manuscript, and interpreted data. RO designed the investigation, analyzed and interpreted data, and reviewed the manuscript. WT identified patients to be included, collected and analyzed data, and reviewed the manuscript. HW interpreted collected data and reviewed the manuscript. MM designed the investigation, analyzed and interpreted data, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors made substantial contributions to the study. The authors confirm that the manuscript, including related data, figures and tables has not been previously published and is not under consideration elsewhere. There has been no financial remuneration. For this retrospective analysis, no ethical committee approval was required. All authors state that the manuscript represents honest work.
Ethics approval
For this retrospective observational study, no ethics committee approval is required by Austrian law. This statement applies to all medical studies without clinical survey regarding pharmaceutical law, medicinal devices act and new medical methods. ("Research projects that are not clinical trials, according to the pharmaceutical act, the medical devices act or new medical methods including non-interventional studies or applied medical research according to the Salzburg Hospital Act are not necessarily to be submitted to the ethics committee of Salzburg for assessment."). Ethics committee Salzburg (Ethikkommission, Land Salzburg) https://www.salzburg.gv.at/gesundheit_/Seiten/ethikkommission.aspx.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mitterer, M., Ortmaier, R., Wiesner, T. et al. Facet joint violation after open and percutaneous posterior instrumentation: a comparative study. Eur Spine J 32, 867–873 (2023). https://doi.org/10.1007/s00586-022-07482-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07482-7