Abstract
Purpose
Astronauts returning from long ISS missions have demonstrated an increased incidence of lumbar disc herniation accompanied by biomechanical and morphological changes associated with spine elongation. This research describes a ground-based study of the effects of an axial compression countermeasure Mk VI SkinSuit designed to reload the spine and reduce these changes before return to terrestrial gravity.
Methods
Twenty healthy male volunteers aged 21–36 without back pain participated. Each lay overnight on a Hyper Buoyancy Flotation (HBF) bed for 12 h on two occasions 6 weeks apart. On the second occasion participants donned a Mk VI SkinSuit designed to axially load the spine at 0.2 Gz during the last 4 h of flotation. Immediately after each exposure, participants received recumbent MRI and flexion–extension quantitative fluoroscopy scans of their lumbar spines, measuring differences between spine geometry and intervertebral kinematics with and without the SkinSuit. This was followed by the same procedure whilst weight bearing. Paired comparisons were performed for all measurements.
Results
Following Mk VI SkinSuit use, participants evidenced more flexion RoM at L3–4 (p = 0.01) and L4–5 (p = 0.003), more translation at L3–4 (p = 0.02), lower dynamic disc height at L5–S1 (p = 0.002), lower lumbar spine length (p = 0.01) and greater lordosis (p = 0.0001) than without the Mk VI SkinSuit. Disc cross-sectional area and volume were not significantly affected.
Conclusion
The MkVI SkinSuit restores lumbar mobility and lordosis following 4 h of wearing during hyper buoyancy flotation in a healthy control population and may be an effective countermeasure for post space flight lumbar disc herniation.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
It is becoming increasingly well-established that an abnormally high proportion of astronauts returning from long duration space missions suffer from lumbar intervertebral disc (IVD) hernias post flight on return to terrestrial gravity [1,2,3]. Furthermore, these pathologies appear to be associated with decreased flexion–extension ranges of motion (RoM) in the upper lumbar motion segments [3]. Whilst the pathophysiology is unknown, these findings point to the need to develop countermeasures to promote long term spinal health [4].
It is known that prolonged periods of spinal unloading both in microgravity (µg) and using long term bed rest analogues on Earth can alter lumbar spine parameters [5, 6]. These include atrophy of the paraspinal muscles, increased muscular fat infiltration and altered protein content of the discs—including decreased glycosaminoglycan and proteoglycan content in both human and animal models [2, 7,8,9,10,11].
Changes in IVD geometry have also been inferred, with disc swelling being assumed due to increases in stature being recorded in-flight [12,13,14]. However, IVD swelling has never been observed in-flight. Lumbar IVD swelling has, however, been observed in response to 3-day dry immersion, with + 11 ± 9% increases in disc volume at L5–S1 and between + 7.5 and + 10.7% at L4/L5 [9, 15]. Thus, it has been proposed that prolonged periods of unloading on the spine during spaceflight can lead to IVD swelling, stretching the posterior annulus fibres and increasing susceptibility to posterior herniation [1, 5, 6, 16].
However, more recent post-flight research has found little evidence of changes in disc hydration, or its association with the incidence of hernias, although this could be a consequence of the washout of the effects of re-entering terrestrial gravity before assessments can be made [3, 6, 17]. Instead, recent studies of NASA astronauts following long duration spaceflight have reported decreased upper lumbar intervertebral ranges of motion (IV-RoM) and muscle trunk atrophy [2, 3, 18]. However, the cause of these changes, their mechanisms and how they may relate to a potentially increased risk of herniation remains unknown. Furthermore, changes in other key kinematic and geometric parameters such as intervertebral laxity, motion sharing inequality, IVD volume, height and cross-sectional area have yet to be investigated.
Immediate complex post-flight testing is challenging, but may be aided if measurements could be performed before the application of upright loading [3, 19]. Furthermore, without knowledge of the underlying pathophysiology, determination and/or development of candidate countermeasures is difficult. However, artificial gravity via short-arm centrifugation [20], and more recently exercise during centrifugation [21] in addition to donning axial loading garments such as SkinSuits [22, 23] have been suggested to promote spinal control [24] whilst exercises performed in the ISS [25,26,27] and sometimes incorporating an axial compression harness [25] may generate transient loading [4]. Of these, axial loading SkinSuits appear to be the most easily implementable for ISS missions and beyond [28] where operational constraints will be more severe [29].
Previous Mk VI SkinSuit studies, with approximately 0.13 Gz of axial loading, have reported an attenuation of stature, with some evidence of compressive effect on the lumbar spine (decreased length, IVD height reduction) compared to 8-h hyper buoyancy flotation (HBF) [30]. However, the effect of the MK VI Skinsuit on lumbar geometry and restraint (i.e. laxity and IV-ROM) are not known. Therefore, our hypothesis was that 4-h SkinSuit reloading in healthy subjects will attenuate the effects of unloading, induced by 12 h HBF, on spinal geometry and kinematics when measured using MRI and quantitative fluoroscopy (QF). The aims of this study were therefore to:
-
1.
Investigate the effect of 4-h axial reloading upon markers of disc swelling in the lumbar spine, induced by the Mk VI SkinSuit.
-
2.
Determine if reloading acts to increase intervertebral motion by comparing parameters of intervertebral restraint between loading conditions
-
3.
Investigate and contrast results derived from non-weight bearing and weight bearing imaging
Methods
In 2016, a ground-based study of the Mk VI SkinSuit as a spinal health countermeasure imparting ~ 0.2 gz of axial loading [22] was commissioned by the European Space Agency (ESA-HRE-OM-MPR-SOW-0001). The research used quantitative fluoroscopy (QF) and upright MRI to investigate the effects of Mk VI SkinSuit reloading performed immediately following a 4-h period of spinal unloading and using a set of lumbar spine geometric and intervertebral kinematic measures (Fig. 1). The study employed both recumbent and weight bearing QF and MRI assessments immediately following unloading, with and without SkinSuit reloading, and with no interim period of weight bearing before testing as a Control condition. The research utilised a Hyper Buoyancy Flotation device (HBF) to unload the spine which has been shown to induce 1.7–2.1 cm of stature elongation after 8 h’ application. This was found to be reduced by 20% after 8 h of wearing an earlier version of the Mk IIV SkinSuit [30]. It was used to compare the same outcome measures in the same individuals after the same period of HBF as a Control, but on a different occasion and with the application of the Mk VI SkinSuit in a short exposure of 4 h following 8 h of HBF.
Participants
Ethical approval for the study was obtained from the National Research Ethics Service (REC Reference 10/H0101/65). Participants were recruited from the student body of our university through poster and email announcements, however, only male participants were recruited to the present study owing to the practical constraints of lying on the HBF. All were required to be healthy and aged between 18 and 50 years and have had no back pain that limited their daily activities in the year prior to participating. All received information sheets about the study and those who expressed a desire to participate gave their written informed consent.
Data collection protocol
Twenty-two male volunteers entered the study. Each was measured and fitted for a Mk VI SkinSuit (Dainese—London) which incorporated a reinforced yoke (chest and shoulder) connected to an elastic fabric (Elasto 2000) that ran from below the yoke line to the ankles (Fig. 2). Elastic ribbons were sewn into the elastic fabric at 2 cm intervals (yoke to ankle) to indicate and distribute material tension with adjustable stirrups attached to the ankles of the suit to initiate the tension once tightened. Each participant attended the Imaging Centre on two occasions in the evening at least 6 weeks apart—one of which required donning the SkinSuit. Participants wore night attire and at 9 pm, entered the HBF room supervised by a research assistant, and lay on the HBF bed for 8 h only broken by a small (15 min) comfort break—where possible, incorporating the donning of the SkinSuit after 8 h in the Test group (Fig. 3). Stature measurements were recorded before and after 8 h overnight HBF (in addition to the 15-min break), using a commercially available stadiometer (SECA, UK). The SkinSuit was then tightened using a previously established protocol to provide axial loading at the foot, with the amount of force produced from each suit measured in this tightened position (ForceShoes, Xsens, Netherlands). Participants then lay on the HBF waterbed device for a further 4 h, after which, if the SkinSuit was used in the session, its ankle straps were released. Urine bottles were supplied so that additional comfort breaks would not require weight bearing.
Imaging protocol
Supine magnetic resonance imaging (MRI)
After 12 h of HBF, all participants were transported directly to the Imaging Centre lying supine on a trolly for recumbent imaging. This began in the MRI room, where they received 11 supine sagittal and axial T2-weighted lumbar spine scans (L1–S1) (5 mm slice thickness, 2597/1117 ms repetition/echo with a 30 cm field of view) parallel to the spine on coronal localisers and 20 (4 blocks of 5 slices) axial slices (4 mm thickness, 5368/132 ms repetition/echo time, 25 cm field of view) aligned through each IVD from L1–S1 to facilitate IVD height and cross-sectional area measurement (Paramed ASG MROpen, 0.5T, Genoa, Italy).
Lateral recumbent quantitative fluoroscopy (QF)
After the supine MRI, participants were transported whilst remaining supine to the X-ray room by trolley where they were positioned on their left side on a motorised table with a horizontal motion frame, such that the lower section swung their upper body through a controlled rate and range of flexion and extension (Atlas Clinical Ltd., Lichfield, UK). Fluoroscopic images acquired at 15 Hz were obtained in this passive recumbent configuration [31], first in 40° of flexion, followed by 40° of extension. A Siemens Arcadis Avantic VC10A digital fluoroscope, (Henkestrasse, Germany) with a 13″ field of view, was used and image acquisition was synchronised with the controller of the horizontal motion frame. The motion occurred over a period of approximately 20 s at 6°/s2 for the first second of motion, followed by 6°/s1. The central ray was positioned at L3-4 disc with all vertebrae from L2–S1 in the field of view during continuous imaging.
Upright (seated) magnetic resonance imaging (MRI)
After the first QF, participants were allowed to stand, and when steady, to walk to the adjacent MRI room where they received sitting scans using a similar protocol to the first MRI session (Fig. 4).
Upright (standing) Quantitative Fluoroscopy (QF)
Following the second MRI, participants walked back to the QF room where they received standing fluoroscopic imaging while stabilised against an upright controller. This guided them by 60° of flexion and 20° of extension in separate sequences synchronised to the fluoroscopic imaging.
Data analysis
All data were anonymised with the author blinded through random number assignment to scans prior to analysis. Images were checked by a consultant radiologist for underlying pathology. Normality was assessed by visual check of histograms and whether the skewness and kurtosis ratio lay below or above 1.96/−1.96 [32]. Data were compared between SkinSuit/non-SkinSuit (Control) exposure and expressed as either means ± 95%CI (stature and MRI measurements) or mean difference ± SkinSuit loading and its significance (p) (subjective ratings and QF measurements—2-sided Wilcoxon test). Effect sizes were calculated by Cohen’s D. and analysis was performed using SPSS v26.0 (SPSS IBM, Chicago, Ill, USA).
Image analysis
MRI scans were inspected for abnormalities by a consultant radiologist and analysed using the RadiAnt Dicom Viewer V1.19 (Medixant, Poznan, Poland). Lumbar spinal length was determined using the distance between the posterior superior corner of the L1 and S1 endplates. Cobb’s method evaluated lumbar curvature through the angle formed between tangent lines drawn from the L1 and S1 superior endplates. Anterior, middle, posterior and average IVD height was determined using a modified Dabb’s method—averaging the distance between the anterior, middle and posterior IVD from L1/L2 to L5/S1 [33]. IVD volume was calculated by multiplying the average height as measured above, with the average of the cross-sectional area taken by drawing the IVD area from the three axial slices through the midline of the IVD (OsiriX Lite, Pixmeo Sarl, Switzerland).
QF image processing and analysis were performed using custom code written in MATLAB (V7.12, The Mathworks, Cambridge, UK) [34]. For the fluoroscopic images, each of the vertebral corners were marked five separate times and processed to determine their movement during the dynamic sequence and averaged. The inter-vertebral motion parameters measured were; maximum IV-RoM, dynamic anterior disc height, maximum translation, laxity, motion sharing inequality (MSI) and motion sharing variability (MSV), all of which have been found to have good intra observer reliability [35,36,37,38].
Results
Sample size
Intervertebral range of motion (IV-RoM) was chosen as the primary outcome variable and an initial pilot study of 8 volunteers was conducted to test the working methods. This found the mean (SD) difference in flexion IV-RoM at L4–5 between unloaded and SkinSuit reloaded states to be 0.8° (1.02). Assuming a nonparametric comparison, the sample size required to detect this difference with 80% power at the 95% level of probability was determined to be 14. It was, therefore, decided to attempt to recruit an additional 13 participants to provide a total of 21, anticipating a loss to follow up of up to 1/3 of them.
Study population
Twenty-two males were recruited to the study. Two withdrew before the second imaging session, both due to unrelated health problems, leaving twenty participants (mean age 25.5, range 21–36, mean BMI 23.7, range 19–29) who completed all parts of the study. No adverse effects were reported, and all participants reported feeling comfortable in the SkinSuit. Inspection of the MRI images by a radiologist found transitional lumbo-sacral segments in two participants and L4–5 disc degeneration in one other. Participants received an average effective radiation dose of 0.74 mSv (upper quartile 0.81) from each of the two QF studies, which compares with 1.3 mSv for one X-ray examination of the lumbar spine in the NHS [39].
All participants comfortably slept on the HBF overnight and could don the SkinSuit without difficulty.
Standing stature
Standing stature was significantly (p < 0.0001) increased after overnight (8-h) sleep on HBF in both sessions (20.6 ± 3.7 mm). Preceding the 15-min break and before donning the SkinSuit, stature had reduced by 6.2 ± 3 mm (p < 0.0001); a 30% attenuation of stature gain. These increments were further reduced by 3.4 ± 6.5 mm upon donning the SkinSuit, which in total resulted in a 50% drop in the unloaded stature gain at the start of SkinSuit reloading period vs. 30% without.
Lumbar geometry (MRI)
The results of an intraobserver reliability study of MRI measurements were: disc height (ICC 0.95), lumbar spine length (ICC 0.99) and lumbar lordosis (ICC 0.98). After SkinSuit reloading, lumbar length was significantly reduced (1.4 mm) compared to no SkinSuit use but only when measured in the supine position (p = 0.014). Lordosis increased by 4.6 mm when measured in the seated position only (p = 0.0001) (Table 1). Disc cross-sectional area generally increased and height decreased after SkinSuit reloading as measured by both supine and seated MRI, although this did not reach significance at any level (Supplementary Table 1). Disc volume differences were inconsistent, and never significant, while disc cross-sectional area and volume could not always be accessed at L1–2 due to the limited MRI image field. Overall, this suggests that spine length is slightly reduced, with very minor indications of disc swelling reduction after SkinSuit reloading during HBF. However, SkinSuit use was also associated with a considerable increase in lordosis when measured seated (Table 1).
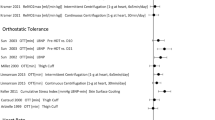
Lumbar kinematics (QF)
The reliability of kinematic measurements in the lumbar spine by QF has been reported to be high in previous studies [38, 40,41,42]. Supplementary Table 2 (a, b) shows the L2–S1 dynamic intervertebral responses after SkinSuit reloading during HBF measured both in the lateral decubitus and standing positions for both flexion and extension. Most of the significant differences with and without SkinSuit donning were found during recumbent flexion, where IV-RoM increased by 0.7° at L3-4 (p = 0.01) (ES = 0.64) and flexion translation by 0.9 mm (p = 0.02) (ES 0.59). At L4-5 during recumbent flexion, IV-RoM was also 0.9° greater (p = 0.003) (ES 0.79) with SkinSuit use. From a previous study, the intrasubject reliability (ICC) for this over 6 weeks was 0.95 [43]. Large effects were also found for the decrease in dynamic minimum anterior disc height at L5–S1 (1.0 mm) during recumbent flexion following SkinSuit reloading in HBF (p = 0.002) (ES = 0.80). No significant effects were observed for weight bearing (standing) intervertebral kinematics, apart from a small effect (ES = 0.20) from an increase in the laxity gradient of 0.11 at L5–S1 (p = 0.02) during weight bearing extension following SkinSuit reloading. In addition, a moderate effect (ES = 0.50) was found in the form of a 21% increase in motion sharing inequality (MSI) among the segments from L2–S1 during recumbent extension following SkinSuit use (p = 0.04). This could be considered a result of unevenly distributed additional mobility at some segments. Motion sharing variability (MSV) was however, unaffected.
These results suggest that 4 h of SkinSuit reloading following rest in HBF is associated with increased lumbar mobility in the mid-lumbar spine, close to where reduced motion has been observed to be associated with disc herniation after long periods on the ISS [3]. Dynamic anterior disc height reduction at L5–S1 was also found following SkinSuit use during recumbent flexion measured by QF but not on static disc height measurement on MRI.
Discussion
The recent association of post-flight disc herniation with abnormal kinematics and spinal geometry has awakened interest in countermeasures to address the effects of unloading and reloading the spine during space missions [3, 44, 45]. The present study explored the potential of ~ 0.2Gz imparted by the Mk VI SkinSuit to restore normal biomechanics in the lumbar spine modulated by being unloaded by a novel ground-based analogue with no SkinSuit. This approach is based on the assumption that (1) the association between upper lumbar stiffness and disc herniation is somehow causative, and (2) restoring normal biomechanics before applying terrestrial gravity could reduce herniation risk. Although intuitive, these assumptions also coexist with the fact that back pain in spaceflight is more prevalent in astronauts who have suffered from it previously [15] and that there are other risk factors for disc hernia that are unseen—for example, the presence of undetected annulus defects as initiation sites for herniation [15, 46, 47].
Our results found a considerable increase in lumbar lordosis with Mk VI SkinSuit use suggesting that the spine elongation reported in other studies may largely be due to loss of lordosis, which appears to be mitigated by SkinSuit use and therefore presumably accounts for most of the majority of stature reductions [12, 13]. This also has implications for lumbar kinematics, as our previous work found increased lordosis in healthy controls to be associated with a higher weightbearing flexion IV-RoM at L2–3 (r = 0.54) and lower at L4–5 (r = − 0.52) [35].
Bailey et al. [3] reported that pre-flight translation at L3–4 was lower in astronauts who experienced postflight disc herniation, with a decrease in translation over the upper three lumbar levels. This can be seen against an increased L3–4 flexion translation and increased L3–5 IV-RoM in the present study following SkinSuit use compared to no SkinSuit. Increased motion was also observed at L2–3 but this did not reach statistical significance (Supplementary Table 2a, Fig. 5a, b.
Our results therefore support the hypothesis that 4 h of SkinSuit reloading attenuates some of the effects of HBF unloading on lumbar geometry and kinematics. These influences are more in line with kinematic changes than disc swelling (aim 1) and were generally only significant when measured before any interim period of weight bearing before testing. Specifically, supine MRI scans showed that lumbar length, lordosis, disc height, disc cross-sectional area and disc volume all exhibited changes consistent with the hypothesis that SkinSuit reloading adds compression upon the lumbar spine. Three of these (lumbar length, disc height and disc volume) were significantly different in the expected directions and two (lordosis and disc cross-sectional area) showed trends (p < 0.20). Lateral recumbent QF kinematic assessments exhibited significantly increased IV-RoM and decreased minimum dynamic disc height during flexion following SkinSuit use (aim 2). Disc height change and Motion Sharing Inequality (MSI) also became significantly greater in extension.
Only two morphologic variables and no biomechanical variables were found to have changed when measured during weight bearing imaging examinations. The difference in these results of the two test orientations may be explained by the tendency of compressive loading during the weight bearing tests to wash out the SkinSuit reloading effects (aim 3). Similarly, the increases in stature observed after µg exposure may be related more to reduction in lumbar lordosis than to disc swelling. This seems to suggest that future astronaut imaging protocols to understand in-flight biomechanical changes and countermeasure effectiveness are probably less worthwhile once a period of post-flight weight bearing has occurred.
The Mk VI SkinSuit has been shown to be compatible with wear during rest and unloading for periods sufficiently long to generate potentially significant reloading effects without the need to perform concurrent physical exercises. The MK VI SkinSuit is a relatively unobtrusive garment which appears comfortable for participants to wear for at least 8 h. However, consideration should be given to the practicality of longer periods of SkinSuit wear, and to what an optimal protocol may comprise of in the last few days prior to return to Earth, or other gravitational environment.
While the present study may support further definition of µg spinal countermeasures, it does not explain the possible relationship between SkinSuit use and protection from hernias. Recent studies have found no consistent post-flight changes in disc hydration, or any association between these and the incidence of disc herniation, casting doubt on the previously assumed role of disc swelling in post-flight herniation [3].
Future work
The present study found little effect of short-term SkinSuit use on disc volume, despite increases in mid-lumbar IV-RoM, whose reduction during space flight seems to be associated with hernias [3], although volume reduction from loading after bedrest occurs only slowly [19]. Therefore, it may be useful to explore the possible association between reduced IV-RoM and other structural phenomena, such as posterior annular-endplate junction defects [47]. Future studies should also seek to include female participants.
Conclusion
The MkVI SkinSuit restores lumbar mobility and lordosis following 4 h of wearing during HBF in a healthy control population and may be an effective countermeasure for post flight lumbar disc herniation.
References
Johnston SL, Campbell MR, Scheuring R, Feiveson AH (2010) Risk of hernated nucleus pulposus among US astronauts. Aviat Space Environ Med 81:566–574
Chang D, Sayson JV, Chiang S, Riascos-Castaneda R, Walker K, Lotz JC, Hargens AR (2014) Risk of intervertebral disc damage after prolonged space flight. Br J Sports Med 48:578–579
Bailey JF, Nyayapati P, Johnson GTA, Dziesinski L, Scheffler AW, Crawford R, Scheuring R, O’Neill CW, Chang D, Hargens AR, Lotz JC (2022) Biomechanical changes in the lumbar spine following spaceflight and factors associated with postspaceflight disc herniation. Spine J 2:197–206. https://doi.org/10.1016/j.spinee.2021.07.021
Green DA, Scott JPR (2018) Spinal health during unloading and reloading associated with spaceflight. Front Physiol 8:1186. https://doi.org/10.3389/fphys.2017.01126
Belavy DL, Adams M, Brisby H, Cagnie B, Danneels L, Fairbank J, Hargens AR, Judex S, Scheuring RA, Sovelius R, Urban J, van Dieen JH, Wilke H-J (2016) Disc herniations in astronauts: what causes them, and what does it tell us about herniation on earth? Eur Spine J 25:144–154. https://doi.org/10.1007/s00586-015-3917-y
Chang DG, Healey RM, Snyder AJ, Sayson JV, Macias BR, Coughlin DG, Bailey JF, Parazynski SE, Lotz JC, Hargens AR (2016) Lumbar spine paraspinal muscle and interverteral disc height changes in astronauts after long-duration spaceflight on the international space station. Spine 41:1917–1924
Yasuoka H, Asazuma T, Nakanishi K, Yoshihara Y, Sugihara A, Omiya M, Okabayashi T, Nemota K (2007) Effects of reloading after simulated microgravity on proteoglycan metabolism in the ncleus pulposus and anulus fibrosus of the lumbar intervertebral disc: an experimental study using a rat tail suspension model. Spine 32:734–740
Jin L, Feng G, Reames DL, Shimer AL, Shen FH, Li X (2013) The effects of simulated microgravity on intervertebral disc degeneration. Spine J 13:235–242
Kordi M, Belavy DL, Armbrecht G, Sheikh A, Felsenberg D, Trudel G (2015) Loss and re-adaptation of lumbar intervertebral disc water signal intensity after prononged bedrest. J Musculoskelet Neuronal Interact 15:294–300
Hides JA, Lambrecht G, Santon WR, Daman V (2016) Changes in multifidus and abdominal muscle size in response to microgravity: possible implications for low back pain research. Eur Spine J 25:808–818
Kalichman I, Caarneli E, Been E (2017) The association between imaging parameters of the paraspinal muscles, spinal degeneration and low back pain. Biomed Res Int 2017:1–14
Thorton W, Moore T (1987) NASA-TM-58280: height changes in microgravity. In: Bungo M, Bagain T, Bowman M, Levitan B (eds) Results of the life sciences DSOs conducted aboard the space Chuttle 1981–1988. Houston TX
McGill S, Axler CT (1996) Changes in spine height throughout 32 hours of bedrest. Arch Phys Med Rehab 77:1071–1073
Sudhakar R, Young K, Reid C, Dirlich T (2015) Quantification of inflight physical changes: anthropometry and neutral body posture (body measures). In. JSC-CN-32660
Treffel L, Mkhitaryan K, Gellee S, Gauquelin-Koch G, Gharib C, Blanc S, Millet C (2016) Intervertebral disc swelling demonstrated by 3D and water content magnetic resonance analyses after a 3-day dry immersion simulating microgravity. Front Physiol. https://doi.org/10.3389/fphys.2016.00605
Sibonga J, Holguin N, Johnston S, Judex S, Scheuring, R. (2008) HRP-47060: Risk of Intervertebral Disc Damage (Report). Human Research Program: Human Health Countermeasures Element. Evidence Book. National Aeronautics and Space Administration, Lyndon B Johnson Space Centre, Houston, Texas. https://humanresearchroadmap.nasa.gov/evidence/reports/IVD.pdf
Bailey JF, Miller SL, Khieub K, O’Neill KW, Healey RM, Coughlin DG, Sayson JV, Chang DG, Hargens AR, Lotz JC (2018) From the international space station to the clinic: how prolonged unloading may disrupt lumbar spine stability. Spine J 18:7–14. https://doi.org/10.1016/j.spinee.2017.08.261
Sayson JV, Lotz JC, Parazynski SE, Chang DG, Healey RM, Hargens AR (2015) Microgravity-induced back pain and interverteral disc herniation: international space station results. In: 66th international astronautical congress. Jerusalem, Israel October 2015
Hutton WC, Malko JA, Fajman WA (2003) Lumbar disc volume measured by MRI: effects of bed rest, horizontal exercise and vertical loading. Aviat Space Environ Med 74:73–78
Clement G, Paloski WH, Rittweger J, Linnarsson D, Barielle MP, Mulder E, Wuyts FL, Zange J (2016) Centrifugation as a countermeasure during bed rest and dry immersion: What has been learned? J Musculoskeletal Neuronal Interact 16:84–91
Frett T, Lecheler L, Speer M, Marcos D, Pesta D, Tegtbur U, Jordan J, Green DA (2022) Comparison of trunk muscle exercises in supine position during short arm centrifugation with 1g at centre of mass and upright in 1g. Front Physiol. https://doi.org/10.3389/fphys.2022.955312
Carvil P, Attias J, Evetts S, Waldie J, Green DA (2017) The effect of the gravity loading countermeasure skinsuit on movement and strength. J Strength Cond Res 31:154–161. https://doi.org/10.1519/JSC.0000000000001460
Kozlovskaya IB, Yarmanova EN, Yegorov AD, Stepantsov VI, Fomina EV, Tomilovaskaya ES (2015) Countermeasure systems for adverse effects of microgravity on long-duration ISS flights. Aerosp Med Hum Perform 86:A24-31
Rathinam C, Spokes G, Bridges S, Green DA (2013) The effects of dynamic lycra body suit on a child with developmental coordination disorder—a single case study. J Prosthet Orthot 25:58–61
Petersen N, Jaekel P, Rosenberger A, Weber T, Scott J, Castrucci F, Lambrecht G, Ploutz-Snyder L, Damann V, Kozlovskaya I, Mester J (2016) Exercise in space: the European Space Agency approach to in-flight exercise countermeasures for long-duration missions on ISS. Extreme Physiol Med. https://doi.org/10.1186/s13728-016-0050-4
Loehr JA, Guilliams ME, Petersen N, Hirsch N, Kawashima S, Ohshima H (2012) Physical training for long duration spaceflight. Aerosp Med Hum Perform 86:A14-23
Dowzer CN, Reilly T, Cable N (1998) Effects of deep and shallow water running on spinal shrinkage. Br J Sports Med 31:44
Stabler RA, Rosado H, Doyle R, Negus D, Carvil PA, Kristjánsson JG, Green DA, Franco-Cendejas R, Davies C, Mogensen A, Scott J, Taylor P (2017) Impact of the Mk VI SkinSuit on skin microbiota of terrestrial volunteers and an International space station-bound astronaut. Nat Microgravity. https://doi.org/10.1038/s41526-017-0029-5
Waldie JM, Newman DJ (2011) A gravity loading countermeasure skinsuit. Acta Astronaut 68:722–730. https://doi.org/10.1016/j.actaastro.2010.07.022
Carvil P (2017) Axial loading as a countermeasure to microgravity-induced deconditioning: effects on the spine and its associated structures. King’s College London, London
Breen AC, Teyhen DS, Mellor FE, Breen AC, Wong K, Deitz A (2012) Measurement of inter-vertebral motion using quantitative fluoroscopy: Report of an international forum and proposal for use in the assessment of degenerative disc disease in the lumbar spine. Adv Orthop. https://doi.org/10.1155/2012/802350
Fallowfield J, Hale B, Wlkinson D (2005) Using statistics in sport and exercise science research. Lotus Publishing, Chichester
Dabbs VM, Dabbs LG (1990) Correlation between disc height narrowing and low-back pain. Spine 15:1366–1369
van Loon IHM, Mellor FE, Breen A (2012) Accuracy and repeatability of sagittal translation of lumbar vertebrae in vitro and in vivo using quantitative fluoroscopy. Clin Chiropr 15:135–146
du Rose A, Breen A (2016) Relationships between lumbar inter-vertebral motion and lordosis in healthy adult males: a cross sectional cohort study. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-016-0975-1
Breen A (2011) Quantitative fluoroscopy and the mechanics of the lumbar spine. Open University
Breen A, Breen A (2016) Accuracy and repeatability of quantitative fluoroscopy for the measurement of sagittal plane translation and instantaneous axis of rotation in the lumbar spine. Med Eng Phys 38:607–614
To D, Breen Ax, Breen A, Mior S, Howarth SJ (2020) Investigator analytic repeatability of two new intervertebral motion biomarkers for chronic, nonspecific low back pain in a cohort of healthy controls. Chiropr Manual Ther. https://doi.org/10.1186/s12998-020-00350-5
England PH (2008) Patient dose information: guidance. In. Gov.uk, London
Breen A, Muggleton J, Mellor F (2006) An objective spinal motion imaging assessment (OSMIA): reliability, accuracy and exposure data. BMC Musculoskelet Disord 7:1–10
Mellor FE, Thomas P, Thompson P, Breen AC (2014) Proportional lumbar spine inter-vertebral motion patterns: a comparison of patients with chronic non-specific low back pain and healthy controls. Eur Spine J 23:2059–2067. https://doi.org/10.1007/s00586-014-3273-3
Yeager MS, Cook DJ, Cheng BC (2014) Reliability of computer-assisted lumbar intervertebral measurement using a novel vertebral motion analysis system. Spine J 14:274–281
Breen A, Hemming R, Mellor F, Breen A (2019) Intrasubject repeatability of in vivo intervertebral motion parameters using quantitative fluoroscopy. Eur Spine J 28:450–460. https://doi.org/10.1007/s00586-018-5849-9
Laws CJ, Berg-Johansen B, Hargens AR, Lotz JC (2016) The effect of simulated microgravity on lumbar spine biomechanics: an in vitro study. Eur Spine J 25:2889–2897
Nicogossian A, Pool S, Sawin C (1995) Status and efficacy of countermeasure to physiological deconditioning from space flight. Acta Astronaut 36:393–398. https://doi.org/10.1016/0094-5765(95)00123-9
Thompson RE, Pearcy MJ, Barker TM (2004) The mechanical effects of intervertebral disc lesions. Clin Biomech 19:448–455. https://doi.org/10.1016/j.clinbiomech.2004.01.012
Wade K, Berger-Roscher N, Saggese T, Rasche V, Wilke H (2022) How annulus defects can act as initiation sites for herniation. Eur Spine J. https://doi.org/10.1007/s00586-022-07132-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer The views expressed herein can in no way be taken to reflect the official opinion of the ESA.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Breen, A., Carvil, P., Green, D.A. et al. Effects of a microgravity SkinSuit on lumbar geometry and kinematics. Eur Spine J 32, 839–847 (2023). https://doi.org/10.1007/s00586-022-07454-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07454-x