Abstract
Objective
The aim of the study was to compare total en bloc spondylectomy (TES) and separation surgery with postoperative stereotactic radiosurgery (SSRS) for isolated metastatic patients with spinal cord compression by assessing recurrence-free survival (RFS), overall survival (OS), postoperative complications, and quality of life scores (QoL).
Methods
From October 2013 to December 2020, 52 isolated spinal metastasis patients with cord compression were selected and separated into two groups based on the surgical method used (TES group, n = 26; and SSRS group, n = 26). Indexes for evaluation included postoperative Frankel grade, postoperative ECOG-PS, RFS, OS, postoperative complications, operation time, intraoperative blood loss, and QoL.
Results
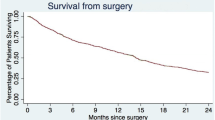
The average follow-up duration was 31.44 months. There was no significant difference (P > 0.05) in postoperative complications and OS between the two groups. However, a significant difference in operation time, intraoperative blood loss, postoperative ECOG-PS, RFS, and mental health domain (6 months after surgery) was found between the two groups (P < 0.05). According to The Spine Oncology Study Group Outcomes Questionnaire assessment, the total pain and physical function domains scores were also elevated after surgery in both groups. However, no significant difference was observed between groups A and B (p = 0.450 and 0.446, respectively).
Conclusions
TES and SSRS were efficient methods for treating solitary spinal metastasis patients with metastatic spinal cord compression. Better local tumor control and mental health were found in the TES group, and most patients felt as if they were free of spinal tumors. Compared with TES, the SSRS caused less operation-related trauma. However, there was no significant difference in OS between the two groups.


Similar content being viewed by others
References
Roodman GD (2004) Mechanisms of bone metastasis. N Engl J Med 350:1655–1664. https://doi.org/10.1056/NEJMra030831
Spratt DE, Beeler WH, de Moraes FY, Rhines LD, Gemmete JJ, Chaudhary N, Shultz DB, Smith SR, Berlin A, Dahele M, Slotman BJ, Younge KC, Bilsky M, Park P, Szerlip NJ (2017) An integrated multidisciplinary algorithm for the management of spinal metastases: an international spine oncology consortium report. Lancet Oncol 18:e720–e730. https://doi.org/10.1016/s1470-2045(17)30612-5
Cao S, Gao X, Bai G, Xin B, Wang T, Cao J, Lv K, Zhu C, Ni X, Zou W, Zhou Y, Xiao J, Liu T (2021) Development and validation of a scoring system for differential diagnosis of tuberculosis and metastatic tumor in the spine. Infect Drug Resist 14:407–413. https://doi.org/10.2147/IDR.S298316
Yao KC, Boriani S, Gokaslan ZL, Sundaresan N (2003) En bloc spondylectomy for spinal metastases: a review of techniques. Neurosurg Focus 15:1–6
Gao X, Wu Z, Wang T, Cao J, Bai G, Xin B, Cao S, Jia Q, Liu T, Xiao J (2021) A discussion on the criteria for surgical decision-making in elderly patients with metastatic spinal cord compression. Global Spine J. https://doi.org/10.1177/2192568221991107
Laufer I, Iorgulescu JB, Chapman T, Lis E, Shi W, Zhang Z, Cox BW, Yamada Y, Bilsky MH (2013) Local disease control for spinal metastases following “separation surgery” and adjuvant hypofractionated or high-dose single-fraction stereotactic radiosurgery: outcome analysis in 186 patients. J Neurosurg Spine 18:207–214
Kato S, Murakami H, Demura S, Yoshioka K, Kawahara N, Tomita K, Tsuchiya H (2014) More than 10-year follow-up after total en bloc spondylectomy for spinal tumors. Ann Surg Oncol 21:1330–1336. https://doi.org/10.1245/s10434-013-3333-7
Moussazadeh N, Laufer I, Yamada Y, Bilsky MH (2014) Separation surgery for spinal metastases: effect of spinal radiosurgery on surgical treatment goals. Cancer Control J Moffitt Cancer Cent 21:168
Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T (2001) Surgical strategy for spinal metastases. Spine 27:298–306
Versteeg AL, Sahgal A, Rhines LD, Sciubba DM, Schuster JM, Weber MH, Varga PP, Boriani S, Bettegowda C, Fehlings MG, Clarke MJ, Arnold PM, Gokaslan ZL, Fisher CG, Tumor AOKF (2018) Psychometric evaluation and adaptation of the Spine Oncology Study Group Outcomes Questionnaire to evaluate health-related quality of life in patients with spinal metastases. Cancer 124:1828–1838. https://doi.org/10.1002/cncr.31240
Barzilai O, Versteeg AL, Goodwin CR, Sahgal A, Rhines LD, Sciubba DM, Schuster JM, Weber MH, Lazary A, Fehlings MG, Clarke MJ, Arnold PM, Boriani S, Bettegowda C, Gokaslan ZL, Fisher CG, Laufer I, Tumor AOKF (2019) Association of neurologic deficits with surgical outcomes and health-related quality of life after treatment for metastatic epidural spinal cord compression. Cancer 125:4224–4231. https://doi.org/10.1002/cncr.32420
Gao X, Zhang K, Cao S, Hou S, Wang T, Guo W, Wu Z, Jia Q, Liu T, Xiao J (2020) Surgical treatment of spinal cord compression caused by metastatic small cell lung cancer: 10 years of experience in a single center. Cancer Manag Res 12:3571–3578. https://doi.org/10.2147/CMAR.S250422
Abe E, Kobayashi T, Murai H, Suzuki T, Chiba M, Okuyama K (2001) Total spondylectomy for primary malignant, aggressive benign, and solitary metastatic bone tumors of the thoracolumbar Spine. J Spinal Disord 14:237–246
Sundaresan N, Rothman A, Manhart K, Kelliher K (2002) Surgery for solitary metastases of the Spine: rationale and results of treatment. Spine 27:1802–1806
Yamada Y, Katsoulakis E, Laufer I, Lovelock M, Barzilai O, Mclaughlin LA, Zhang Z, Schmitt AM, Higginson DS, Lis E (2017) The impact of histology and delivered dose on local control of spinal metastases treated with stereotactic radiosurgery. Neurosurg Focus 42:E6
Palma DA, Olson R, Harrow S et al (2020) Stereotactic Ablative Radiotherapy for the Comprehensive Treatment of Oligometastatic Cancers: Long-Term Results of the SABR-COMET Phase II Randomized Trial. J Clin Oncol 38(25):2830–2838. https://doi.org/10.1200/JCO.20.00818
Zelefsky MJ, Yamada Y, Greco C et al (2021) Phase 3 Multi-Center, Prospective, Randomized Trial Comparing Single-Dose 24 Gy Radiation Therapy to a 3-Fraction SBRT Regimen in the Treatment of Oligometastatic Cancer. Int J Radiat Oncol Biol Phys 110(3):672–679. https://doi.org/10.1016/j.ijrobp.2021.01.004
Wise JJ, Fischgrund JS, Herkowitz HN, Montgomery D, Kurz LT (1999) Complication, survival rates, and risk factors of surgery for metastatic disease of the Spine. Spine 24:1943–1951
Cao S, Li L, Du Y, Gan J, Wang J, Wang T, Liu Y, Liu W, Zhou Y, Gao X, Li H, Liu T (2021) Porous gelatin microspheres for controlled drug delivery with high hemostatic efficacy. Colloids Surf B 207:112013. https://doi.org/10.1016/j.colsurfb.2021.112013
Arrigo RT, Kalanithi P, Cheng I, Alamin T, Carragee EJ, Mindea SA, Park J, Boakye M (2011) Predictors of survival after surgical treatment of spinal metastasis. Neurosurgery 68:674–681. https://doi.org/10.1227/NEU.0b013e318207780c
Gao X, Zhao C, He S, Fan T, Xu W, Yang C, Liu T, Xiao J (2018) Treatment and outcomes of 28 patients with spinal metastasis from gynecological cancer. J Neurooncol 137:387–394. https://doi.org/10.1007/s11060-017-2728-x
Funding
This work was supported by the National Natural Science Foundation of China (81972506).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cao, S., Gao, X., Zhang, Y. et al. A comparison of two different surgical procedures in the treatment of isolated spinal metastasis patients with metastatic spinal cord compression: a case–control study. Eur Spine J 31, 1583–1589 (2022). https://doi.org/10.1007/s00586-021-07032-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-07032-7