Abstract
Purpose
To summarize the recommendations from the national clinical guideline published by the Danish Health Authority, regarding cemental augmentation as treatment for painful vertebral lesions, in patients with malignant disease.
Methods
A multidisciplinary working group formulated recommendations based on the GRADE approach.
Results
Two of the questions were based on randomized studies and one on professional consensus. The guideline recommends cemental augmentation for painful vertebral lesions in patients with malignant diagnosis, either hematological or non-hematological. Fracture of the posterior wall is not a contradiction to cemental augmentation, but care should always be taken while injecting the cement, to decrease the risk of cemental leaks into the spinal canal.
Conclusion
The recommendations are based on low-to-moderate quality of evidence or professional consensus as well as patient preferences and positive and harmful effects of the intervention. The working group recommends more randomized studies on patients with different malignant diseases and painful vertebral lesions comparing percutaneous vertebroplasty/kyphoplasty and conservative treatment to confirm the conclusion in this guideline.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction/background
Since 2012, the Danish Health Authority (DHA) has been publishing national clinical guidelines on different health areas to support the evidence-based decision making. Guidelines on healthcare areas with high burden of disease, and challenging interdisciplinary and intersectorial cooperation, have the highest priority. More than 70 guidelines have been published so far, supporting uniform and high-quality treatment across Denmark.
Recently a national clinical guideline on the treatment with vertebral augmentation, including percutaneous vertebroplasty (PVP) and kyphoplasty (KP), of painful vertebral lesions on the basis of malignant disease has been published (https://drks.ortopaedi.dk/nkr-for-perkutan-vertebroplastik-til-palliativ-behandling-af-maligne-sammenfald-i-ryggen/).
Percutaneous vertebroplasty has been developed in the 1980s and is a minimally invasive treatment for painful vertebral lesions [1]. Under fluoroscopy, a Jamshidi needle is inserted in the vertebral body through a transpedicular approach. Polymethylmethacrylate is injected into the vertebral body under imaging guidance. Kyphoplasty differs from vertebroplasty as the height of the fractured vertebra is restored with a balloon catheter prior to injection of bone cement. Both procedures can be performed under local anesthesia, and the patients do not need to be hospitalized for more than one day [2].
The first lesion treated using percutaneous vertebroplasty was a hemangioma. Later osteoporotic fractures became the most frequent indication, but patients with vertebral lesions caused by malignant disease are suitable for the procedure as well.
In Denmark, there is an incidence of approximately 37,000 new cancer diagnoses annually. Between 5 and 10% of these patients will experience metastasis to the spine [3]. Treatment of the cancer occasionally results in development of osteoporosis, with the risk of vertebral fractures. Some of these patients have advanced cancer, and the treatment of pain is essential in order to improve quality of life (Table 1).
The treatment of painful vertebral lesions in patients with malignant disease varies in different parts of Denmark. In some regions, PVP is offered, and in other regions, the practice of PVP is not well established and practitioners are not aware of the treatment.
There was a need for a review of the literature to make an evidence-based guideline on the topic, in order to offer patients with malignant diagnosis and painful vertebral lesions a uniform and evidence-based treatment across the different regions of Denmark.
Material and methods
Study design
The Danish national guidelines are based on the Grades of Recommendation Assessment, Development, and Evaluation (GRADE) approach [4]. In other words, this guideline is based on a critical systematic review of the literature followed by meta-analysis of the evidence. The recommendations are made on the basis of the evidence combined with an evaluation of possible patient preferences and potential risks and harms of the vertebral augmentation procedure in this vulnerable patient population.
Description of work process
A multidisciplinary work group was assembled. A search specialist from a university library and a methodologist previously employed at the DHA were a part of the group to ensure the GRADE approach. A lead reviewer was appointed by the DHA to coordinate the work and draft the report.
The other work group members were appointed by invitation from relevant professional organizations and scientific associations. The working group was composed of an oncologist, a radiologist, two spine surgeons (an orthopedic surgeon and a neurosurgeon), an anesthesiologist, an orthopedic surgeon, a hematologist, a general practitioner, a nurse with specialty in palliative care, and a specialist in palliative medicine.
The work process consisted of formulating three research questions (PICO questions) for evaluating, searching for the literature, grading the evidence, and formulating the recommendations.
The work was approved by a reference group with representatives from the Danish healthcare system, patient organizations, and a patient, who gave advice in formulating the research questions.
Research questions (PICO questions)
Population
This study was restricted to patients with malignant disease with painful low-energy fracture of one or more vertebral bodies. Patients with neurological signs or infection were excluded. Patients with spinal instability and the need for surgical intervention other than vertebral augmentation were excluded as well. In PICO 1, patients with malignant disease other than hematologic disease were included. In PICO 2, only patients with hematologic disease were included. In PICO 3, there was no distinction between different malignant diseases, but only patients with fractures involving the posterior wall of the vertebral body were included.
Intervention
The intervention was vertebral augmentation, including percutaneous vertebroplasty or kyphoplasty. Both treatments are pain-relieving procedures for painful vertebral lesions. Kyphoplasty is not used routinely in Denmark, but is included in this guideline in order to avoid missing important studies in the literature review. The concept vertebral augmentation is covering both procedures.
Comparison
The comparison included physiotherapy, bed rest, analgesics, bracing, and other non-surgical procedures.
Outcome
Outcome measures were determined for each research question. In PICO 1 and PICO 2, pain was determined to be the primary outcome measure. In PICO 3, complications because of cemental leak to the spinal canal or the foraminae were the primary outcome. Other outcome measures comprised of quality of life, mobility, the need for pain medication, new vertebral fractures, symptomatic complications (e.g., cemental leaks, infection, fracture of pedicle, hemothorax, lesions to spinal nerves or the medulla spinalis), and serious adverse events. Time frame in all outcomes was the longest follow-up period in the studies.
Literature review
The search parameters and terms were determined by the multidisciplinary group. A search protocol was constructed, and the literature search was completed by a search specialist from the Danish Health Authority. The following databases were searched for English, Scandinavian, and German language publications from 2009 to 2019: Guidelines International Network (G-I-N), NICE (UK), Scottish Intercollegiate Guidelines Network (SIGN), CRD/HTA database, The Cochrane Library, Socialstyrelsen (Sweden), SBU (Sweden), Helsedirektoratet (Norway), Folkehelseinstituttet (Norway), Netpunkt, PubMed og Embase. The search terms and strategies are available at https://drks.ortopaedi.dk/soegeprotokol-systematiske-reviews-eller-rct/ and https://drks.ortopaedi.dk/soegeprotokol-nkr-vertebroplasty-guidelines/.
The procedure was a literature search in three steps. In the first step, the search was performed on clinical guidelines, in the second step, the search was performed on systematic reviews and meta-analyses, and in the third step, there was a search on clinical randomized controlled trials. The titles and abstracts were screened by the lead reviewer. The selected papers were collected in full text and screened for the inclusion and exclusion criteria by the lead reviewer and a member from the multidisciplinary group independently. In case of any disagreements, the paper was discussed to achieve consensus (Table 2).
The literature was evaluated in different ways in order to the type of paper. Clinical guidelines were evaluated according to AGREE, systematic reviews according to AMSTAR, and randomized studies according to Cochrane Risk of Bias Tool. In case of high-quality clinical guidelines or systematic reviews, data were extracted directly from these studies. Data from clinical randomized studies were extracted by the lead reviewer and by a member from the group independently. Disagreements on the extracted data were discussed until consensus.
The data and the references were handled using the web-based software Covidence. Data were exported to the RevMan software, and meta-analyses were performed by the methodologist.
The quality of the evidence was graded according to the GRADE definition: very low, low, moderate, and high. The best research evidence available was used to answer the PICO questions.
Creation of recommendations
The methodologist presented the work in tables, and forest plots. The work group suggested recommendation either for or against a treatment and decided from the available evidence whether the recommendation was strong or weak.
In case of no available evidence, an expert opinion based on discussion in the work group was the basis for practical recommendations.
The final recommendation was based on the evidence together with potential positive or negative effects, and the expected patient preferences. From the work described above, the guideline content was developed, and the literature supporting the recommendations was referenced.
Results
In this clinical guideline, three PICO questions were covered. In PICO 1, vertebral augmentation was compared to non-operative treatment in patients with painful vertebral lesions and malignant disease other than hematologic disease. In PICO 2, vertebral augmentation was compared to non-operative treatment in patients with painful vertebral lesions and malignant hematologic disease, and in PICO 3, the risk for complications caused by cement extravasation in patients with painful vertebral lesions with fractures involving the posterior wall of the vertebral body and malignant disease was researched.
A summary of the interventions and recommendations is presented in Table 3.
Discussion
Randomized studies demonstrate significant reduction in patient-reported outcome measures in patients with malignant disease and painful vertebral lesions compared to conservative treatment. The risk of symptomatic cemental leaks in patients with fracture of the posterior wall of the vertebral body is not described in any publications.
To our knowledge, this is the first guideline evaluating treatment efficacy on cancer-related painful vertebral lesions. This guideline demonstrates significant improvement in pain, quality of life, and mobility.
In 2019, a systematic review on the same topic was published [5]. This review included not only randomized studies, but also other publications involving vertebral augmentation techniques. In all, 87 studies were included in the study and a meta-analysis was performed. The review demonstrated clinically relevant improvement in VAS, ODI, and KPS. The results from the review support the conclusion in this guideline.
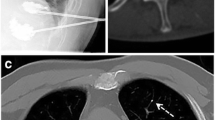
This guideline and the review find a high level of cemental leaks, but symptomatic complications are rare. We did not find any study demonstrating a higher risk of cemental leaks into the spinal canal in case of fracture of the posterior wall. However, care should always be taken while injecting the cement, to decrease the risk of cemental leak into the spinal canal and to avoid escape of cement to the venous system leading to pulmonary cemental embolies. Injecting the cement should be performed under continues radiation.
The major limitation of this guideline is the sparse number of randomized studies.
Furthermore, we did not distinguish between kyphoplasty and vertebroplasty, the number of levels treated, the volume of injected cement, and type of malignant disease. The effect of the procedure and risk of complications may depend on parameters mentioned above.
To find any differences in patient-reported outcome measures in patients with these parameters when comparing cemental augmentation with conservative treatment, randomized studies with a higher number of included patients are necessary.
The primary purpose of vertebral augmentation, especially in patients with malignant disease, is fast and effective pain relief, and in this case, the type of cancer and the prognosis for survival might be less relevant.
We are not aware of evidence describing any correlation between the volume of injected cement and level of pain reduction. In order to avoid complications, the injection of cement is ceased when cemental leaks are observed. The final injected volume depends on both the initial volume of the fractured vertebral body and on any leaks observed.
We expect that the majority of patients with malignant disease and painful vertebral lesions will accept cemental augmentation. Reduction in pain for these patients is of great importance. In addition, the risk of symptomatic complications is low. Life expectancy for these patients may be short, and pain is a major impact factor on quality of life.
To confirm the conclusion in this guideline, more randomized studies on patients with different malignant diseases and painful vertebral lesions comparing percutaneous vertebroplasty/kyphoplasty with conservative treatment are needed. If possible, double-blinded studies should be performed in order to avoid confounders and risk of bias.
Conclusion
A multidisciplinary work group developed a Danish National Clinical Guideline regarding cemental augmentation as treatment for painful vertebral lesions, in patients with malignant disease. The recommendations were based on either weak-to-moderate evidence or professional consensus.
The guideline work group recommends vertebral augmentation as treatment for painful vertebral lesions in patients with malignant disease. Fracture of the posterior wall is not a contraindication for cemental augmentation, but care should always be taken while injecting the cement, to decrease the risk of cemental leak into the spinal canal.
References
Galibert PDH, Rosat P, Le Gars D (1987) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 33(2):166–168
Zoarski GH, Stallmeyer MJB, Obuchowski A (2002) Percutaneous vertebroplasty: A to Z. Tech Vasc Interv Radiol 5(4):223–238
LE Bilsky MH, Raizer J, Lee H, Boland P (1999) The diagnosis and treatment of metastatic spinal tumor. Oncologist 4:459–469
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed) 336(7650):924–926
Sørensen ST, Carreon L, Rousing R, Andersen MØ (2019) Vertebroplasty or kyphoplasty as palliative treatment for cancer-related vertebral compression fractures: a systematic review. Spine J. 19(6):1067–1075
Berenson J, Jarzem P, Zonder J, Schechtman K, Tillman JB, Bastian L, Ashraf T, Vrionis F (2011) Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol. 12(3):225–235
Audat ZA, Hajyousef MH, Fawareh MD, Alawneh KM, Odat MA, Barbarawi MM et al (2016) Comparison if the addition of multilevel vertebral augmentation to conventional therapy will improve the outcome of patients with multiple myeloma. Scoliosis Spinal Disord. 11:47
Amoretti N, Diego P, Amélie P, Andreani O, Foti P, Schmid-Antomarchi H et al (2018) Percutaneous vertebroplasty in tumoral spinal fractures with posterior vertebral wall involvement: feasibility and safety. Eur J Radiol 104:38–42
Basile A, Cavalli M, Fiumara P, Di Raimondo F, Mundo E, Caltabiano G et al (2011) Vertebroplasty in multiple myeloma with osteolysis or fracture of the posterior vertebral wall usefulness of a delayed cement injection. Skeletal Radiol. 40(7):913–919
Cianfoni A, Raz E, Mauri S, Di Lascio S, Reinert M, Pesce G et al (2015) Vertebral augmentation for neoplastic lesions with posterior wall erosion and epidural mass. AJNR Am J Neuroradiol 36(1):210–218
Kirkegaard AO, Sørensen ST, Ziegler DS, Carreon L, Andersen MØ, Rousing R (2018) Percutaneous vertebroplasty is safe and effective for cancer-related vertebral compression fractures. Dan Med J 65(10):A5509
Molloy S, Sewell MD, Platinum J, Patel A, Selvadurai S, Hargunani R et al (2016) Is balloon kyphoplasty safe and effective for cancer-related vertebral compression fractures with posterior vertebral body wall defects? J Surg Oncol 113(7):835–842
Reyad RM, Ghobrial HZ, Hakim SM, Hashem RH, Elsaman A, Shaaban MH (2017) Thick cement usage in percutaneous vertebroplasty for malignant vertebral fractures at high risk for cement leakage. Diagn Interv Imaging 98(10):721–728
Acknowledgements
We would like to acknowledge the working group: Andreas Ole Kirkegaard, lead reviewer, MD, Bodil Abild Jespersen, senior consultant, Aarhus University Hospital, Conni Skrubbeltang, research librarian, the Danish Health Authority, Else Bay Andresen, senior consultant, Lillebelt Hospital, Eva Holtved, senior consultant, Odense University Hospital, Gitte Aagaard, nurse, Randers Regional Hospital, Hans Peter Henriksen, general practitioner, Jens Aaboe, Method Consultant, the Danish Health Authority, Leif Hougaard Sørensen, senior consultant, Aarhus University hospital, Marianne Dyrby Lorenzen, chairman, Lillebelt Hospital, Michael Nielsen, senior consultant, Capio CFR, Mikkel Østerheden Andersen, senior consultant, Lillebelt Hospital, Rikke Rousing, senior consultant, Lillebelt Hospital, Thomas Lund, senior consultant, Odense University Hospital, Viola Olesen, Junior Consultant, Copenhagen University Hospital, Rigshospitalet.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Potential conflicts of interest have been declared by all involved partners and made publicly available on the Danish Spine Society webpage (in Danish) https://drks.ortopaedi.dk/habilitetserklaeringer/.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rousing, R., Kirkegaard, A.O., Nielsen, M. et al. Percutaneous vertebroplasty as treatment of malignant vertebral lesions: a systematic review and GRADE evaluation resulting in a Danish national clinical guideline. Eur Spine J 29, 1573–1579 (2020). https://doi.org/10.1007/s00586-020-06392-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06392-w