Abstract
Purpose
The purpose was to investigate reasons and their frequency for why total disc replacement (TDR) specialty surgeons performed anterior cervical discectomy and fusion (ACDF) rather than TDR.
Methods
A consecutive series of 464 patients undergoing cervical spine surgery during a 5-year period by three TDR specialty surgeons was reviewed. For each ACDF, the reason for not performing TDR was recorded.
Results
TDR was performed in 76.7% of patients (n = 356) and ACDF in 23.3% (n = 108). The most common reason for ACDF versus TDR was anatomical (conditions that may not be adequately addressed with TDR and/or may interfere with device function), which occurred in 64 of 464 patients (13.79%). The second most common reason was insurance (denial/lack of coverage n = 17, 3.23%), and deformity/kyphosis not addressable with TDR was noted in 13 (2.80%). Pseudoarthrosis repair led to ACDF in three patients (0.65%), two did not receive TDR due to osteoporosis (0.43%), and in two others (0.43%) ACDF was undertaken due to high risk of heterotopic ossification. There was one case (0.22%) each of: nickel allergy, trauma with posterior element fracture, TDR removal, multiple prior cervical spine surgeries, concern about artifact on future imaging studies, benign osteoblastic bone, and limitation to adequate surgical approach for TDR. ACDF patients’ mean age was significantly greater than TDR patients’ (55.3 vs. 46.7 years; p < 0.01). TDR group had significantly more single-level procedures than ACDF (60.8% vs. 43.5%; p < 0.05).
Conclusion
The most common reason for ACDF versus TDR was anatomy that may compromise segmental stability and/or TDR functionality. Older age and greater number of operated levels may be related to anatomical factors, primarily significant osteophytes and severely degenerated facets. These factors, as well as deformity/kyphosis, are more common in older patients and require multi-level treatment. This study found that many patients are good cervical TDR candidates; however, even among TDR specialists, ACDF may be preferred where it is prudent to not take undue risks.
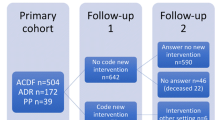
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material


Similar content being viewed by others
References
Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, Darden B (2009) Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 9(4):275–286. https://doi.org/10.1016/j.spinee.2008.05.006
Lavelle WF, Riew KD, Levi AD, Florman JE (2019) 10-year outcomes of cervical disc replacement with the BRYAN(R) Cervical Disc: results from a prospective, randomized, controlled clinical trial. Spine 44(9):601–608. https://doi.org/10.1097/brs.0000000000002907
Coric D, Guyer RD, Nunley PD, Musante D, Carmody C, Gordon C, Lauryssen C, Boltes MO, Ohnmeiss DD (2018) Prospective, randomized multicenter study of cervical arthroplasty versus anterior cervical discectomy and fusion: 5-year results with a metal-on-metal artificial disc. J Neurosurg Spine 28(3):252–261. https://doi.org/10.3171/2017.5.spine16824
Lanman TH, Burkus JK, Dryer RG, Gornet MF, McConnell J, Hodges SD (2017) Long-term clinical and radiographic outcomes of the Prestige LP artificial cervical disc replacement at 2 levels: results from a prospective randomized controlled clinical trial. J Neurosurg Spine 27(1):7–19. https://doi.org/10.3171/2016.11.spine16746
Vaccaro A, Beutler W, Peppelman W, Marzluff JM, Highsmith J, Mugglin A, DeMuth G, Gudipally M, Baker KJ (2013) Clinical outcomes with selectively constrained SECURE-C cervical disc arthroplasty: two-year results from a prospective, randomized, controlled, multicenter investigational device exemption study. Spine 38(26):2227–2239
Hu Y, Lv G, Ren S, Johansen D (2016) Mid- to long-term outcomes of cervical disc arthroplasty versus anterior cervical discectomy and fusion for treatment of symptomatic cervical disc disease: a systematic review and meta-analysis of eight prospective randomized controlled trials. PLoS ONE 11(2):e0149312. https://doi.org/10.1371/journal.pone.0149312
Lu VM, Mobbs RJ, Phan K (2019) Clinical outcomes of treating cervical adjacent segment disease by anterior cervical discectomy and fusion versus total disc replacement: a systematic review and meta-analysis. Glob Spine J 9(5):559–567. https://doi.org/10.1177/2192568218789115
Xiong Y, Xu L, Yu X, Yang Y, Zhao D, Hu Z, Li C, Zhao H, Duan L, Zhang B, Chen S, Liu T (2018) Comparison of 6-year follow-up result of hybrid surgery and anterior cervical discectomy and fusion for the treatment of contiguous two-segment cervical degenerative disc diseases. Spine 43(20):1418–1425. https://doi.org/10.1097/brs.0000000000002639
Wu TK, Wang BY, Deng MD, Hong Y, Rong X, Chen H, Meng Y, Liu H (2017) A comparison of anterior cervical discectomy and fusion combined with cervical disc arthroplasty and cervical disc arthroplasty for the treatment of skip-level cervical degenerative disc disease: a retrospective study. Medicine (Baltimore) 96(41):e8112. https://doi.org/10.1097/md.0000000000008112
Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR (2008) The prevalence of indications and contraindications to cervical total disc replacement. Spine J 8(5):711–716. https://doi.org/10.1016/j.spinee.2007.06.018
Ding D, Shaffrey ME (2012) Cervical disk arthroplasty: patient selection. Clin Neurosurg 59:91–97
Tu TH, Lee CY, Kuo CH, Wu JC, Chang HK, Fay LY, Huang WC, Cheng H (2019) Cervical disc arthroplasty for less-mobile discs. J Neurosurg Spine 1:2. https://doi.org/10.3171/2019.2.spine181472
Patwardhan AG, Carandang G, Voronov LI, Havey RtM, Paul GA, Lauryssen C, Coric D, Dimmig T, Musante D (2016) Are collapsed cervical discs amenable to total disc arthroplasty? Analysis of prospective clinical data with 2-year follow-up. Spine 41(24):1866–1875. https://doi.org/10.1097/brs.0000000000001793
Chung SB, Muradov JM, Lee SH, Eoh W, Kim ES (2012) Uncovertebral hypertrophy is a significant risk factor for the occurrence of heterotopic ossification after cervical disc replacement: survivorship analysis of Bryan disc for single-level cervical arthroplasty. Acta Neurochir (Wien) 154(6):1017–1022
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors did have disclosures for cervical TDR, though none are directly related to this study and no funding was received to support this study or the preparation of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Guyer, R.D., Ohnmeiss, D.D., Blumenthal, S.L. et al. In which cases do surgeons specializing in total disc replacement perform fusion in patients with cervical spine symptoms?. Eur Spine J 29, 2665–2669 (2020). https://doi.org/10.1007/s00586-019-06275-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06275-9