Abstract
Purpose
Anterior cervical spine surgery is associated with postoperative dysphagia, sore throat and dysphonia. It is unclear, whether this is caused by increased endotracheal tube (ETT) cuff pressure after retractor placement. This study aims to assess the effect of ETT cuff pressure adjustment on postoperative dysphagia, sore throat and dysphonia.
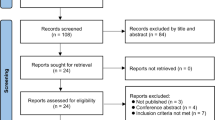
Methods
In this, single-centre, observer and patient-blinded randomized controlled trial patients treated with anterior cervical spine surgery were randomized to adjustment of the ETT cuff pressure to 20 mmHg after placement of the retractor versus no adjustment. Primary outcome was the incidence and severity of postoperative dysphagia. Secondary outcomes were sore throat and dysphonia. Outcomes were evaluated on day one and 2 months after the operation.
Results
Of 177 enrolled patients, 162 patients (92.5%) could be evaluated. The incidence of dysphagia was 75.9% on day one and 34.6% 2 months after surgery. Dysphagia in the intervention and control group was present in 77.8% versus 74.1% of patients on day one (odds ratio (OR) 1.2, 95% confidence interval (CI) (0.6–2.5)) and 28.4% versus 40.7% of patients after 2 months (OR 0.6, 95% CI 0.3–1.1), respectively. Severity of dysphagia, sore throat and dysphonia was similar in both groups.
Conclusions
Anterior cervical spine surgery is accompanied by a high incidence of postoperative dysphagia, lasting until at least 2 months after surgery in over a third of our patients. Adjusting ETT cuff pressure to 20 mmHg after retractor placement, as compared to controls, did not lower the risk for both short- and long-term dysphagia.
Netherlands National Trial Registry Number: NTR 3542.
Graphical abstract
These slides can be retrieved under electronic supplementary material.


Similar content being viewed by others
References
Sperry RJ, Johnson JO, Apfelbaum RI (1993) Endotracheal tube cuff pressure increases significantly during anterior cervical fusion with the Caspar instrumentation system. Anesth Analg 76(6):1318–1321
Winslow CP, Winslow TJ, Wax MK (2001) Dysphonia and dysphagia following the anterior approach to the cervical spine. Arch Otolaryngol Neck Surg 127(1):51–55
Ratnaraj J, Todorov A, McHugh T, Cheng MA, Lauryssen C (2002) Effects of decreasing endotracheal tube cuff pressures during neck retraction for anterior cervical spine surgery. J Neurosurg 97(2 Suppl):176–179
Bulger RF, Rejowski JE, Beatty RA (1985) Vocal cord paralysis associated with anterior cervical fusion: considerations for prevention and treatment. J Neurosurg 62(5):657–661
Audu P, Artz G, Scheid S, Harrop J, Albert TJ, Vaccaro A, Hilibrand A, Sharan A, Spiegal J, Rosen M (2006) Recurrent laryngeal nerve palsy after anterior cervical spine surgery: the impact of endotracheal tube cuff deflation, reinflation, and pressure adjustment. Anesthesiology 105(5):898–901
Lou Sole M, Penoyer DA, Su X, Jimenez E, Kalita SJ, Poalillo E, Byers JF, Bennett M, Ludy JE (2009) Assessment of endotracheal cuff pressure by continuous monitoring: a pilot study. Am J Crit Care 18(2):133–143
Liu J, Zhang X, Gong W, Li S, Wang F, Fu S, Zhang M, Hang Y (2010) Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesth Analg 111(5):1133–1137
Liu J, Hai Y, Kang N, Chen X, Zhang Y (2017) Risk factors and preventative measures of early and persistent dysphagia after anterior cervical spine surgery: a systematic review. Eur Spine J 27(6):1209–1218
Arts MP, Rettig TC, de Vries J, Wolfs JF, in ’t Veld BA (2013) Does maintaining endotracheal tube cuff pressure at 20 mm Hg prevent dysphagia after anterior cervical spine surgery? BMC Musculoskelet Disord 14(1):280
Griesdale DEG, Liu D, McKinney J, Choi PT (2012) Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anaesth 59(1):41–52
Aziz MF, Healy D, Kheterpal S, Fu RF, Dillman D, Brambrink AM (2011) Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology 114(1):34–41
Fisahn C, Schmidt C, Rustagi T, Moisi M, Iwanaga J, Norvell DC, Tubbs RS, Schildhauer TA, Chapman JR (2018) Comparison of chronic dysphagia in standalone versus conventional plate and cage fusion. World Neurosurg 109:e382–e388
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976) 27(22):2453–2458
Karnell MP, Melton SD, Childes JM, Coleman TC, Dailey SA, Hoffman HT (2007) Reliability of clinician-based (GRBAS and CAPE-V) and patient-based (V-RQOL and IPVI) documentation of voice disorders. J Voice 21(5):576–590
De Bodt MS, Wuyts FL, Van De Heyning PH, Croux C (1997) Test-retest study of the GRBAS scale: influence of experience and professional background on perceptual rating of voice quality. J Voice 11(1):74–80
IPA (1999) Handbook of the International Phonetic Association. http://dla.library.upenn.edu/dla/olac/record.html?id=www_mpi_nl_1839_00-0000-0000-0003-89CB-D
Hartrick CT, Kovan JP, Shapiro S (2003) The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract 3(4):310–316
Olsson EC, Jobson M, Lim MR (2015) Risk factors for persistent dysphagia after anterior cervical spine surgery. Orthopedics 38(4):e319–e323
Kalb S, Reis MT, Cowperthwaite MC, Fox DJ, Lefevre R, Theodore N, Papadopoulos SM, Sonntag VKH (2012) Dysphagia after anterior cervical spine surgery: incidence and risk factors. World Neurosurg 77(1):183–187
Lee MJ, Bazaz R, Furey CG, Yoo J (2007) Risk factors for dysphagia after anterior cervical spine surgery: a two-year prospective cohort study. Spine J 7(2):141–147
Kowalczyk Izabela, Ryu Won Hyung A, Rabin Doron, Arango Miguel, Duggal Neil (2015) Reduced endotracheal tube cuff pressure to assess dysphagia after anterior cervical spine surgery. J Spinal Disord Tech 28(10):E552–E558
Anderson KK, Arnold PM (2013) Oropharyngeal dysphagia after anterior cervical spine surgery: a review. Glob Spine J 3(4):273–286
Nam TW, Lee DH, Shin JK, Goh TS, Lee JS (2013) Effect of intravenous dexamethasone on prevertebral soft tissue swelling after anterior cervical discectomy and fusion. Acta Orthop Belg 79(2):211–215
Wang T, Ma L, Yang D-L, Wang H, Bai Z-L, Zhang L-J, Ding W-Y (2017) Factors predicting dysphagia after anterior cervical surgery: a multicenter retrospective study for 2 years of follow-up. Medicine (Baltimore) 96(34):e7916
Acknowledgements
We acknowledge Mrs. A. Hanschke and Mrs. Ch. Severijns for their role as research nurse in collecting the voice recordings, support in the data collection and obtaining the research grant. Furthermore, we acknowledge the department of speech and language therapy of the Hogeschool Rotterdam for their contribution in judging the GRADE score with regard to dysphonia
Funding
This study was funded by a small project grant from the internal scientific board of the Haaglanden Medical Centre to ensure the cooperation of research nurses and the purchase of the digital voice recorder.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
in ’t Veld, B.A., Rettig, T.C.D., de Heij, N. et al. Maintaining endotracheal tube cuff pressure at 20 mmHg during anterior cervical spine surgery to prevent dysphagia: a double-blind randomized controlled trial. Eur Spine J 28, 353–361 (2019). https://doi.org/10.1007/s00586-018-5798-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5798-3