Abstract
Purpose
To investigate the effect of the preoperative cross-sectional area (CSA) of the semispinalis cervicis on postoperative loss of cervical lordosis (LCL) after laminoplasty.
Methods
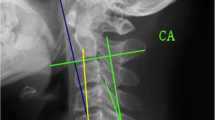
A total of 144 patients who met the inclusion criteria between January 1999 and December 2015 were enrolled. Radiographic assessments were performed to evaluate the T1 slope, C2-7 sagittal vertical axis (SVA), cephalad vertebral level undergoing laminoplasty (CVLL), preoperative C2-7 Cobb angle, and preoperative CSA of the semispinalis cervicis.
Results
The T1 slope and the summation of the CSAs (SCSA) at each level of the semispinalis cervicis correlated with LCL, whereas the C2-7 SVA, CVLL, and preoperative C2-7 Cobb angle did not. Multiple regression analysis demonstrated that a high T1 slope and a low SCSA of the semispinalis cervicis were associated with LCL after laminoplasty in patients with cervical spondylotic myelopathy (CSM). The CSA of the semispinalis cervicis at the C6 level had the greatest association with LCL, which suddenly decreased with a LCL of 10°. The best cutoff point of the CSA of the semispinalis cervicis at the C6 level, which predicts LCL > 10°, was 154.5 mm2 (sensitivity 74.3%; specificity 71.6%; area under the curve 0.828; 95% confidence interval 0.761–0.895).
Conclusion
Preoperative SCSA of the semispinalis cervicis was a risk factor for LCL after laminoplasty. Spine surgeons should evaluate semispinalis cervicis muscularity at the C6 level when planning laminoplasty for patients with CSM.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.







Similar content being viewed by others
References
Cao J, Zhang J, Yang D, Yang L, Shen Y (2017) Multivariate analysis of factors associated with kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kyphotic alignment. Sci Rep 7:43443. https://doi.org/10.1038/srep43443
Zhang JT, Li JQ, Niu RJ, Liu Z, Tong T, Shen Y (2017) Predictors of cervical lordosis loss after laminoplasty in patients with cervical spondylotic myelopathy. Eur Spine J 26:1205–1210. https://doi.org/10.1007/s00586-017-4971-4
Ratliff JK, Cooper PR (2003) Cervical laminoplasty: a critical review. J Neurosurg 98:230–238
Baba H, Uchida K, Maezawa Y, Furusawa N, Azuchi M, Imura S (1996) Lordotic alignment and posterior migration of the spinal cord following en bloc open-door laminoplasty for cervical myelopathy: a magnetic resonance imaging study. J Neurol 243:626–632
Kim B, Yoon DH, Ha Y, Yi S, Shin DA, Lee CK, Lee N, Kim KN (2016) Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J 16:219–225. https://doi.org/10.1016/j.spinee.2015.10.042
Liu J, Ebraheim NA, Sanford CG Jr, Patil V, Haman SP, Ren L, Yang H (2007) Preservation of the spinous process-ligament-muscle complex to prevent kyphotic deformity following laminoplasty. Spine J 7:159–164. https://doi.org/10.1016/j.spinee.2006.07.007
Kim P, Murata H, Kurokawa R, Takaishi Y, Asakuno K, Kawamoto T (2007) Myoarchitectonic spinolaminoplasty: efficacy in reconstituting the cervical musculature and preserving biomechanical function. J Neurosurg Spine 7:293–304. https://doi.org/10.3171/SPI-07/09/293
Hosono N, Sakaura H, Mukai Y, Ishii T, Yoshikawa H (2005) En bloc laminoplasty without dissection of paraspinal muscles. J Neurosurg Spine 3:29–33. https://doi.org/10.3171/spi.2005.3.1.0029
Tani S, Isoshima A, Nagashima Y, Tomohiko Numoto R, Abe T (2002) Laminoplasty with preservation of posterior cervical elements: surgical technique. Neurosurgery 50:97–101 (discussion 101-102)
Yoshida M, Otani K, Shibasaki K, Ueda S (1992) Expansive laminoplasty with reattachment of spinous process and extensor musculature for cervical myelopathy. Spine 17:491–497
Machino M, Yukawa Y, Hida T, Ito K, Nakashima H, Kanbara S, Morita D, Kato F (2012) Cervical alignment and range of motion after laminoplasty: radiographical data from more than 500 cases with cervical spondylotic myelopathy and a review of the literature. Spine 37:E1243–E1250. https://doi.org/10.1097/BRS.0b013e3182659d3e
Kim TH, Lee SY, Kim YC, Park MS, Kim SW (2013) T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine 38:E992–E997. https://doi.org/10.1097/BRS.0b013e3182972e1b
Fujimura Y, Nishi Y (1996) Atrophy of the nuchal muscle and change in cervical curvature after expansive open-door laminoplasty. Arch Orthop Trauma Surg 115:203–205
Zotti MGT, Boas FV, Clifton T, Piche M, Yoon WW, Freeman BJC (2017) Does pre-operative magnetic resonance imaging of the lumbar multifidus muscle predict clinical outcomes following lumbar spinal decompression for symptomatic spinal stenosis? Eur Spine J 26:2589–2597. https://doi.org/10.1007/s00586-017-4986-x
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166:193–199. https://doi.org/10.1148/radiology.166.1.3336678
Elliott JM, Jull GA, Noteboom JT, Durbridge GL, Gibbon WW (2007) Magnetic resonance imaging study of cross-sectional area of the cervical extensor musculature in an asymptomatic cohort. Clin Anat 20:35–40. https://doi.org/10.1002/ca.20252
Sakai K, Yoshii T, Hirai T, Arai Y, Torigoe I, Tomori M, Sato H, Okawa A (2016) Cervical sagittal imbalance is a predictor of kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kyphotic alignment. Spine 41:299–305. https://doi.org/10.1097/BRS.0000000000001206
Lin S, Zhou F, Sun Y, Chen Z, Zhang F, Pan S (2015) The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty. Eur Spine J 24:127–135. https://doi.org/10.1007/s00586-014-3605-3
Ogawa Y, Toyama Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, Hirabayashi H, Hirabayashi K (2004) Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine 1:168–174. https://doi.org/10.3171/spi.2004.1.2.0168
Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M (2003) Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine 28:1258–1262. https://doi.org/10.1097/01.BRS.0000065487.82469.D9
Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, Lafage V, Shaffrey CI, Schwab F, Ames CP, Issg (2015) The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 76(Suppl 1):S14–S21. https://doi.org/10.1227/01.neu.0000462074.66077.2b (discussion S21)
Masini M, Maranhao V (1997) Experimental determination of the effect of progressive sharp-angle spinal deformity on the spinal cord. Eur Spine J 6:89–92
Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, Yoshikawa H (2007) Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: part 1: clinical results and limitations of laminoplasty. Spine 32:647–653. https://doi.org/10.1097/01.brs.0000257560.91147.86
Cho JH, Ha JK, Kim DG, Song KY, Kim YT, Hwang CJ, Lee CS, Lee DH (2014) Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty? Spine 39:E1575–E1581. https://doi.org/10.1097/BRS.0000000000000614
Iizuka H, Nakajima T, Iizuka Y, Sorimachi Y, Ara T, Nishinome M, Takagishi K (2007) Cervical malalignment after laminoplasty: relationship to deep extensor musculature of the cervical spine and neurological outcome. J Neurosurg Spine 7:610–614. https://doi.org/10.3171/SPI-07/12/610
Iizuka H, Shimizu T, Tateno K, Toda N, Edakuni H, Shimada H, Takagishi K (2001) Extensor musculature of the cervical spine after laminoplasty: morphologic evaluation by coronal view of the magnetic resonance image. Spine 26:2220–2226
Vasavada AN, Li S, Delp SL (1998) Influence of muscle morphometry and moment arms on the moment-generating capacity of human neck muscles. Spine 23:412–422
Maeda T, Arizono T, Saito T, Iwamoto Y (2002) Cervical alignment, range of motion, and instability after cervical laminoplasty. Clin Orthop Relat Res 401:132–138
Sakaura H, Hosono N, Mukai Y, Oshima K, Iwasaki M, Yoshikawa H (2008) Preservation of the nuchal ligament plays an important role in preventing unfavorable radiologic changes after laminoplasty. J Spinal Disord Tech 21:338–343. https://doi.org/10.1097/BSD.0b013e3181453de4
Kurokawa R, Kim P (2015) Cervical laminoplasty: the history and the future. Neurol Med Chir 55:529–539. https://doi.org/10.2176/nmc.ra.2014-0387
Duetzmann S, Cole T, Ratliff JK (2015) Cervical laminoplasty developments and trends, 2003–2013: a systematic review. J Neurosurg Spine 23:24–34. https://doi.org/10.3171/2014.11.SPINE14427
Lind B, Sihlbom H, Nordwall A, Malchau H (1989) Normal range of motion of the cervical spine. Arch Phys Med Rehabil 70:692–695
Shiraishi T, Kato M, Yato Y, Ueda S, Aoyama R, Yamane J, Kitamura K (2012) New techniques for exposure of posterior cervical spine through intermuscular planes and their surgical application. Spine 37:E286–E296. https://doi.org/10.1097/BRS.0b013e318239cc7e
Wang L, Wang Y, Yu B, Li Z, Liu X (2015) Open-door versus French-door laminoplasty for the treatment of cervical multilevel compressive myelopathy. J Clin Neurosci 22:450–455. https://doi.org/10.1016/j.jocn.2014.08.022
Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, Kitagawa T, Nakamura K (2001) Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine 26:479–487
Hirabayashi K, Satomi K (1988) Operative procedure and results of expansive open-door laminoplasty. Spine 13:870–876
Iizuka H, Nakagawa Y, Shimegi A, Tsutsumi S, Toda N, Takagishi K, Shimizu T (2005) Clinical results after cervical laminoplasty: differences due to the duration of wearing a cervical collar. J Spinal Disord Tech 18:489–491
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval
This study was approved by the Institutional Review Board of the Asan Medical Center (IRB#: 2017-1120).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, BJ., Park, J.H., Jeon, SR. et al. Importance of the preoperative cross-sectional area of the semispinalis cervicis as a risk factor for loss of lordosis after laminoplasty in patients with cervical spondylotic myelopathy. Eur Spine J 27, 2720–2728 (2018). https://doi.org/10.1007/s00586-018-5726-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5726-6