Abstract
Introduction
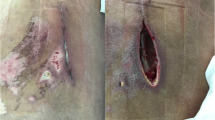
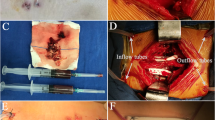
The treatment of postoperative deep spinal wound infection involves debridement and intravenous antibiotics. Authors have previously reported success in a small series of patients treated with vacuum-assisted closure (VAC) therapy, but its use over exposed dura is controversial and the outcome has not been reported in large series.
Purpose
To review the outcomes following the treatment of postoperative spinal infections with VAC therapy, particularly those with exposed dura.
Methods
This is a review of prospectively collected data in 42 patients, all of whom had deep postoperative spinal infections. 30 of these patients had exposed dura. All patients had an initial debridement followed by application of VAC Whitefoam (with exposed dura) or grey Granufoam (where no dura was exposed). Pressure was set at 50 mmHg with exposed dura or 125 mmHg where no dura was exposed. All patients underwent a minimum 6 week course of antibiotics. We report on the number of visits to theatre required for dressing changes and debridement and the eventual outcomes.
Results
Five patients required a flap reconstruction. Two patients died before definitive final closure due to other complications (pneumonia and stroke). In all the other patients, their wounds healed fully. A mean of 2.3 infection surgeries were required to eradicate infection and achieve wound closure.
Conclusions
This is one of the largest studies which confirms the safety and efficacy of VAC dressings in patients with spinal wound infections, even when the dura is exposed.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
References
Weinstein MA, McCabe JP, Cammisa FP (2000) Postoperative spinal wound infection: a review of 2391 consecutive index procedures. J Spinal Disord 13:422–426
Malamo-Lada H, Zarkotou O, Nikolaides N et al (1999) Wound infections following posterior spinal instrumentation for paralytic scoliosis. Clin Microbiol Infect 5:135–139
Glassman SD, Dimar JR, Puno RM, Johnson JR (1996) Salvage of instrumental lumbar fusions complicated by surgical wound infection. Spine 21:2163–2169
Calderone RR, Garland DE, Capen DA, Oster H (1996) Cost of medical care for postoperative spinal infections. Orthop Clin N Am 27:171–182
Saxena V, Hwang C-W, Huang S et al (2004) Vacuum-assisted closure: microdeformations of wounds and cell proliferation. Plast Reconstr Surg 114:1086–1096
Canavese F, Gupta S, Krajbich JI, Emara KM (2008) Vacuum-assisted closure for deep infection after spinal instrumentation for scoliosis. J Bone Joint Surg Br 90:377–381
Jones GA, Butler J, Lieberman I, Schlenk R (2007) Negative-pressure wound therapy in the treatment of complex postoperative spinal wound infections: complications and lessons learned using vacuum-assisted closure. J Neurosurg Spine 6:407–411
Mehbod A, Ogilvie JW, Pinto MR et al (2005) Postoperative deep wound infections in adults after spinal fusion: management with vacuum-assisted wound closure. J Spinal Disord Tech 18:14–17
Ploumis A, Mehbod A, Dressel TD et al (2008) Therapy of spinal wound infections using vacuum-assisted wound closure: risk factors leading to resistance to treatment. J Spinal Disord Tech 21:320–323
Powers AK, Neal MT, Argenta LC et al (2013) Vacuum-assisted closure for complex cranial wounds involving the loss of dura mater. J Neurosurg 118:302–308
Subotic U, Kluwe W, Oesch V (2011) Community-associated methicillin-resistant staphylococcus aureus-infected chronic scalp wound with exposed dura in a 10-year-old boy: vacuum-assisted closure is a feasible option: case report. Neurosurgery 68:E1481–E1484
Marathe US, Sniezek JC (2004) Use of the vacuum-assisted closure device in enhancing closure of a massive skull defect. Laryngoscope 114:961–964
Walma MS, Burbach JPM, Verheijen PM et al (2016) Vacuum-assisted closure therapy for infected perineal wounds after abdominoperineal resection. A retrospective cohort study. Int J Surg 26:18–24
Yoshimoto A, Inoue T, Fujisaki M et al (2016) Efficacy of vacuum-assisted closure therapy on rehabilitation during the treatment for surgical site infection after cardiovascular surgery. Gen Thorac Cardiovasc Surg 64:464–469
Lambert KV, Hayes P, McCarthy M (2005) Vacuum assisted closure: a review of development and current applications. Eur J Vasc Endovasc Surg 29:219–226
Gabriel A, Shores J, Bernstein B et al (2009) A clinical review of infected wound treatment with (V.A.C.) therapy: experience and case series. Int Wound J 6:221–225
DeFranzo AJ, Argenta LC, Marks MW et al (2001) The use of vacuum-assisted closure therapy for the treatment of lower-extremity wounds with exposed bone. Plast Reconstr Surg 108:1184–1191
Picada R, Winter RB, Lonstein JE et al (2000) Postoperative deep wound infection in adults after posterior lumbosacral spine fusion with instrumentation: incidence and management. J Spinal Disord 13:42–45
Mithani SK, Tufaro AP (2006) Management of wound complications in spinal surgery. Neurosurg Q 16:9–14
Tsubouchi N, Fujibayashi S, Otsuki B et al (2017) Risk factors for implant removal after spinal surgical site infection. Eur Spine J. https://doi.org/10.1007/s00586-017-5294-1
Muschik M, Lück W, Schlenzka D (2004) Implant removal for late-developing infection after instrumented posterior spinal fusion for scoliosis: reinstrumentation reduces loss of correction. A retrospective analysis of 45 cases. Eur Spine J 13:645–651
Collins I, Wilson-MacDonald J, Chami G et al (2008) The diagnosis and management of infection following instrumented spinal fusion. Eur Spine J 17:445–450
Vitaz TW, Oishi M, Welch WC et al (2004) Rotational and transpositional flaps for the treatment of spinal wound dehiscence and infections in patient populations with degenerative and oncological disease. J Neurosurg 100:46–51
Abbas Khan MA, Chipp E, Hardwicke J et al (2010) The use of dermal regeneration template (Integra®) for reconstruction of a large full-thickness scalp and calvarial defect with exposed dura. J Plast Reconstr Aesthet Surg 63:2168–2171
Donovan DJ, Person DA (2006) Giant eccrine adenocarcinoma of the scalp with intracranial invasion: resection and reconstruction using a vacuum-assisted closure device: technical case report. Neurosurgery 58(4 Suppl 2):E371
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, R., Beder, D., Street, J. et al. The use of vacuum-assisted closure in spinal wound infections with or without exposed dura. Eur Spine J 27, 2536–2542 (2018). https://doi.org/10.1007/s00586-018-5612-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5612-2