Abstract
Purpose
The measurement of distal motor latency (DML) is an established method for diagnosing entrapment peripheral neuropathy. DML can also serve as an index for disease severity and prognosis. We considered that measuring DML could be useful in estimating the severity of spinal root impairment and predicting prognosis in patients with lumbar spinal stenosis (LSS). The purpose of this study was to investigate the efficacy of intraoperative direct electrical stimulation of the spinal root and the measurement of DML in LSS.
Methods
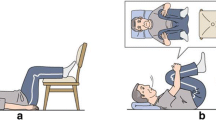
In 39 patients with LSS, a total of 93 spinal roots were stimulated, and evoked electromyography was recorded at the leg muscles after decompression. DML was measured and its correlation with clinical severity, as evaluated by Zurich claudication questionnaire (ZCQ) and Short Form 36 (SF-36), was investigated.
Results
For the stimulation of the L3, L4, and L5 spinal root, the mean DML (ms) were 6.8 (±1.4), 7.4 (±1.3), and 6.0 (±1.3) in gluteus medius, 9.3 (±1.5), 9.2 (±1.5), and 9.0 (±1.6) in biceps femoris, 9.7 (±1.0), 9.8 (±1.8), and 9.4 (±1.2) in vastus medialis, 16.1 (±1.0), 14.7 (±1.3), and 14.1 (±1.5) in tibialis anterior, and 16.4 (±1.4), 14.3 (±1.8), and 13.9 (±1.9) in gastrocnemius muscles. Statistically significant positive correlations were observed between DML and height. Preoperative symptom and function scores of ZCQ and postoperative bodily pain scores of SF-36 were significantly worse in the patients with prolonged DML.
Conclusions
DML is thought to be useful for estimating the severity of spinal root impairment and for predicting the prognosis.



Similar content being viewed by others
References
Mondelli M, Reale F, Sicurelli F, Padua L (2000) Relationship between the self-administered Boston questionnaire and electrophysiological findings in follow-up of surgically-treated carpal tunnel syndrome. J Hand Surg Br 25:128–134
Dudley Porras AF, Rojo Alaminos P, Vinuales JI, Ruiz Villamanan MA (2000) Value of electrodiagnostic tests in carpal tunnel syndrome. J Hand Surg Br 25:361–365
Yoshimoto M, Miyakawa T, Takebayashi Ida K, Tanimoto K, Kawamura S, Yamashita T (2014) Microendoscopy-assisted muscle-preserving interlaminar decompression for lumbar spinal stenosis: clinical results of consecutive 105 cases with more than 3-year follow-up. Spine 39:E318–E325
Stucki G, Daltroy L, Liang MH, Lipson SJ, Fossel AH, Katz JN (1996) Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine 21:796–803
Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K (1998) Translation, adaptation, and validation of the SF-36 Health Survey for the use in Japan. J Clin Epidemiol 51:1037–1044
Fukuhara S, Ware JE, Kosinski M, Wada S, Gandek B (1998) Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol 51:1045–1053
Schizas C, Theumann N, Burn A, Tansey R, Wardlaw D, Smith FW, Kulik G (2010) Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine 35:1919–1924
Jaiser SR, Barnes JD, Baker SN, Baker MR (2015) A multiple regression model of normal central and peripheral motor conduction times. Muscle Nerve 51:706–712
Livingston SC, Friedlander DL, Gibson BC, Melvin JR (2013) Motor evoked potential response latencies demonstrate moderate correlations with height and limb length in healthy young adults. Neurodiagn J 53:63–78
Schirmer CM, Shils JL, Arle JE, Cosgrove GR, Dempsey PK, Tarlov E, Kim S, Martin CJ, Feltz C, Moul M, Magge S (2011) Heuristic map of myotomal innervation in humans using direct intraoperative nerve root stimulation. J Neurosurg Spine 15:64–70
Phillips LH, Park TS (1991) Electrophysiologic mapping of the segmental anatomy of the muscles of the lower extremity. Muscle Nerve 14:1213–1218
Chotigavanich C, Sawangnatra S (1992) Anomalies of the lumbosacral nerve roots. An anatomic investigation. Clin Orthop Relat Res 278:46–50
Foerster O (1933) The dermatomes in man. Brain 56:1–39
Thage O (1965) The myotomes L2-S2 in man. Acta Neurol Scand 13:241–243
Tsao BE, Levin KH, Bodner RA (2003) Comparison of surgical and electrodiagnostic findings in single root lumbosacral radiculopathies. Muscle Nerve 27:60–64
Seçil Y, Ekinci AS, Bayram KB, Incesu TK, Tokuçoğlu F, Gürgör N, Özdemirkıran T, Başoğlu M, Ertekin C (2012) Diagnostic value of cauda equina motor conduction time in lumbar spinal stenosis. Clin Neurophysiol 123:1831–1835
Iwasaki H, Yoshida M, Yamada H, Hashizume H, Minamide A, Nakagawa Y, Kawai M, Tsutsui S (2014) A new electrophysiological method for the diagnosis of extraforaminal stenosis at L5–S1. Asian Spine J 8:145–149
Eversmann WW Jr, Ritsick JA (1978) Intraoperative changes in motor nerve conduction latency in carpal tunnel syndrome. J Hand Surg Am 3:77–81
Rotman MB, Enkvetchakul BV, Megerian JT, Gozani SN (2004) Time course and predictors of median nerve conduction after carpal tunnel release. J Hand Surg Am 29:367–372
Kavanaugh GJ, Svien HJ, Holman CB, Johnson RM (1968) “Pseudoclaudication” syndrome produced by compression of the cauda equina. JAMA 206:2477–2481
Kobayashi S, Yoshizawa H, Hachiya Y, Ukai T, Morita T (1993) Vasogenic edema induced by compression injury to the spinal nerve root. Distribution of intravenously injected protein tracers and gadolinium-enhanced magnetic resonance imaging. Spine 18:1410–1424
Jinkins JR (1993) Gd-DTPA enhanced MR of the lumbar spinal canal in patients with claudication. J Comput Assist Tomogr 17:555–562
Watanabe R, Parke WW (1986) Vascular and neural pathology of lumbosacral spinal stenosis. J Neurosurg 64:64–70
Kunogi J, Hasue M (1991) Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine 16:1312–1320
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
No funds were received in support of this work. No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Murohashi, T., Yoshimoto, M., Takebayashi, T. et al. Efficacy of intraoperative direct electrical stimulation of the spinal root and measurement of distal motor latency in lumbar spinal stenosis. Eur Spine J 26, 434–440 (2017). https://doi.org/10.1007/s00586-016-4772-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4772-1