Abstract
Purpose
Adult spinal deformity (ASD) may be classified as idiopathic (ID) or degenerative (DD) (or other) based on classifier’s perception, the reliability of and factors inherent to which remain unknown. The aim of this study is to evaluate the inter- and intra-observer reliability of surgeons’ perception in differentiating ID from DD and to identify the determinants of this differentiation.
Methods
From a multicentric prospective database of ASD, 179 patients were identified with the diagnosis of ID (n = 103) or DD (n = 76); without previous surgery; and a lumbar coronal curve larger than 20°. Standing antero-posterior and lateral X-rays of these patients were sent to five experienced spine surgeons to be identified as DD or ID (or other); followed by a second round after reshuffling. Weighted kappa statistics were used, the strength of agreement for the kappa coefficient was considered as; 0.81–1 = almost perfect, 0.61–0.8 = substantial, 0.41–0.60 = moderate, 0.21–0.40 = fair, 0.01–0.20 = slight, and ≤0 = poor. Patients were then stratified based on the number of agreements on a total of 10 rounds as excellent (10 out of 10), good (more than 7 out of 10) and fair/poor (7 and less). These excellent and good agreements were further compared for additional radiological parameters.
Results
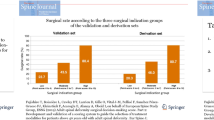
Agreement levels were moderate to substantial for intra but mostly fair for inter-observer comparisons. For ID patients, there were 42 cases with excellent and 38 with very good agreement whereas for DD, there were no excellent and only 17 cases with very good agreement. Upon comparison of these (ID vs DD for at least very good cases), it was seen that they were different for some coronal parameters such as lumbar Cobb angle (larger in ID, p < 0.001), central sacral vertical line (CSVL) modifier (C more common in ID, p = 0.007) and presence of rotatory subluxation (less common in DD, p = 0.017), but very different for sagittal parameters (lumbar lordosis, sagittal vertical axis, T2 sagittal tilt, pelvic tilt, sacral slope, and global tilt; increased sagittal imbalance in DD, all p ≤ 0.001).
Conclusion
Surgeons in this study demonstrated reasonable (moderate to substantial) intra-observer agreement, but only fair agreement amongst them. Alarming as it may appear, we should be cautious in interpreting these results based on only radiology and no clinical information. In patients with good agreement, the most consistent radiologic determinant of degenerative ASD appeared to be the presence of sagittal imbalance.


Similar content being viewed by others
References
Bradford DS, Tay BK, Hu SS (1999) Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine (Phila Pa 1976) 24:2617–2629
Silva FE, Lenke LG (2010) Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 28:E1
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis research society—Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37(12):1077–1082
Lowe T, Berven SH, Schwab FJ, Bridwell KH (2006) The SRS classification for adult spinal deformity: building on the King/Moe and Lenke classification systems. Spine (Phila Pa 1976) 31:S119–S125
Aebi M (2005) The adult scoliosis. Eur Spine J 14:925–948
Terran J, Schwab F, Shaffrey CI, Smith JS, Devos P, Ames CP et al (2013) The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery 73:559–568
Liu Y, Liu Z, Zhu F, Qian B, Zhu Z, Xu L et al (2013) Validation and reliability analysis of the new SRS-Schwab classification for adult spinal deformity. Spine (Phila Pa 1976) 38:902–908
Schwab F, Farcy JP, Bridwell K, Berven S, Glassman S, Harrast J et al (2006) A clinical impact classification of scoliosis in the adult. Spine (Phila Pa 1976) 31:2109–2114
Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP et al (2013) Change in classification grade by the SRS-Schwab adult spinal deformity classification predicts impact on health-related quality of life measures: prospective analysis of operative and non-operative treatment. Spine (Phila Pa 1976) 38:1663–1671
Acaroglu E, Dede O, Pellise F, Guler UO, Domingo-Sabat M, Alanay A, Perez-Grueso FS, European Spine Study Group (2015). Adult spinal deformity: a very heterogeneous population of patients with different needs. Acta Orthop Trauma Turc (in print)
Acaroglu E, Guler UO, Olgun ZD, Yavuz Y, Pellise F, Domingo-Sabat M, Yakici S, Alanay A, Perez-Grueso FS, Yavuz Y, European Spine Study Group (2015). Multiple regression analysis of factors affecting HRQL in adult spinal deformity (ASD). Spine Deform (in print)
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Boissiere L, Obeid I, Vital JM, Kleinstück F, Pellise F, Perez-Grueso FJS, Alanay A, Acaroglu E, European Spine Study Group (2014) Global tilt: a single parameter incorporating the spinal and pelvic sagittal parameters and least affected by patient positioning. Eur Spine J 23(Suppl 5):469–496
Vila-Casademunt A, Pellisé F, Acaroglu E, Sánchez Pérez-Grueso FJ, Pérez Martín-Buitrago M, Sanli T, Yakici S, de Frutos AG, Matamalas A, Sánchez-Márquez JM, Obeid I, Yaman O, Bagó J; ESSG, European Spine Study Group. (2014) The reliability of sagittal pelvic parameters: the effect of lumbosacral ınstrumentation and measurement experience. Spine (Phila Pa 1976). PubMed PMID: 25494319 (Epub ahead of print)
Dimar JR, Carreon LY, Labelle H, Djurasovic M, Weidenbaum M, Brown C, Roussouly P (2008) Intra- and inter-observer reliability of determining radiographic sagittal parameters of the spine and pelvis using a manual and a computer-assisted methods. Eur Spine J 17(10):1373–1379
Marty-Poumarat C, Scattin L, Marpeau M, Garreau de Loubresse C, Aegerter P (2007) Natural history of progressive adult scoliosis. Spine 32(11):1227–1234 (PubMed PMID: 17495780)
Yang C, Yang M, Chen Y, Wei X, Ni H, Chen Z, Li J, Bai Y, Zhu X, Li M (2015) Radiographic parameters in adult degenerative scoliosis and different parameters between sagittal balanced and imbalanced ADS patients. Medicine (Baltimore) 94(29):e1198. doi:10.1097/MD.0000000000001198 (PubMed PMID: 26200633; PubMed Central PMCID: PMC4603005)
Acknowledgement
This study as well as the European Spine Study Group is sponsored by a research grant from Depuy Synthes.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests to declare.
Rights and permissions
About this article
Cite this article
Guler, U.O., Yuksel, S., Yakici, S. et al. Analysis of the reliability of surgeons’ ability to differentiate between idiopathic and degenerative spinal deformity in adults radiologically. What descriptive parameters help them decide?. Eur Spine J 25, 2401–2407 (2016). https://doi.org/10.1007/s00586-015-4366-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4366-3