Abstract
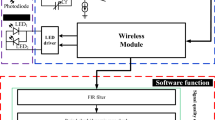
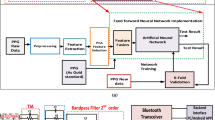
A high-order filter as part of an analog front-end circuit for an optical, cuffless photoplethysmography (PPG) sensor is developed herein to maximize the sensing accuracy of measured blood pressures (BPs). The BP device consists physically of light emitting diodes and photo-diodes (PDs) to sense the dynamic change of intravascular blood volume based on the known principle of PPG and then calculate the BP based on reflective pule transient time in a PPG signal. The photoplethysmography (PPG) signal acquired by the PDs are expected to be processed by an excellent front-end circuitry to reduce its noise and DC offset but without much distortion to obtain accurate BP prediction. This front-end is accomplished herein by a transimpedance amplifier, a critical high-order band-pass filter and a programmable gain amplifier, which is followed by microprocessor and a wireless module. The band-pass filter is optimized with a passband from 0.2 to 7.2 Hz, where the low-pass is in a 4th order while the high-pass is in 2nd order. The low-pass is designed for reducing noise including those due to ambient lighting, while the high-pass is for reducing DC drifting caused mainly by breathing and/or subject slow motion. 46 subjects were tested with the designed high-order filters in comparison with reference device. The advantages of employing high-order low-pass filter versus first-order is clearly seen in experimental data with an accuracy on predicting BP reaching ±3 mmHg, as stopped to ±7 mmHg using commonly used first-order filters.















Similar content being viewed by others
References
Ahmad S, Bolic M, Dajani H, Groza V, Batkin I, Rajan S (2010a) Measurement of heart rate variability using an oscillometric blood pressure monitor. IEEE Trans Instrum Meas 59(10):2575–2590
Ahmad S, Chen S, Souerdan K, Batkin I, Bolic M, Dajani H et al. (2010b) A prototype of an integrated blood pressure and electrocardiogram device for multi-parameter physiologic monitoring. In: Proceedings of IEEE conference on instrumentation measurement technology, pp 1244–1249
American National Standard for Electronic or Automated Sphygmomanometers, ANSI/AAMI SP 10 2002, Association for the Advancement Instrumentation, Arlington, 2002
Bramwell JC, Hill AV (1922) The velocity of the pulse wave in man. Proc R Soc Lond B 93(652):298–306
Ding XR, Zhang YT, Liu J, Dai WX, Tsang HK (2016) Continuous cuffless blood pressure estimation using pulse transit time and photoplethysmogram intensity ratio. IEEE Trans Biomed Eng 63(5):964–972
Dupuis P, Eugene C (2000) Combined detection of respiratory and cardiac rhythm disorders by high-resolution differential cuff pressure measurement. IEEE Trans Instrum Meas 49(3):498–502
Gao M, Olivier NB, Mukkamala R (2016) Comparison of noninvasive pulse transit time estimates as markers of blood pressure using invasive pulse transit time measurements as a reference. Physiol Rep. https://doi.org/10.14814/phy2.12768
Geddes LA, Voelz MH, Babbs CF, Bourland JD, Tacker WA (1981) Pulse transit time as an indicator of arterial blood pressure. Psychophysiology 18:71–74
He X, Goubran RA, Liu XP (2014) Secondary peak detection of PPG signal for continuous cuffless arterial blood pressure measurement. IEEE Trans Instrum Meas 63(6):1431–1439
Huang F, Lin K, Gao F, Chen C, Shao H, Wang B (2015) A 1.2-V 7.2-μw ECG AFE with continuous time self-calibration filters. In: IEEE 11th international conference on ASIC (ASICON), pp 1–4
Hughes DJ, Babbs CF, Geddes LA, Bourland JD (1979) Measurements of Young’s modulus of elasticity of the canine aorta with ultrasound. Ultrason Imaging 1(4):356–367
IEEE Standards Association (2014) IEEE standard for wearable cuffless blood pressure measuring devices. IEEE Standard 1708–2014, pp 1–38
Kachuee M, Kiani MM, Mohammadzade H, Shabany M (2017) Cuffless blood pressure estimation algorithms for continuous health-care monitoring. IEEE Trans Biomed Eng 64(4):859–869
Kaniusas E, Pfutzner H, Mehnen L, Kosel J, Tellez-Blanco C, Varoneckas G, Alonderis A, Meydan T, Vazquez M, Rohn M, Merlo AM, Marquardt B (2006) Method for continuous nondisturbing monitoring of blood pressure by magnetoelastic skin curvature sensor and ECG. IEEE Sens J 6(3):819–828
Kao YH, Tu TY, Chao PCP, Lee YP, Wey CL (2016) Optimizing a new cuffless blood pressure sensor via a solid-fluid-electric finite element modelling with consideration of varied mis-positionings. J Microsyst Technol 22:1437–1447
Kurylyak Y, Lamonaca F, Grimaldi D (2013) A Neural Network-based method for continuous blood pressure estimation from a PPG signal. In: International conference of the IEEE in instrumentation and measurement technology, pp 280–283
Lee SY, Cheng CJ (2009) Systematic design and modeling of a OTA-C filter for portable ECG detection. IEEE Trans Biomed Circuits Syst 3(1):53–64
Lin WQ, Wu HH, Su CS, Yang JT, Xiao JR, Cai YP, Chen GZ (2017) Comparison of continuous noninvasive blood pressure monitoring by TL-300 with standard invasive blood pressure measurement in patients undergoing elective neurosurgery. J Neurosurg Anesthesiol 29(1):1–7
Mahmoud SA, Bamakhramah A, Al-Tunaiji SA (2014) Six order cascaded power line notch filter for ECG detection systems with noise shaping. Circuits Syst Signal Process 33(8):2385–2400
Martin SLO, Carek AM, Kim CS, Ashouri H, Inan OT, Hahn JO, Mukkamala R (2016) Weighing scale-based pulse transit time is a superior marker of blood pressure than conventional pulse arrival time. Sci Rep 6:39273
Miao F, Fu N, Zhang YT, Ding XR, Hong X, He Q, Li Y (2017) A novel continuous blood pressure estimation approach based on data mining techniques. IEEE J Biomed Health Inform 21(6):1730–1740
Miyauchi Y, Koyama S, Ishizawa H (2013) Basic experiment of blood pressure measurement which uses FBG sensors. In: Proceedings of IEEE international conference instrumentation measurement, pp 1767–1770
O’brien E, Petrie J, Littler W, de Swiet M, Padfield PL, O’malley K, Atkins N (1990) The British Hypertension Society protocol for the evaluation of automated and semi-automated blood pressure measuring devices with special reference to ambulatory systems. J Hypertens 8:607–619
Okumura M, Tanimoto H, Itakura T, Sugawara T (1993) Numerical noise analysis for nonlinear circuits with a periodic large signal excitation including cyclostationary noise sources. IEEE Trans Circuits Syst I: Fundam Theory and Appl 40(9):581–590
Pinheiro E, Postolache O, Girao P (2009) Pulse arrival time and ballistocardiogram application to blood pressure variability estimation. In: Proceedings of the IEEE international workshop on medical measurement and applications, pp 132–136
Poon C, Zhang Y (2006) Cuff-less and noninvasive measurements of arterial blood pressure by pulse transit time. In: 2005 IEEE engineering in medicine and biology 27th annual conference, pp 5877–5880
Rybynok VO, Kyriacou PA (2010) Beer-lambert law along non-linear mean light pathways for the rational analysis of photoplethysmography. J Phys Conf Ser 238(1):012061
Sharma M, Barbosa K, Ho V, Griggs D, Ghirmai T, Krishnan SK, Cao H (2017) Cuff-less and continuous blood pressure monitoring: a methodological review. Technologies 5(2):21
Shin H, Min SD (2017) Feasibility study for the non-invasive blood pressure estimation based on ppg morphology: normotensive subject study. Biomed Eng Online 16(1):10
Silvani A, Grimaldi D, Vandi S, Barletta G, Vetrugno R, Provini F et al (2008) Sleep-dependent changes in the coupling between heart period and blood pressure in human subjects. Am J Physiol Regul Integr Comp Physiol 294:1686–1692
Suzuki S, Oguri K (2008) Cuffless and non-invasive systolic blood pressure estimation for aged class by using a photoplethysmograph. In: Proceedings of the 30th annual international conference of the IEEE in engineering in medicine and biology society, pp 1327–1330
Teng XF, Zhang YT (2003) Continuous and noninvasive estimation of arterial blood pressure using a photoplethysmographic approach. In: Proceedings of the 25th annual international conference of the IEEE in engineering in medicine and biology society, vol 4, pp 3153–3156
Tu TY, Chao PCP, Lee YP (2013) A new non-invasive cuff-less blood pressure sensor. In: 2013 IEEE Sensors in Baltimore, MD, pp 1–4
Tu TY, Kao YH, Chao PC, Lee YP (2014) Optimizing a new blood pressure sensor for maximum performance based on finite element model. In: Conference on IEEE sensors, Valencia, Spain, pp 1873–1876
WHO (2015a) Cardiovascular diseases (CVDs). WHO, Geneva
WHO (2015b) World health statistic 2015. World Health Organization, Geneva
Xing X, Sun M (2016) Optical blood pressure estimation with photoplethysmography and FFT-based neural networks. Biomed Opt Express 7(8):3007–3020
Yoon YZ, Kang JM, Kwon Y, Park S, Noh S, Kim Y, Park J, Hwang SW (2017) Cuff-less blood pressure estimation using pulse waveform analysis and pulse arrival time. IEEE J Biomed Health Inform PP(99):1
Acknowledgement
This work was supported in part by the Novel Bioengineering and Technological Approaches to Solve Two Major Health Problems in Taiwan sponsored by the Taiwan Ministry of Science and Technology Academic Excellence Program under Grant Number: MOST 106-2633-B-009-001 and 107-2633-B-009-003. The authors appreciate the supports from MOST 106-2221-E-009 -089, 106-2218-E-009 -011 and Chunwha Prcture Tubes, Ltd.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kao, YH., Chao, P.CP. & Wey, CL. Towards maximizing the sensing accuracy of an cuffless, optical blood pressure sensor using a high-order front-end filter. Microsyst Technol 24, 4621–4630 (2018). https://doi.org/10.1007/s00542-018-3877-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00542-018-3877-3