Abstract
For point-of-care diagnosis of influenza A (H1N1) virus, a convection polymerase chain reaction (PCR) in a capillary tube is developed for rapid nucleic acid amplification with a simple heating scheme. When the capillary tube is heated from the bottom end with a constant temperature, a stable temperature gradient across the tube generates a continuous circulatory flow which spontaneously transports the reagent through different temperature zones associated with the denaturing, annealing, and extension stages of PCR. A resistive heater, which is powered by a 5 V power supply, is used for heating the capillary tube. For real-time detection, Taqman probes labeled with FAM (Carboxyfluorescein) are used in amplification. A light-emitting diode positioned on the top of the capillary tube is used to shine the reagent for excitation. Real-time fluorescence detection is obtained with a smartphone whose camera is used to take the fluorescent images. A custom algorithm running on the smartphone is developed with Java for the analysis of images to interpret the detection result. The low cost and small device can be powered with a portable mobile power supply. In less than 30 min, H1N1 virus can be successfully detected with a reasonable detection limit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Influenza A (H1N1) virus, a subtype of influenza A virus, is one of the most common causes of human influenza (Kong et al. 2015). Influenza A virus is an orthomyxoviruse that contains the glycoproteins haemagglutinin and neuraminidase. Accordingly, influenza A viruses are described as H1N1, H1N2 etc. depending on the type of H or N antigens they express with metabolic synergy. Haemagglutinin causes red blood cells to clump together and binds the virus to the infected cells. Neuraminidase is a type of glycoside hydrolase enzyme which helps to move the virus particles through the infected cells, as well as to assist in budding from the host cells (Lamb and Choppin 1983). Some strains of H1N1 are endemic in humans and cause influenza-like illness, for example, serious human flu infections with H1N1 in the world (Lessler et al. 2009; Tharakaraman and Sasisekharan 2015).
As a critical tool for molecule diagnosis, PCR is able to amplify the DNA or RNA templates to a large quantity with millions of copies after up to 30–40 amplification cycles consisting of denaturation, annealing, and extension of three stages regulated by thermal cycling. H1N1 diagnosis based on PCR is widely adopted because of its high sensitivity, accuracy and specificity (Takayama et al. 2013). It is anticipated that microfluidic technology potentially is able to move conventional instrument PCR from the centralized labs with highly trained staff to places with poor medical resource by using smart microfluidic PCR systems (Zhang et al. 2007; Tian et al. 2015). Especially for point-of-care test, microfluidic PCR offers reasonable solutions to integrate and automate the analysis process, shorten the analysis time, reduce the device size and lower the diagnostics cost (Norian et al. 2014; Chen et al. 2010). For example, an integrated microfluidic device was developed for influenza and other genetic analyses with PCR in point-of-care settings (Pal et al. 2005).
Microfluidic PCR performed in a small reaction chamber is normally heated by a complicated thermal cycler that provides repeated temperatures respectively for different reaction stages with typical 30 cycles (Bian et al. 2015). When the microfluidic PCR chip is made from polymeric material, such as polycarbonate (PC), polymethyl methacrylate (PMMA), or cyclic olefin copolymer (COC), it is difficult to shorten the transition time between different reaction stages as well as the dwelling time for each of them especially when the chamber size is relatively large, e.g., 10–50 μl (Qiu et al. 2010).
One special format of microfluidic PCR in a pseudo-isothermal manner, convection PCR, provides a promising solution for rapid nucleic acid analysis with significantly simplified heating device and remarkably shortened amplification time (Krishnan et al. 2002; Chen et al. 2004). When heated from the bottom end with a constant temperature, a stable temperature gradient across the capillary reactor will generate a continuous circulatory flow which spontaneously and repeatedly transports the reagent through different temperature zones associated with the denaturing, annealing, and extension stages of PCR (Chang et al. 2012; Chung et al. 2010; Li et al. 2016; Priye et al. 2012).
To successfully detect H1N1 in a short time with high convenience, low cost and remarkable easiness, here we report for the first time a portable, low cost and easy-to-use system for the rapid detection of H1N1 based on the convection PCR using a smartphone accessory for point-of-care diagnostics. Custom capillary tubes are developed and fabricated with injection molding for convection PCR amplification. To simplify the detection procedure and shorten the total test time, real-time in situ fluorescence monitor of the reaction is performed with a smartphone camera, and meanwhile a custom image processing algorithm running on the smartphone is developed to analyze the fluorescence signal intensity of collected images. A resistive heater, which is powered by a DC voltage, is used to heat the capillary tube from the bottom end with a constant temperature. With low power consumption, the device can be powered with a portable mobile power supply. Influenza A (H1N1) virus nucleic acid targets are successfully detected by the system with a limit of detection (LOD) of 1.0 TCID50/mL in less than 30 min.
2 Microfluidic convection PCR system
2.1 Microfluidic convection PCR reactor
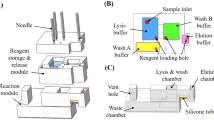
For point-of-care diagnosis of H1N1, it is desirable to conveniently implement convection PCR in a low cost, single-use (disposable) microfluidic chip reactor. Because of the features with mass fabrication, biocompatibility, optical transparency, and low autofluorescence, polymeric material-based reactors are the first choice for convection PCR (Chin et al. 2012; Qiu and Mauk 2015). Here, custom capillary tubes with excellent smoothness and transparency, which are made from optical-quality polycarbonate by injection molding, are used for amplification, as shown in Fig. 1. Similar to typical PCR tubes, the capillary tube can be handled with easiness and convenience on positioning and alignment. The capillary tube consists of a head for reagent loading and a capillary reaction chamber (~40 μl) with outside/inside diameters of 3.3 mm/1.7 mm, and length of 19 mm.
2.2 Heating module with a resistive heater
A resistive heater, which is powered by a DC voltage of 5 V, is used to heat the capillary tube from the bottom end with a constant temperature. As shown in Fig. 2, the bottom section of the capillary tube is surrounded by an aluminum block whose interior side is attached with a rubberized resistive heater. The length of the capillary tube immersed within the heating block is 7.5 mm.
An open-loop control strategy with low cost is adopted to maintain the reaction temperature by applying a properly set voltage to the resistive heater. Because of low power consumption, the resistive heater can be powered by a portable mobile power supply. Comparing to traditional PCR performed in complicated thermal cyclers, convection PCR can be much more conveniently performed with significantly simplified heating scheme in the point-of-care settings.
2.3 Fluorescence detection with a smartphone accessory
A smartphone is used for the real-time detection of fluorescence signal of reagent with its own camera. A LED excitation source positioned on the top of the capillary tube is used to shine the reagent through a short pass optical filter when the light passes through the capillary tube from top to bottom. As shown in Fig. 3, the fluorescent image of the reagent inside the capillary tube is taken by a smartphone camera after it is coupled through an optical filter (to block the excitation). To just demonstrate the principle of smartphone based detection, a simplified schematic illustration without the heating block is shown in Fig. 3.
The flash light source of the smartphone is not used because it shines the capillary tube from the side wall and part of light will be refracted by the tube. With a LED excitation source on the top of the capillary tube, the reagent is shined with enough efficiency, which helps the fluorescence detection. In the process of amplification, a custom program running on the smartphone controls the camera to take fluorescent images of the reagent according to a predefined time interval. The fluorescent images are further processed by a custom image analysis algorithm running on the same smartphone to determine the detection result.
2.4 Digital fluorescent image analysis
A custom Java program running on the smartphone was developed to analyze the collected images of the capillary tube to extract the fluorescence signal intensity of convection PCR reaction. First, the four boundaries of the convection PCR reaction inside the capillary tube are recognized. Based on the geometry characteristics of the reaction region of the capillary tube, four different geometry-specific patterns are constructed to respectively identify four boundaries of the rectangle reaction area. Because the convection PCR reaction in the capillary tube exhibits green fluorescence surrounded by the black background, the purpose of the geometry-specific patterns is to find out the most significant boundaries between the green fluorescent reaction area and the black background. Second, the average grey value of the recognized convection PCR reaction area within the four boundaries is obtained to represent the relative fluorescence signal intensity after it is subtracted by the average grey value of the background.
2.5 Instrumentation
Different components, including a smartphone, a heating module, a LED, and optical accessories, are fixed inside or outside a portable instrument box fabricated with the 3D printing technology. As shown in Fig. 4, on the side wall of the instrument (130 × 95 × 160 mm), a smartphone, which works as a multifunctional module for fluorescent image collection and analysis, and user interfacing, is fixed from the outside for user operation by providing friendly graphical interface.
As shown in Fig. 4, a portable mobile power supply can be used to provide +5 V DC power for continuously heating the capillary tube. From the amplitude of the sustaining current of the DC voltage to maintain the desirable heating temperature, it can be estimated that more than 100 convection PCR runs can be performed when the capacity of the mobile power supply is around 20,000 mAh.
3 Results and discussion
3.1 Assessment of capillary tube heating with a resistive heater
To evaluate the performance of heating the capillary tube with a resistive heater, we constructed a calibration capillary tube equipped with a 0.76 mm diameter thermistor at the bottom end of the capillary reactor. The calibration capillary tube was inserted into the heating position and held tightly by the bottom heating part (Fig. 2), and the temperature sensor was connected to a standard temperature recording device. The experiments were carried out at room temperature of 23 °C. The heating voltage applied to the resistive heater was adjusted through a potentiometer until the temperature readings of the calibration capillary tube stayed at around 95 °C. The actual working voltage was 3.1 V with a sustaining current of 380 mA. The thermal time-response of the open-loop system was tested in a separate set of experiments. Figure 5 depicts the temperature readings from the inside thermistor of the calibration capillary tube when it was heated from the room temperature until stayed at 95 °C for 30 min.
As shown in Fig. 5, the average ramping rate is approximately 0.12 °C/s. With the open-loop control scheme, the steady-state temperature inside the calibration capillary tube was maintained within the range of 94.6–95.7 °C for more than 30 min, which is allowable for convection PCR amplification.
3.2 Detection of H1N1 with convection PCR
A magnetic beads-based RNA blood kit (Beijing Wantai Biological Pharmacy Enterprise Co., Ltd.) was used for RNA extraction from 200 μL aliquots of influenza A (H1N1) virus sample. The viral samples (200 μL) were tenfold serially diluted from influenza A (H1N1) virus culture stock (1000–1.0 TCID50/ml) using a semi-automated instrument (Taiwan Nanotechnology Corp., SLA-32). Currently, for H1N1 clinical test, limit of detection (LOD) of commercial kits with 1.0 TCID50/mL, or even higher value of 101.29 TCID50/ml (Influenza A virus real-time kit, Guangzhou Huayin Medicine Science Limited) is allowable.
The convection PCR reaction mix was comprised of 3 μL mixture (Takara Bio Inc.) of primers and TaqMan probes labeled with FAM at the 5′ end and Eclipse at the 3′ end, 4 mM dNTP (Takara Bio Inc., Shiga, Japan), 4 μL 10 × Fast Buffer I (Mg2+ plus), 0.4 U of AMV Reverse Transcriptase (Promega, USA), 1 U of SpeedSTAR HS DNA polymerase (Takara Bio Inc.), 10 μL influenza A (H1N1) virus RNA templates and molecular-biology grade water, which is totally 40 μL. The convection PCR components were prepared and mixed on the benchtop and then loaded into the capillary tube reactor before being covered with 10 μL sterile mineral oil (Sigma-Aldrich, St. Louis, MO, USA). It is proved that the sterile mineral oil will not affect the excitation of reagent from the top of the capillary tube with a LED. Influenza A (H1N1) virus amplification with convection PCR yielded a 105-bp amplicon. Together with CPCR amplification, reverse transcription of H1N1 RNA templates is completed within the same instrument. The reaction was monitored in real-time through the smartphone accessory located on the outside wall of the instrument box.
Beside positive samples, no-template (negative) controls were also run in the capillary tubes to ensure the absence of false positives. The experiments were repeated multiple times with similar results. As an example, Fig. 6 depicts real-time convection PCR with influenza A (H1N1) virus RNA template (1.0 TCID50/mL). Similar results were obtained with higher concentrations of H1N1 viruses. The fluorescent signal image of the reagent inside the capillary tube was recorded in real-time by the smartphone camera with a time interval of 30 s, and the relative fluorescent signal intensity for each image was analyze by the custom digital image processing algorithm running on the same smartphone.
Real-time convection PCR with influenza A (H1N1) virus RNA template (1.0 TCID50/mL). a Fluorescence images at amplification time of 0 min (a), 4 min (b), 8 min (c), 12 min (d), 16 min (e), 20 min (f), 24 min (g), 26 min (h), 28 min (i), and 30 min (j). b Fluorescence signal intensity as a function of time
In Fig. 6a, in the presence of influenza A (H1N1) virus RNA with concentration of 1.0 TCID50/mL, the fluorescent signal intensity inside the capillary tube increased with the elapsed amplification time. In Fig. 6b, a real-time curve was constructed by extracting the fluorescent signal intensity inside the capillary tube from each fluorescence image taken in sequence, which confirmed that H1N1 RNA sample (1.0 TCID50/mL) has been amplified successfully.
It can be concluded that with a simple and concise bottom-end heating mode, H1N1 detection based on convective PCR can be performed successfully within 30 min with reasonable sensitivity. A potential issue for bottom-end heating mode is that the convection amplification will probably be affected by environmental temperature fluctuation. A smartphone accessory is able to further simplify the process of detection and data analysis of H1N1 detection with its own camera and controller. Because for convection PCR, the reagent repeatedly undergoes the three PCR temperature zones with un-recordable cycles based on its convection characteristics, only qualitative detection of H1N1 can be provided at this stage.
4 Conclusions
We described here for the first time a rapid nucleic acid based detection method for H1N1 by microfluidic convection real-time PCR with a smartphone accessory. A simple and easy to use capillary tube, which works as the microfluidic convection PCR reactor, is developed and fabricated with injection molding. A concise, low cost, and open-loop heating scheme is adopted to heat the capillary tube with a resistive heater from the bottom end with a constant temperature. Together with CPCR amplification, reverse transcription of H1N1 RNA templates is completed within the same instrument. Real-time fluorescence monitoring of the reaction is assisted by a smartphone accessory. A smartphone camera is used to take the fluorescent images of the reagent when it is excited by a LED from the top of the capillary tube. To obtain the fluorescent signal intensity of the collected images, each of them is further analyzed by a custom digital image processing algorithm running on the smartphone. The smartphone also provides a graphic user interface for instrument’s operation. Influenza A (H1N1) virus with the concentration of 1.0 TCID50/mL can be successfully detected in 30 min with the portable convection PCR instrument. Comparing to typical real-time PCR, H1N1 detection could be performed in significantly shorter time with lower cost with the microfluidic convection real-time PCR assisted by a smartphone accessory in point-of-care settings.
References
Bian X, Jing F, Li G, Fan X, Jia C, Zhou H, Jin Q, Zhao J (2015) A microfluidic droplet digital PCR for simultaneous detection of pathogenic Escherichia coli O157 and Listeria monocytogenes. Biosens Bioelectron 74:770–777
Chang HG, Tsai Y, Tsai C, Lin C, Lee P, Teng P, Su C, Jeng C (2012) A thermally baffled device for highly stabilized convective PCR. Biotechnol J 7:662–666
Chen Z, Qian S, Abrams WR, Malamud D, Bau HH (2004) Thermosiphon-based PCR reactor: experiment and modeling. Anal Chem 76:3707–3715
Chen D, Mauk MG, Qiu X, Liu C, Kim J, Ramprasad S, Ongagna S, Abrams WR, Malamud D, Corstjens PLAM, Bau HH (2010) An integrated, self-contained microfluidic cassette for isolation, amplification, and detection of nucleic acid. Biomed Microdevices 12:705–719
Chin CD, Linder V, Sia SK (2012) Commercialization of microfluidic point-of-care diagnostic devices. Lab Chip 12:2118–2134
Chung KH, Park SH, Choi YH (2010) A palmtop PCR system with a disposable polymer chip operated by the thermosiphon effect. Lab Chip 10:202–210
Kong W, Wang F, Dong B, Ou C, Meng D, Liu J, Fan Z (2015) Novel reassortant influenza viruses between pandemic (H1N1) 2009 and other influenza viruses pose a risk to public health. Microb Pathog 89:62–72
Krishnan M, Victor MU, Burns MA (2002) PCR in a Rayleigh-Benard convection cell. Science 298:793
Lamb RA, Choppin PW (1983) The gene structure and replication of influenza virus. Annu Rev Biochem 52:467–506
Lessler J, Reich NG, Cummings DA (2009) New York City Department of Health and Mental Hygiene Swine Influenza Investigation Team, H. P. Nair, H. T. Jordan. N Engl J Med 27:2628–2636
Li Z, Zhao Y, Zhang D, Zhuang S, Yamaguchi Y (2016) The development of a portable buoyancy-driven PCR system and its evaluation by capillary electrophoresis. Sens Actuators B Chem 230:779–784
Norian H, Field RM, Kymissis I, Shepard K (2014) An integrated CMOS quantitative-polymerasechain-reaction lab-on-chip for point-of-care diagnostics. Lab Chip 14:4076–4084
Pal R, Yang M, Lin R, Johnson BN, Srivastava N, Razzacki SZ, Chomistek KJ, Heldsinger DC, Haque RM, Ugaz VM, Thwar PK, Chen Z, Alfano K, Yim MB, Krishnan M, Fuller AO, Larson RG, Burked DT, Burns MA (2005) An integrated microfluidic device for influenza and other genetic analyses. Lab Chip 5:1024–1032
Priye A, Hassanbc YA, Ugaz VM (2012) Education: DNA replication using microscale natural convection. Lab Chip 12:4946–4954
Qiu X, Mauk MG (2015) An integrated, cellulose membrane-based PCR chamber. Microsyst Technol 21:841–850
Qiu X, Mauk MG, Chen D, Liu C, Bau HH (2010) A large volume, portable, real-time PCR reactor. Lab Chip 10:3170–3177
Takayama I, Nakauchi M, Fujisaki S, Odagiri T, Tashiro M, Kageyama T (2013) Rapid detection of the S247N neuraminidase mutation in influenza A(H1N1) pdm09 virus by one-step duplex RT-PCR assay. J Virol Methods 188:73–75
Tharakaraman K, Sasisekharan R (2015) Influenza surveillance: 2014–2015 H1N1 “swine”-derived influenza viruses from India. Cell Host Microbe 17:279–282
Tian Q, Mu Y, Xu Y, Song Q, Yu B, Ma C, Jin W, Jin Q (2015) An integrated microfluidic system for bovine DNA purification and digital PCR detection. Anal Biochem 491:55–57
Zhang C, Da X, Hase T (2007) Miniaturized PCR chips for nucleic acid amplification and analysis: latest advances and future trends. Nucl Acids Res 13:4223–4237
Acknowledgments
The work was supported by the National Natural Science Foundation of China (No. 81371711) and the Fundamental Research Funds for the Central Universities (ZZ1329, YS1404).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Qiu, X., Ge, S., Gao, P. et al. A smartphone-based point-of-care diagnosis of H1N1 with microfluidic convection PCR. Microsyst Technol 23, 2951–2956 (2017). https://doi.org/10.1007/s00542-016-2979-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00542-016-2979-z