Abstract
Purpose
This study aimed to compare non-invasive oscillometric blood pressure (NIBP) measurement with invasive arterial blood pressure (IBP) measurement in patients with sepsis.
Methods
We conducted a retrospective study to evaluate the agreement between IBP and NIBP using the Medical Information Mart for Intensive Care IV (MIMIC-IV) database. Paired blood pressure measurements of mean arterial pressure (MAP), systolic blood pressure (SBP), and diastolic blood pressure (DBP) were compared using Bland–Altman analysis and paired Student’s t test. We also focus on the effect of norepinephrine (NE) on the agreement between the two methods and the association between blood pressure and mortality during intensive care unit (ICU) stay.
Results
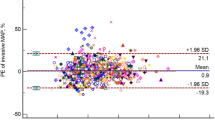
A total of 96,673 paired blood pressure measurements from 6060 unique patients were analyzed in the study. In Bland–Altman analysis, the bias (± SD, 95% limits of agreement) was 6.21 mmHg (± 12.05 mmHg, − 17.41 to 29.83 mmHg) for MAP, 0.39 mmHg (± 19.25 mmHg, − 37.34 to 38.12 mmHg) for SBP, and 0.80 mmHg (± 12.92 mmHg, − 24.52 to 26.12 mmHg) for DBP between the two techniques. Similarly, large limits of agreement were shown in different groups of NE doses. NE doses significantly affected the agreement between IBP and NIBP. SBP between the two methods gave an inconsistent assessment of patients’ risk of ICU mortality.
Conclusion
IBP and NIBP were not interchangeable in septic patients. Clinicians should be aware that non-invasive MAP was clinically and significantly underestimated invasive MAP.



Similar content being viewed by others
Data availability
All Data was extracted from the Medical Information Mart for Intensive Care IV v1.0, a freely accessible public database constructed by the Massachusetts Institute of Technology Computational Physiology Laboratory (https://mimic.mit.edu/).
Abbreviations
- IBP:
-
Invasive arterial blood pressure
- NIBP:
-
Non-invasive oscillometric blood pressure
- NE:
-
Norepinephrine
- ICU:
-
Intensive care unit
- MIMIC-IV:
-
Medical Information Mart for Intensive Care IV
- BMI:
-
Body mass index
- SOFA:
-
Sequential Organ Failure Assessment
- SAPS II:
-
Simplified Acute Physiology Score II
- CVP:
-
Central venous pressure
- IMAP:
-
Invasive mean arterial pressure
- ISBP:
-
Invasive systolic blood pressure
- IDBP:
-
Invasive diastolic blood pressure
- NIMAP:
-
Non-invasive mean arterial pressure
- NISBP:
-
Non-invasive systolic blood pressure
- NIDBP:
-
Non-invasive diastolic blood pressure
- MAP:
-
Mean arterial pressure
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- AAMI:
-
Association for the Advancement of Medical Instrumentation
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- LOA:
-
Limits of agreement
- AKI:
-
Acute kidney injury
References
Meidert AS, Saugel B. Techniques for non-invasive monitoring of arterial blood pressure. Front Med (Lausanne). 2017;4:231. https://doi.org/10.3389/fmed.2017.00231.
Pour-Ghaz I, Manolukas T, Foray N, Raja J, Rawal A, Ibebuogu UN, Khouzam RN. Accuracy of non-invasive and minimally invasive hemodynamic monitoring: where do we stand? Ann Transl Med. 2019;7:421. https://doi.org/10.21037/atm.2019.07.06.
Lakhal K, Ehrmann S, Boulain T. Noninvasive BP monitoring in the critically Ill: time to abandon the arterial catheter? Chest. 2018;153:1023–39. https://doi.org/10.1016/j.chest.2017.10.030.
Mirdamadi A, Etebari M. Comparison of manual versus automated blood pressure measurement in intensive care unit, coronary care unit, and emergency room. ARYA Atheroscler. 2017;13:29–34.
Watson S, Aguas M, Bienapfl T, Colegrove P, Foisy N, Jondahl B, Yosses MB, Yu L, Anastas Z. Postanesthesia patients with large upper arm circumference: is use of an “extra-long” adult cuff or forearm cuff placement accurate? J Perianesth Nurs. 2011;26:135–42. https://doi.org/10.1016/j.jopan.2011.02.001.
Hromádka M, Tůmová P, Rokyta R, Seidlerová J. [Copy] Blood pressure measurement in patients with cardiogenic shock: the effect of norepinephrine. Blood Press Monit. 2019;24:213–20. https://doi.org/10.1097/MBP.0000000000000393.
Rebesco MR, Pinkston MC, Smyrnios NA, Weisberg SN. A comparison of non-invasive blood pressure measurement strategies with intra-arterial measurement. Prehosp Disaster Med. 2020;35:516–23. https://doi.org/10.1017/S1049023X20000916.
Hamzaoui O, Scheeren TWL, Teboul J-L. Norepinephrine in septic shock: when and how much? Curr Opin Crit Care. 2017;23:342–7. https://doi.org/10.1097/MCC.0000000000000418.
Lee GT, Hwang SY, Jo IJ, Kim TR, Yoon H, Park JH. Associations between mean arterial pressure and 28-day mortality according to the presence of hypertension or previous blood pressure level in critically ill sepsis patients. J Thorac Dis. 2019;11:1980–8. https://doi.org/10.21037/jtd.2019.04.108.
Kobayashi N, Nakagawa A, Kudo D, Ishigaki T, Ishizuka H, Saito K. Arterial blood pressure correlates with 90-day mortality in sepsis patients: a retrospective multicenter derivation and validation study using high-frequency continuous data. Blood Press Monit. 2019;24:225–33. https://doi.org/10.1097/MBP.0000000000000398.
Johnson A, Bulgarelli L, Pollard T, Horng S, Celi LA. Mark R. MIMIC-IV (version 1.0). PhysioNet. 2021. https://doi.org/10.13026/s6n6-xd98.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10. https://doi.org/10.1001/jama.2016.0287.
Lehman LH, Saeed M, Talmor D, Mark R, Malhotra A. Methods of blood pressure measurement in the ICU. Crit Care Med. 2013;41:34–40. https://doi.org/10.1097/CCM.0b013e318265ea46.
Kaufmann T, Cox EGM, Wiersema R, Hiemstra B, Eck RJ, Koster G. Non-invasive oscillometric versus invasive arterial blood pressure measurements in critically ill patients: a post hoc analysis of a prospective observational study. J Crit Care. 2020;57:118–23. https://doi.org/10.1016/j.jcrc.2020.02.013.
Bur A, Herkner H, Vlcek M, Woisetschläger C, Derhaschnig U, Delle Karth G. Factors influencing the accuracy of oscillometric blood pressure measurement in critically ill patients. Crit Care Med. 2003;31:793–9. https://doi.org/10.1097/01.CCM.0000053650.12025.1A.
Saherwala AA, Stutzman SE, Osman M, Kalia J, Figueroa SA, Olson DM, Aiyagari V. Correlation of noninvasive blood pressure and invasive intra-arterial blood pressure in patients treated with vasoactive medications in a neurocritical care unit. Neurocrit Care. 2018;28:265–72. https://doi.org/10.1007/s12028-018-0521-0.
Hohn A, Defosse JM, Becker S, Steffen C, Wappler F, Sakka SG. Non-invasive continuous arterial pressure monitoring with Nexfin does not sufficiently replace invasive measurements in critically ill patients. Br J Anaesth. 2013;111:178–84. https://doi.org/10.1093/bja/aet023.
Meidert AS, Dolch ME, Mühlbauer K, Zwissler B, Klein M, Briegel J, Czerner S. Oscillometric versus invasive blood pressure measurement in patients with shock: a prospective observational study in the emergency department. J Clin Monit Comput. 2021;35:387–93. https://doi.org/10.1007/s10877-020-00482-2.
Yüksel S, Altun-Uğraş G, Altınok N, Demir N. The effect of cuff size on blood pressure measurement in obese surgical patients: a prospective crossover clinical trial. Florence Nightingale J Nurs. 2020;28:205–12. https://doi.org/10.5152/FNJN.2020.19119.
Mourad J-J, Lopez-Sublet M, Aoun-Bahous S, Villeneuve F, Jaboureck O, Dourmap-Collas C. Impact of miscuffing during home blood pressure measurement on the prevalence of masked hypertension. Am J Hypertens. 2013;26:1205–9. https://doi.org/10.1093/ajh/hpt084.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49:e1063–143. https://doi.org/10.1097/CCM.0000000000005337.
Guinot P-G, Bernard E, Levrard M, Dupont H, Lorne E. Dynamic arterial elastance predicts mean arterial pressure decrease associated with decreasing norepinephrine dosage in septic shock. Crit Care. 2015;19:14. https://doi.org/10.1186/s13054-014-0732-5.
Monge García MI, Santos A, Del Diez CB, Guijo González P, Gracia Romero M, Gil Cano A, Cecconi M. Noradrenaline modifies arterial reflection phenomena and left ventricular efficiency in septic shock patients: a prospective observational study. J Crit Care. 2018;47:280–6. https://doi.org/10.1016/j.jcrc.2018.07.027.
Wittrock M, Scholze A, Compton F, Schaefer J-H, Zidek W, Tepel M. Noninvasive pulse wave analysis for the determination of central artery stiffness. Microvasc Res. 2009;77:109–12. https://doi.org/10.1016/j.mvr.2008.10.001.
Pinsky MR. Defining the boundaries of bedside pulse contour analysis: dynamic arterial elastance. Crit Care. 2011;15:120. https://doi.org/10.1186/cc9986.
Gruenewald M, Meybohm P, Renner J, Broch O, Caliebe A, Weiler N. Effect of norepinephrine dosage and calibration frequency on accuracy of pulse contour-derived cardiac output. Crit Care. 2011;15:R22. https://doi.org/10.1186/cc9967.
Laurent S, Cockcroft J, van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605. https://doi.org/10.1093/eurheartj/ehl254.
Pytte M, Dybwik K, Sexton J, Straume B, Nielsen EW. Oscillometric brachial mean artery pressures are higher than intra-radial mean artery pressures in intensive care unit patients receiving norepinephrine. Acta Anaesthesiol Scand. 2006;50:718–21. https://doi.org/10.1111/j.1399-6576.2006.01045.x.
Riley LE, Chen GJ, Latham HE. Comparison of noninvasive blood pressure monitoring with invasive arterial pressure monitoring in medical ICU patients with septic shock. Blood Press Monit. 2017;22:202–7. https://doi.org/10.1097/MBP.0000000000000258.
Ait-Oufella H, Bakker J. Understanding clinical signs of poor tissue perfusion during septic shock. Intensive Care Med. 2016;42:2070–2. https://doi.org/10.1007/s00134-016-4250-6.
Smischney NJ, Shaw AD, Stapelfeldt WH, Boero IJ, Chen Q, Stevens M, Khanna AK. Postoperative hypotension in patients discharged to the intensive care unit after non-cardiac surgery is associated with adverse clinical outcomes. Crit Care. 2020;24:682. https://doi.org/10.1186/s13054-020-03412-5.
Khanna AK, Kinoshita T, Natarajan A, Schwager E, Linn DD, Dong J. Association of systolic, diastolic, mean, and pulse pressure with morbidity and mortality in septic ICU patients: a nationwide observational study. Ann Intensive Care. 2023;13:9. https://doi.org/10.1186/s13613-023-01101-4.
Maheshwari K, Nathanson BH, Munson SH, Khangulov V, Stevens M, Badani H. The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intensive Care Med. 2018;44:857–67. https://doi.org/10.1007/s00134-018-5218-5.
Al-Husinat L, Alsabbah A, Hmaid AA, Athamneh R, Adwan M, Hourani MN. Norepinephrine may exacerbate septic acute kidney injury: a narrative review. J Clin Med. 2023. https://doi.org/10.3390/jcm12041373.
Acknowledgements
The authors express their sincere appreciation to the staff members of the Massachusetts Institute of Technology Computational Physiology Laboratory and the Beth Israel Deaconess Medical Center, who have participated in the Medical Information Mart for Intensive Care IV.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ZJ: Conceptualization, Methodology, Formal analysis, Data Curation, Writing—Original Draft. SL: Conceptualization, Methodology, Writing—Original Draft. WL: Conceptualization, Writing—Review and Editing. FY: Conceptualization, Writing—Review and Editing. YZ: Formal analysis, Writing—Original Draft. HL: Formal analysis, Writing—Original Draft. JL: Formal analysis, Writing—Original Draft. ZZ: Formal analysis, Writing—Original Draft. JLZ: Conceptualization, Methodology, Writing—Review and Editing.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there is no conflict of interest.
Ethics approval and consent to participate
The author who had finished the online training for the Collaborative Institutional Training Initiative Program can access the database (Record ID 40486481). The MIMIC-IV v1.0 contain no identifiers and are publicly available for studies of critical care. The Institutional Review Board approval and the need for informed consent was waived.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
540_2023_3304_MOESM1_ESM.pdf
Supplementary file1 Figure S1. The association between MAP and ICU mortality. Error bars show 95% confidence intervals of the mortality rates. No difference between MAP measurements in terms of their ICU mortality was observed (p>0.05) based on the chi-square test. ICU intensive care unit, MAP mean arterial pressure. (PDF 387 KB)
540_2023_3304_MOESM2_ESM.pdf
Supplementary file2 Figure S2. The association between DBP and ICU mortality. Error bars show 95% confidence intervals of the mortality rates. No difference between DBP measurements in terms of their ICU mortality was observed (p>0.05) based on the chi-square test. ICU intensive care unit, DBP diastolic blood pressure. (PDF 387 KB)
About this article
Cite this article
Jiang, Z., Li, S., Wang, L. et al. A comparison of invasive arterial blood pressure measurement with oscillometric non-invasive blood pressure measurement in patients with sepsis. J Anesth 38, 222–231 (2024). https://doi.org/10.1007/s00540-023-03304-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03304-2