Abstract
Purpose
Research has shown that a higher dose of bupivacaine administered in continuous paravertebral block (CPVB) provides a greater analgesic effect after video-assisted thoracoscopic surgery (VATS). In this randomized, controlled, double-blind study, we hypothesized that 0.25% 8 ml/h of levobupivacaine administered in CPVB after VATS provides a greater analgesic effect than 0.125% 8 ml/h.
Methods
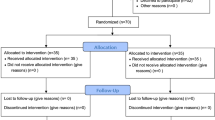
Fifty patients who underwent unilateral VATS were randomized to receive a postoperative continuous infusion of 0.125% (low group, n = 25) or 0.25% (high group, n = 25) levobupivacaine at 8 mL/h for CPVB. The primary outcome was the visual analog scale (VAS) score during coughing on the morning of postoperative day (POD) 1. The secondary outcomes were the VAS scores at rest and during coughing on POD 2, the number of anesthetized dermatomes, the frequency of rescue analgesics, postoperative nausea and vomiting, patient satisfaction, and adverse events and complications.
Results
There was no significant difference in the VAS score during coughing on the morning of POD 1 between the low and high groups [median, 37.5 (interquartile range 21–50) vs. 40.0 (interquartile range 21–50), respectively; p = 0.79]. Similarly, there were no significant differences in any secondary outcomes between the two groups.
Conclusions
Levobupivacaine at 0.25% 8 ml/h in CPVB did not provide better analgesia after VATS over 0.125% 8 ml/h.
Clinical trial registration number
UMIN000037930



Similar content being viewed by others
References
Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol. 2016;17:836–44.
Kaplowitz J, Papadakos PJ. Acute pain management for video-assisted thoracoscopic surgery: an update. J Cardiothorac Vasc Anesth. 2012;26:312–21.
Kaoud Abd-Elshafy S, Abdallal F, Zarief Kamel E, Edwar H, Abd Allah E, Hassan Mohamed Maghraby H, Ahmed Sayed J, Shaaban Ali M, Elkhayat H, Shalaby Khalaf Mahran G. Paravertebral dexmedetomidine in video-assisted thoracic surgeries for acute and chronic pain prevention. Pain Physician. 2019;22:271–80.
Davies RG, Myles PS, Graham JM. A comparison of the analgesic efficacy and side-effects of paravertebral vs. epidural blockade for thoracotomy - a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2006;96:418–26.
Hu Z, Liu D, Wang Z-Z, Wang B, Dai T. The efficacy of thoracic paravertebral block for thoracoscopic surgery. A meta-analysis of randomized trials. Medicine (Baltimore). 2018;97:e13771.
Yeung GHY, Gates S, Nadiu BV, Wilson MJA, Smith FG. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2:CD009121.
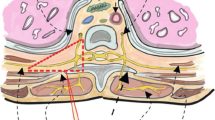
Krediet AC, Moayeri N, van Geffen GJ, Bruhn J, Renes S, Bigeleisen PE, Groen GJ. Different approaches of ultrasound-guided thoracic paravertebral block: an illustrated review. Anesthesiology. 2015;123:459–74.
Kotzé A, Scally A, Howell S. Efficacy and safety of different techniques of paravertebral block for analgesia after thoracotomy: a systematic review and metaregression. Br J Anaesth. 2009;103:626–36.
Shibata Y, Nishiwaki K. Ultrasound-guided intercostal approach to thoracic paravertebral block. Anesth Analg. 2009;109:996–7.
Kosiński S, Fryźlewicz E, Wiłkojć M, Ćmiel A, Zieliński M. Comparison of continuous epidural block and continuous paravertebral block in postoperative analgaesia after video-assisted thoracoscopic surgery lobectomy: a randomised, non-inferiority trial. Anaesthesiol Intensive Ther. 2016;48:280–7.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Heppolette CAA, Brunnen D, Bampoe S, Odor PM. Clinical pharmacokinetics and pharmacodynamics of levobupivacaine. Clin Pharmacokinet. 2020;59:715–45.
Baskan S, Taspinar V, Ozdogan L, Yetis Gulsoy K, Erk G, Dikmen B, Gogus N. Comparison of 0.25% levobupivacaine and 0.25% bupivacaine for posterior approach interscalene brachial plexus block. J Anesth. 2010;24:38–42.
Urbanek B, Duma A, Kimberger O, Huber G, Marhofer P, Zimpfer M, Kapral S. Onset time, quality of blockade, and duration of three-in-one blocks with levobupivacaine and bupivacaine. Anesth Analg. 2003;97:888–92.
Yoshida T, Fujiwara T, Furutani K, Ohashi N, Baba H. Effects of ropivacaine concentration on the spread of sensory block produced by continuous thoracic paravertebral block: a prospective, randomised, controlled, double-blind study. Anaesthesia. 2014;69:231–9.
Fagenholz PJ, Bowler GMR, Carnochan FM, Walker WS. Systemic local anaesthetic toxicity from continuous thoracic paravertebral block. Br J Anaesth. 2012;109:260–2.
Yoshida T, Watanabe Y, Hashimoto T, Ohta A, Nakamoto T. Effects of catheter tip location on the spread of sensory block caused by a continuous thoracic paravertebral block: a prospective, randomized, double-blind study. Biomed Res Int. 2019;2019:1051629.
Cox B, Durieux ME, Marcus MA. Toxicity of local anaesthetics. Best Pract Res Clin Anaesthesiol. 2003;17:111–36.
Bauer C, Pavlakovic I, Mercier C, Maury JM, Koffel C, Roy P, Fellahi JL. Adding sufentanil to ropivacaine in continuous thoracic paravertebral block fails to improve analgesia after video-assisted thoracic surgery: a randomised controlled trial. Eur J Anaesthesiol. 2018;35:766–73.
Hida K, Murata H, Ichinomiya T, Inoue H, Sato S, Hara T. Effects of programmed intermittent thoracic paravertebral bolus of levobupivacaine on the spread of sensory block: a randomized, controlled, double-blind study. Reg Anesth Pain Med. 2019;44:326–32.
Taketa Y, Irisawa Y, Fujitani T. Programmed intermittent bolus infusion versus continuous infusion of 0.2% levobupivacaine after ultrasound-guided thoracic paravertebral block for video-assisted thoracoscopic surgery: a randomised controlled trial. Eur J Anaesthesiol. 2019;36:272–8.
Luyet C, Hermann G, Ross S, Vogt A, Greif R, Moriggl B, Eichenberger U. Ultrasound-guided thoracic paravertebral puncture and placement of catheters in human cadavers: where do catheters go? Br J Anaesth. 2011;106:246–54.
Fujii T, Shibata Y, Ban Y, Shitaokoshi A, Takahashi K, Matsui S, Nishiwaki K. A single paravertebral injection via a needle vs. a catheter for spreading to multiple intercostal levels: a randomized controlled trial. J Anesth. 2020;34:72–8.
Stevens RA, Bray JG, Artuso JD, Kao TC, Spitzer L. Differential epidural block. Reg Anesth. 1992;17:22–5.
Chen L, Wu Y, Cai Y, Ye Y, Li L, Xia Y, Papadimos TJ, Xu X, Wang Q. Comparison of programmed intermittent bolus infusion and continuous infusion for postoperative patient-controlled analgesia with thoracic paravertebral block catheter: a randomized, double-blind, controlled trial. Reg Anesth Pain Med. 2019;44:240–5.
Acknowledgements
The authors thank the nurses on the lung surgery ward and in the intensive care unit of Bell Land General Hospital for serving as assessors in this study. The authors also thank Angela Morben, DVM, ELS, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
The authors have no sources of funding to declare for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kawase, S., Horiuchi, T. & Nagahata, T. 0.125% 8 ml/h v.s. 0.25% 8 ml/h of levobupivacaine in continuous paravertebral block for postoperative analgesia in video-assisted thoracoscopic surgery: a randomized, controlled, double-blind study. J Anesth 37, 6–12 (2023). https://doi.org/10.1007/s00540-022-03114-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-022-03114-y