Abstract
Purpose
The dynamic response of pressure monitoring circuits must be evaluated to obtain true invasive blood pressure values. Since Gardner’s recommendations in 1981, the natural frequency and the damping coefficient have become standard parameters for anesthesiologists. In 2006, we published a new dynamic response evaluation method (step response analysis) that can plot frequency spectrum curves instantly in clinical situations. We also described the possibility of the defect of the standard parameters. However, the natural frequency and the damping coefficient are considered the gold standard and are even included in a major anesthesiology textbook. Therefore, we attempted to clarify the issues of these parameters with easy-to-understand pressure waves and basic numerical formulae.
Methods
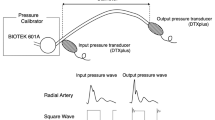
A blood pressure wave calibrator, a single two-channel pressure amplifier, and personal computer were used to analyze blood pressure monitoring circuits. All data collection and analytical processes were performed using our step response analysis program.
Results
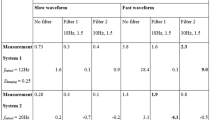
We compared two different circuits with almost the same natural frequency and damping coefficients. However, their amplitude spectrum curves and input/output pressure values were significantly different.
Conclusions
The natural frequency and the damping coefficient are inadequate for the dynamic response evaluation. These parameters are primarily obtained from the phase spectrum curve and not from the amplitude spectrum curve. We strongly recommend an evaluation using the amplitude spectrum curve with our step response analysis method. It is crucial to maintain an amplitude gain of 1 (input amplitude = output amplitude) in the pressure wave frequency range of 0–20 Hz.





Similar content being viewed by others
References
Geddes LA. The direct and indirect measurement of blood pressure. Chicago: Year Book Medical Publishers; 1970. p. 48.
Gardner RM. Direct blood pressure measurement—dynamic response requirements. Anesthesiology. 1981;54(3):227–36.
Schroeder B, Barbeito A, Bar-Yosef S, Mark JB. Cardiovascular monitoring. In: Miller RD, editor. Miller's anesthesia. 8th ed. Philadelphia: Elsevier; 2015. p. 1345–1395.
Watanabe H, Yagi S, Namiki A. Recommendation of a clinical impulse response analysis for catheter calibration—damping coefficient and natural frequency are incomplete parameters for clinical evaluation. J Clin Monit Comput. 2006;20(1):37–42.
Fujiwara S, Tachihara K, Mori S, Ouchi K, Yokoe C, Imaizumi U, Morimoto Y, Miki Y, Toyoguchi I, Yoshida K, Yokoyama T. Effect of using a PlanectaTM port with a three-way stopcock on the natural frequency of blood pressure transducer kits. J Clin Monit Comput. 2016;30(6):925–31.
Kleinman B, Powell S. Dynamic response of the ROSE damping device. J Clin Monit. 1989;5(2):111–5.
Watanabe H, Yagi S, Namiki A. Recommendation of a new clinical impulse response analysis for catheter calibration—let’s evaluate your pressure monitoring lines in the operating room just after priming. Anesth Analg. 2006;102:S155.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Figure 6 is a simple hydraulic model of the pressure monitoring system.
This pressure monitoring system is represented by a second-order linear differential equation as follows:
\(M\ddot{x}\left( t \right) = {\text{Inertial drag}} = {\text{Mass}} \times {\text{Acceleration}}\) \(R\dot{x}\left( t \right) = {\text{Viscous drag}} = {\text{Viscous resistance}} \times {\text{Velocity}}\) \(Kx\left( t \right) = {\text{Elastic drag}} = {\text{Elastic constant}} \times {\text{Displacement}}\) \(f\left( t \right) = {\text{External force}}\)
Harmonic analysis is conducted to determine the characteristic (spectrum) at the arbitrary frequency \((\omega = 2\pi f)\).
Displacement:
External force:
Velocity:
Acceleration:
Substituting Eqs. (2)–(5) into (1) and deleting the common denominator \({e}^{j\omega t}\) gives the following:
Transfer function \(H\left( \omega \right) \) (the displacement output for the external force) is as follows:
\(H\left( \omega \right)\) is composed of the amplitude and phase spectra:
Amplitude spectrum: \(\left| {H\left( \omega \right)} \right|,\) Phase spectrum: \(\theta \left( \omega \right)\).
The amplitude spectrum (\(\left| {H\left( \omega \right)} \right|\)) at the natural frequency \(\left( {\omega_{n} } \right)\) is as follows:
It is difficult to obtain the natural frequency directly from the amplitude spectrum. On the other hand, we can obtain the natural frequency from the phase spectrum \(\theta \left( {\omega_{n} } \right)\), which is represented by complex numbers:
In the complex number plane (Fig. 7), the phase at the natural frequency \(\theta \left( {\omega_{n} } \right)\) is \(- \frac{\pi }{2}\).
This means that the frequency at the natural frequency is derived from the phase spectrum curve and the natural frequency is at \(- \frac{\pi }{2}\) on the phase sperum curve.
About this article
Cite this article
Watanabe, H., Yagi, Si. Why the natural frequency and the damping coefficient do not evaluate the dynamic response of clinically used pressure monitoring circuits correctly. J Anesth 34, 898–903 (2020). https://doi.org/10.1007/s00540-020-02843-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-020-02843-2