Abstract
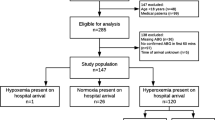
While oxygen administration has been in clinical practice, the focus has generally been on avoidance of hypoxemia. More recently, renewed emphasis has been placed on the potential deleterious effects of hyperoxia. The aim of this study is to investigate the incidence of intraoperative inadvertent hyperoxia among neonate, which was defined at three different thresholds: normoxia (PaO2 60–100 mmHg), hyperoxia (PaO2 101–199 mmHg), and severe hyperoxia (PaO2 ≥ 200 mmHg). This study included 65 patients with 174 eligible arterial blood gas (ABG) samples, who were less than 60 weeks post-menstrual age and required a non-cardiac surgical procedure. Among the 65 patients, 62 (96%) patients experienced either hyperoxia or severe hyperoxia during general anesthesia on at least one ABG. Among the 174 ABG readings, only 28 (16%) had PaO2 levels within our defined normoxia range. The incidence of hyperoxia in neonate under general anesthesia is high. Although it is unknown if brief exposure during anesthesia is associated with similar outcomes, educational initiatives seem warranted to increase awareness of these clinical concerns, as there seems to be limited clinical benefit from such care.
Similar content being viewed by others
References
Owen LS, Manley BJ, Davis PG, Doyle LW. The evolution of modern respiratory care for preterm infants. Lancet. 2017;389:1649–59.
Walsh BK, Smallwood CD. Pediatric oxygen therapy: a review and update. Respir Care. 2017;62:645–61.
Resseguie EA, Staversky RJ, Brookes PS, O’Reilly MA. Hyperoxia activates ATM independent from mitochondrial ROS and dysfunction. Redox Biol. 2015;5:176–85.
Rook D, Schierbeek H, Vento M, Vlaardingerbroek H, van der Eijk AC, Longini M, Buonocore G, Escobar J, van Goudoever JB, Vermeulen MJ. Resuscitation of preterm infants with different inspired oxygen fractions. J Pediatr. 2014;164(1322–1326):e3.
Cayabyab R, Ramanathan R. Retinopathy of prematurity: therapeutic strategies based on pathophysiology. Neonatology. 2016;109:369–76.
Aversa S, Marseglia L, Manti S, D’Angelo G, Cuppari C, David A, Chirico G, Gitto E. Ventilation strategies for preventing oxidative stress-induced injury in preterm infants with respiratory disease: an update. Paediatr Respir Rev. 2016;17:71–9.
Jobe A. Mechanisms of lung injury and bronchopulmonary dysplasia. Am J Perinat. 2016;33:1076–8.
Tataranno M, Oei J, Perrone S, Wright I, Smyth J, Lui K, Tarnow Mordi W, Longini M, Proietti F, Negro S, Saugstad O, Buonocore G. Resuscitating preterm infants with 100% oxygen is associated with higher oxidative stress than room air. Acta Paediatr. 2015;104:759–65.
Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, Simon WM, Weiner GM, Zaichkin JG. Part 13: Neonatal resuscitation. Pediatrics. 2015;136:S196–218.
Askie LM, Darlow BA, Finer N, Schmidt B, Stenson B, Tarnow-Mordi W, Davis PG, Carlo WA, Brocklehurst P, Davies LC, Das A, Rich W, Gantz MG, Roberts RS, Whyte RK, Costantini L, Poets C, Asztalos E, Battin M, Halliday HL, Marlow N, Tin W, King A, Juszczak E, Morley CJ, Doyle LW, Gebski V, Hunter KE, Simes RJ. Association between oxygen saturation targeting and death or disability in extremely preterm infants in the neonatal oxygenation prospective meta-analysis collaboration. JAMA. 2018;319:2190–201.
Manja V, Lakshminrusimha S, Cook DJ. Oxygen saturation target range for extremely preterm infants: a systematic review and meta-analysis. JAMA Pediatr. 2015;169:332–40.
Kayton A, Timoney P, Vargo L, Perez JA. A review of oxygen physiology and appropriate management of oxygen levels in premature neonates. Adv Neonat Care. 2018;18:98–104.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No competing financial interests exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Wakimoto, M., Miller, R., Chenault, K. et al. Inadvertent hyperoxia during intraoperative care in neonates: a case-series study. J Anesth 34, 149–152 (2020). https://doi.org/10.1007/s00540-019-02720-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02720-7