Abstract
Purpose
Studies evaluating the safety of hydroxyethyl starch with a molecular weight of 70 kDa and a molar substitution ratio of 0.5 (HES 70/0.5) are scarce in the literature. In this study, we investigated the relationship between intraoperative HES 70/0.5 administration and postoperative bleeding.
Methods
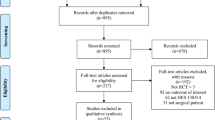
This is a single-center, retrospective cohort study. Subjects were postoperative adult patients who stayed in the intensive care unit (ICU) for more than 24 h during the period from January 1, 2010 to December 31, 2012. We compared postoperative adult patients with and without intraoperative HES 70/0.5 administration. The primary outcome was the drainage volume from surgical sites during the first 24 h after ICU admission. We conducted propensity score matching between the control group and the HES group.
Results
We analyzed data for 769 patients who met our inclusion criteria. Using propensity score matching, we successfully created 119 matched pairs from the HES group and control group, with no significant differences in patient characteristics. The drainage volume during the first 24 h after ICU admission was greater in the HES group than in the control group (400 ± 479 vs. 260 ± 357 mL, p < 0.003).
Conclusion
Our retrospective cohort study suggests that intraoperative HES 70/0.5 administration is associated with increased postoperative bleeding.

Similar content being viewed by others
References
Finfer S, Liu B, Taylor C, Bellomo R, Billot L, Cook D, Du B, McArthur C, Myburgh J, SAFE TRIPS Investigators. Resuscitation fluid use in critically ill adults: an international cross-sectional study in 391 intensive care units. Crit Care. 2010;14:R185.
Westphal M, James MF, Kozek-Langenecker S, Stocker R, Guidet B, Van Aken H. Hydroxyethyl starches: different products—different effects. Anesthesiology. 2009;111:187–202.
Kozek-Langenecker SA. Effects of hydroxyethyl starch solutions on hemostasis. Anesthesiology. 2005;103:654–60.
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, Glass P, Lipman J, Liu B, McArthur C, McGuinness S, Rajbhandari D, Taylor CB, Webb SA, CHEST Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901–11.
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Åneman A, Madsen KR, Møller MH, Elkjær JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Søe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjældgaard AL, Fabritius ML, Mondrup F, Pott FC, Møller TP, Winkel P, Wetterslev J, 6S Trial Group; Scandinavian Critical Care Trials Group. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124–34.
Endo A, Uchino S, Iwai K, Saito K, Sanui M, Takinami M, Uezono S. Intraoperative hydroxyethyl starch 70/0.5 is not related to acute kidney injury in surgical patients: retrospective cohort study. Anesth Analg. 2012;115:1309–14.
Paul M, Dueck M, Joachim Herrmann H, Holzki J. A randomized, controlled study of fluid management in infants and toddlers during surgery: hydroxyethyl starch 6% (HES 70/0.5) vs lactated Ringer’s solution. Paediatr Anaesth. 2003;13:603–8.
Suzuki T, Miyao H, Terui K, Koyama K, Shiibashi M. Fluid therapy with hydroxyethyl starch for massive blood loss during surgery. J Anesth. 2010;24:418–25.
Kotake Y, Fukuda M, Yamagata A, Iwasaki R, Toyoda D, Sato N, Ochiai R. Low molecular weight pentastarch is more effective than crystalloid solution in goal-directed fluid management in patients undergoing major gastrointestinal surgery. J Anesth. 2014;28:180–8.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25:1–21.
Jamnicki M, Bombeli T, Seifert B, Zollinger A, Camenzind V, Pasch T, Spahn DR. Low- and medium-molecular-weight hydroxyethyl starches: comparison of their effect on blood coagulation. Anesthesiology. 2000;93:1231–7.
Jacob M, Bruegger D, Rehm M, Welsch U, Conzen P, Becker BF. Contrasting effects of colloid and crystalloid resuscitation fluids on cardiac vascular permeability. Anesthesiology. 2006;104:1223–31.
Komori M, Takada K, Tomizawa Y, Uezono S, Nishiyama K, Ozaki M. Effects of colloid resuscitation on peripheral microcirculation, hemodynamics, and colloidal osmotic pressure during acute severe hemorrhage in rabbits. Shock. 2005;23:377–82.
Ueyama H, He YL, Tanigami H, Mashimo T, Yoshiya I. Effects of crystalloid and colloid preload on blood volume in the parturient undergoing spinal anesthesia for elective Cesarean section. Anesthesiology. 1999;91:1571–6.
Conroy JM, Fishman RL, Reeves ST, Pinosky ML, Lazarchick J. The effects of desmopressin and 6% hydroxyethyl starch on factor VIII:C. Anesth Analg. 1996;83:804–7.
Ickx BE, Bepperling F, Melot C, Schulman C, Van der Linden PJ. Plasma substitution effects of a new hydroxyethyl starch HES 130/0.4 compared with HES 200/0.5 during and after extended acute normovolaemic haemodilution. Br J Anaesth. 2003;91:196–202.
Zdolsek HJ, Vegfors M, Lindahl TL, Törnquist T, Bortnik P, Hahn RG. Hydroxyethyl starches and dextran during hip replacement surgery: effects on blood volume and coagulation. Acta Anaesthesiol Scand. 2011;55:677–85.
Deusch E, Gamsjäger T, Kress HG, Kozek-Langenecker SA. Binding of hydroxyethyl starch molecules to the platelet surface. Anesth Analg. 2003;97:680–3.
Franz A, Bräunlich P, Gamsjäger T, Felfernig M, Gustorff B, Kozek-Langenecker SA. The effects of hydroxyethyl starches of varying molecular weights on platelet function. Anesth Analg. 2001;92:1402–7.
Van Der Linden P, James M, Mythen M, Weiskopf RB. Safety of modern starches used during surgery. Anesth Analg. 2013;116:35–48.
Haase N, Wetterslev J, Winkel P, Perner A. Bleeding and risk of death with hydroxyethyl starch in severe sepsis: post hoc analyses of a randomized clinical trial. Intensive Care Med. 2013;39:2126–34.
Meybohm P, Van Aken H, De Gasperi A, De Hert S, Della Rocca G, Girbes AR, Gombotz H, Guidet B, Hasibeder W, Hollmann MW, Ince C, Jacob M, Kranke P, Kozek-Langenecker S, Loer SA, Martin C, Siegemund M, Wunder C, Zacharowski K. Re-evaluating currently available data and suggestions for planning randomised controlled studies regarding the use of hydroxyethyl starch in critically ill patients—a multidisciplinary statement. Crit Care. 2013;17:R166.
Coriat P, Guidet B, de Hert S, Kochs E, Kozek S, Van Aken H. Counter statement to open letter to the Executive Director of the European Medicines Agency concerning the licensing of hydroxyethyl starch solutions for fluid resuscitation. Br J Anaesth. 2014;113:194–5.
Myburgh J, Finfer S, Bellomo R. Patient-centered outcomes and trials of hydroxyethyl starch. Crit Care. 2013;17:452.
Phillips DP, Kaynar AM, Kellum JA, Gomez H. Crystalloids vs. colloids: KO at the twelfth round? Crit Care. 2013;17:319.
Bellomo R, Bion J, Finfer S, Myburgh J, Perner A, Reinhart K. Open letter to the Executive Director of the European Medicines Agency concerning the licensing of hydroxyethyl starch solutions for fluid resuscitation. Br J Anaesth. 2014;112:595–600.
Devereaux PJ, Mrkobrada M, Sessler DI, Leslie K, Alonso-Coello P, Kurz A, Villar JC, Sigamani A, Biccard BM, Meyhoff CS, Parlow JL, Guyatt G, Robinson A, Garg AX, Rodseth RN, Botto F, Lurati Buse G, Xavier D, Chan MT, Tiboni M, Cook D, Kumar PA, Forget P, Malaga G, Fleischmann E, Amir M, Eikelboom J, Mizera R, Torres D, Wang CY, VanHelder T, Paniagua P, Berwanger O, Srinathan S, Graham M, Pasin L, Le Manach Y, Gao P, Pogue J, Whitlock R, Lamy A, Kearon C, Baigent C, Chow C, Pettit S, Chrolavicius S, Yusuf S, POISE-2 Investigators. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014;370:1494–503.
Rasmussen KC, Johansson PI, Højskov M, Kridina I, Kistorp T, Thind P, Nielsen HB, Ruhnau B, Pedersen T, Secher NH. Hydroxyethyl starch reduces coagulation competence and increases blood loss during major surgery: results from a randomized controlled trial. Ann Surg. 2014;259:249–54.
Dixon B, Santamaria JD, Reid D, Collins M, Rechnitzer T, Newcomb AE, Nixon I, Yii M, Rosalion A, Campbell DJ. The association of blood transfusion with mortality after cardiac surgery: cause or confounding? (CME). Transfusion. 2013;53:19–27.
Dixon B, Reid D, Collins M, Newcomb AE, Rosalion A, Yap CH, Santamaria JD, Campbell DJ. The operating surgeon is an independent predictor of chest tube drainage following cardiac surgery. J Cardiothorac Vasc Anesth. 2014;28:242–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Assistance with the study
None.
Funding
Our departmental funding supported this study. No other funding was received.
The authors have no conflicts of interest.
About this article
Cite this article
Fukushima, T., Uchino, S., Fujii, T. et al. Intraoperative hydroxyethyl starch 70/0.5 administration may increase postoperative bleeding: a retrospective cohort study. J Anesth 31, 330–336 (2017). https://doi.org/10.1007/s00540-017-2334-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-017-2334-2