Abstract
Purpose
Continuous lenalidomide maintenance treatment after autologous stem cell transplantation delivers improvement in progression free and overall survival among newly diagnosed multiple myeloma patients and has been the standard of care in the UK since March 2021. However, there is scant information about its impact on patients’ day-to-day lives. This service evaluation aimed to qualitatively assess patients receiving lenalidomide treatment at a cancer centre in London, in order that the service might better align with needs and expectations of patients.
Methods
We conducted 20 semi-structured interviews among myeloma patients who were on continuous lenalidomide maintenance treatment at a specialist cancer centre in London. Members of the clinical team identified potentially eligible participants to take part, and convenience sampling was used to select 10 male and 10 female patients, median age of 58 (range, 45–71). The median treatment duration was 11 months (range, 1–60 months). Participants were qualitatively interviewed following the same semi-structured interview guide, which was designed to explore patient experience and insights of lenalidomide. Reflexive thematic analysis was used for data analysis.
Results
Four overarching themes were as follows: (i) lenalidomide: understanding its role and rationale; (ii) reframing the loss of a treatment-free period to a return to normal life; (iii) the reality of being on lenalidomide: balancing hopes with hurdles; (iv) gratitude and grievances: exploring mixed perceptions of care and communication. Results will be used to enhance clinical services by tailoring communication to better meet patients’ preferences when making treatment decisions.
Conclusion
This study highlights that most patients feel gratitude for being offered continuous lenalidomide and perceive it as alleviating some fears concerning relapse. It reveals variations in side effects in different age groups; younger patients reported no/negligible side effects, whilst several older patients with comorbidities described significant symptom burden, occasionally leading to treatment discontinuation which caused distress at the perceived loss of prolonged remission. Future research should prioritise understanding the unique needs of younger patients living with multiple myeloma.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Background
Multiple myeloma (MM) is an incurable malignancy of plasma cells in the bone marrow and is the second most common haematological malignancy, with incidence set to rise due to an ageing population [1, 2]. Patients with MM often experience high symptom burden including fatigue, bone pain, fractures, and kidney failure [3].
In the UK, initial treatments for MM include high-dose chemotherapy and autologous stem cell transplantation (ASCT) [4], which can cause side effects such as neuropathy, fatigue, and gastrointestinal issues [5]. An older patient profile means that age-related comorbidities often coincide with these symptoms [6]. The MM disease trajectory is characterised by periods of active disease followed by treatment-induced remission that shorten as the disease progresses, eventually becoming non-responsive to treatment [7,8,9], causing uncertainty for many patients [10]. A meta-aggregation of 11 qualitative studies examining experiences of MM suggests that grief and isolation are common [11], with quantitative surveys suggesting that patients can experience depression [12], anxiety [13], and poor health-related quality of life (QoL) [14, 15].
The outcomes of patients with MM have improved with novel therapies in the last 20 years [16]; however, relapse is almost inevitable; thus a key treatment objective is to prolong progression-free survival (PFS) and overall survival (OS) whilst minimising toxicity [17]. In 2021 the National Institute of Clinical Excellence (NICE) approved continuous lenalidomide for eligible UK National Health Service (NHS) patients receiving ASCT post-induction chemotherapy [18], after randomised trials demonstrated extended PFS and OS compared to placebo by enhancing the depth of disease response through the suppression of residual malignant cells [19,20,21,22,23]. Patient-reported outcomes from an observational study of 169 patients receiving lenalidomide maintenance and 137 receiving no maintenance suggest manageable side effects [24]. However, clinical trial data demonstrate that neutropenia, fatigue, neuropathy, and gastrointestinal disturbances are common, particularly in the first 6 months of treatment [20, 21], with two large trials indicating that 29% of participants experienced severe enough side effects to discontinue treatment [19]. Data also show that lenalidomide increases the risk of secondary malignancies [25].
Before lenalidomide maintenance was used in this setting, individuals would typically enter a treatment-free phase after ASCT, where they might experience a reasonable QoL without treatment burden [26], but maintenance eliminates that opportunity. A discrete choice experiment examining treatment preferences suggested that medication breaks provide an opportunity for patients to detach from the ‘illness’ experience [27], a finding echoed in a qualitative evaluation of ASCT during the COVID-19 pandemic [28]. However, a survey of 736 MM patients exploring perceptions of maintenance versus side-effect burden showed two-thirds would opt for maintenance if it offered PFS benefit, even if it was mildly toxic and showed no OS improvement [29]. Whilst the PFS and OS benefits of lenalidomide are proven, both short- and longer-term toxicities reported in trials mean that the trade-off between efficacy and harm should be considered [30] Yet to our knowledge, no exploration of patients’ experience of being on continuous lenalidomide has been conducted, and a deeper understanding of how it might impact individuals’ QoL is scant. Qualitative research can explore the complexity of human experiences, providing insights into individuals’ perspectives [31, 32]. The objectives of this qualitative service evaluation at a single-centre department in London were to:
-
1)
Explore patients’ understanding of the role of lenalidomide in their treatment for MM.
-
2)
Examine patients’ experience of lenalidomide, including perceived impact on QoL and experience of side effects.
It was anticipated that the findings would be consolidated and presented to clinicians so that improvements could be integrated into future care, through the delivery of communication better suited to patients’ needs.
Methods
Participants and recruitment
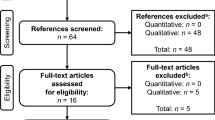
Participants were patients in a specialist cancer centre in a large, university-affiliated central London hospital, where they were receiving MM treatment. As this was a study exploring experiences of patients on lenalidomide maintenance treatment, participants were eligible for the study if they had undergone induction chemotherapy followed by ASCT and were receiving continuous lenalidomide. If participants were unable to give informed consent or did not possess adequate proficiency in the English language, they were deemed ineligible to take part. Patients were approached by members of the clinical care team and asked to consider taking part in an interview examining the perceived impact of lenalidomide on their lives. Participants were recruited using convenience sampling, where the selection was based on their availability and willingness to contribute. The invitation letter stated there was no obligation to participate, and that non-participation would not impact ongoing care. If they agreed to take part, they were emailed the study information and given a week to consider participation. In line with Health Research Authority guidelines, ethical approval was not required as the study was a service evaluation [33]. Those who agreed to participate gave written, informed consent to the research team contacting them to arrange interviews, and to their details being stored on a secure system called the University College London (UCL) Data Safe Haven. A target sample size of 16–24 participants was determined as acceptable for achieving adequate information power, with the understanding that more would be recruited if this was not attained [34].
Data collection
One-to-one in-depth semi-structured qualitative interviews (mean duration 52 min) were conducted (via telephone/MS Teams) between June and October 2022. Three health psychology researchers (2 females: CB and EB, 1 male: FB) with qualitative research experience carried out the interviews and took notes. One researcher (CB) had previously conducted research among MM patients [28]. A semi-structured guide was designed by the team to examine patients’ experiences of being on lenalidomide, their understanding of its role, and its perceived impact on their lives (See Supplementary Material 1 for guide). The guide was pilot tested on one patient by CB to ensure flow, and to ensure it encouraged participants to share experiences of lenalidomide and how information was understood/interpreted. The final sample size was based on the concept of ‘information power’ [34], which suggests that study aims, data richness, and analytical strategy dictate sample size. According to the guidelines of this commonly used paradigm in qualitative research, the sample size was deemed adequate when the incorporation of additional data contributed minimal or negligible alteration to the findings, in this case after 20 interviews had been conducted. Interviews were audio-recorded, anonymised, and transcribed verbatim by an external transcription service with a UCL data sharing agreement, with identifiable information removed. The researchers had no pre-existing relationship with participants.
Analysis
Interview transcripts were analysed using reflexive thematic analysis (RTA) [35], which acknowledges researcher subjectivity in data engagement [36]. Analysis was underpinned by a critical realist ontology that recognised how participants’ experiences were influenced by their social, cultural, and personal beliefs [37]. The epistemological stance taken was one of social constructionism, which assumes knowledge is co-constructed by researchers and participants [38].
Two researchers (CB and FB) adhered to RTA’s six stages [39]. Microsoft Word and Excel were used to manage the data. In Data familiarisation, analytical points of interest were identified by reviewing transcripts; Coding involved noting relevant segments and applying labels; Generating initial themes identified shared patterns that formed the basis for developing themes; Developing and reviewing themes ensured themes communicated a compelling story; Refining, defining and naming themes assigned descriptions and names to themes; Writing up involved completion of the analysis. HP and RT reviewed themes with the lead author (CB) to minimise bias and promote reflexivity, and CB kept a reflexive journal throughout the process [35]. The Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist was the basis for the reporting of this research [40] (See Supplementary Material 2).
Results
Participants
Twenty-four patients were approached and 20 agreed to take part. Two declined because of ill health and two did not give reasons. The mean interview duration was 52 min (range 22 to 98 min). See Table 1. for participant characteristics.
Themes and subthemes
Four themes and 12 subthemes were developed from the data; these are presented in Table 2 with illustrative quotes. Overarching themes were (1) lenalidomide: understanding its role and rationale, (2) reframing the loss of a treatment-free period to a return to normal life, (3) the reality of being on lenalidomide: balancing hopes with hurdles, and (4) gratitude and grievances: exploring patients’ mixed perceptions of care and communication.
Lenalidomide: understanding its role and rationale
Attitudes towards lenalidomide seemed to depend on timing of diagnosis
A pattern in the narratives was noted, whereby patients’ attitudes towards taking lenalidomide seemed to vary based on the timing of the diagnosis. In addition, there appeared to be varied understanding and evaluation of maintenance treatment after initial discussion about lenalidomide with the medical team. Some patients diagnosed before NICE approval claimed to have been told that lenalidomide might impede normal life, as it precluded medication breaks. By contrast, it appears that among those diagnosed after NICE approval, many tended to feel that clinicians conveyed how lenalidomide could extend/improve their lives.
Many patients described how the challenges of their initial MM treatments such as ASCT often diverted attention from having the capacity to consider future treatments such as lenalidomide maintenance, leading to a failure to engage fully in discussions about it. This arguably added to variations in understanding about lenalidomide when it came time to start treatment. Furthermore, a small number of participants misunderstood what ‘maintenance’ actually meant, leading to more misunderstanding; some assumed it was an infrequent regime, e.g. an occasional scan or chemotherapy infusion rather than a long-term undertaking.
‘Lenalidomide doubles remission’ is convincing
Most patients came to believe that continuous lenalidomide would significantly extend remission and many were convinced that clinicians told them it would double their remission. This belief appeared to be decoded as a form of certainty of efficacy, which contrasted with the unpredictability of MM. Recognition of its considerable cost was apparent, alongside gratitude for its provision free of charge at point of delivery by the NHS.
Reframing the loss of a treatment-free period to a return to normal life
Lenalidomide: offering a welcomed sense of security
Participants describing resistance towards lenalidomide recalled a mindset change once they understood it offered an antidote to the uncertainty of waiting for relapse. Staving off relapse was associated with affording them the chance to feel ‘normal’ again, allowing time with family and friends, to pursue hobbies, or establish a previously eradicated sense of freedom. Consequently, the perceived disadvantages of lenalidomide were outweighed by optimism for these benefits.
Maintenance perceived as ‘just another pill’ versus a demanding treatment
Participants highlighted that the lenalidomide regimen was manageable, especially in contrast to the demands of induction and ASCT. For many, taking one pill a day did not constitute ‘treatment’ so much as ‘swallowing a tablet’, often alongside others.
Participants experienced strong emotions in their transition from frontline to maintenance treatment
Several participants reported how they surrendered to being a ‘patient’ when first diagnosed, ‘opting out’ of decision-making amid procedures/preparation for ASCT. In contrast, participants described that having to make choices again (i.e. decide whether to take lenalidomide) caused them consternation, which coincided with reduced doctor-patient interactions. Whilst desirable, having less medical support raised expectations from friends/family that life had returned to normal. Some patients described experiencing mental health symptoms (anxiety, depression), as they recognised implications of their illness and its perceived impact on their lives.
Several participants described a desire to address health behaviours, i.e. alcohol intake, diet, exercising, and stress in order to maximise treatment efficacy during maintenance. However, some (mostly older patients) expressed concerns about adopting new regimes without discussions with their medical team, which proved difficult due to time constraints. Some younger patients claimed to have sought health guidance from sources outside of the team to expand their health knowledge.
The reality of being on lenalidomide maintenance: balancing hopes with hurdles
Differing assumptions about the perceived impact of lenalidomide: from ambivalence to miracle cure
Patients' attitudes towards the perceived impact of lenalidomide on their disease trajectory appeared to fall into three groups: (i) a small group exhibited ambivalence, harbouring doubts regarding lenalidomide’s efficacy, often swayed by anecdotal evidence of people surviving with no additional treatment after ASCT; (ii) several participants appeared pragmatic, demonstrating an understanding of lenalidomide’s role in prolonging remission, whilst acknowledging that relapse was inevitable; (iii) a large group displayed ‘magical thinking’, affording lenalidomide with the capacity to provide them an exceptionally long remission and/or cure.
Despite differences in attitudes, the perceived benefits of lenalidomide appeared to strengthen for many over time, described as providing a conceptual safety net that kept the disease at bay. The desire to feel safe when evidence suggests precariousness was widespread. Some participants depicted lenalidomide as a buffer against the inevitability of relapse, a drawing of a metaphorical line in the sand.
Perceived impact of side effects on patients
Three distinct groups emerged in this sample: (i) a predominantly younger group of participants experienced minimal /no side effects, e.g. mild fatigue and bloating; (ii) a mixed age group experienced more pronounced symptoms such as joint pain, gastrointestinal discomfort, and fatigue that were reported to impact daily life to a tolerable degree (two patients’ dosage was reduced to alleviate symptoms); (iii) a group of mainly older participants experienced side effects which were reported as markedly impacting QoL; rashes, fatigue, gastric disturbances, bone pain; two patients had to discontinue treatment due to debilitating symptoms.
Many participants recounted difficulty in distinguishing between lenalidomide’s side effects and residual symptoms from MM; age was also cited as a proxy for aches/pains. This ambiguity served to reinforce the decision to continue taking it. A few participants worried when they experienced no side effects, as it led them to assume lenalidomide was ineffective. Some participants admitted sporadically skipping doses to lessen side effects, not always admitting this to the medical team.
Concerns about toxicity/secondary cancers were latent, growing more recessive as patients tolerated lenalidomide and fears were diminished. A small number avoided mentioning side effects to clinicians for fear of being taken off lenalidomide. Those required to reduce dosage or discontinue expressed deep disappointment at the thought of lost therapeutic benefits.
Blood tests as the focal point of worry and hope
Blood tests appeared to incite anxiety among many participants, as they were perceived as the only solid gauge of lenalidomide’s efficacy. For those with no or many side effects, test results provided evidence of the one thing patients knew was critical—continued remission as seen through paraprotein levels or light-chain analysis. Whilst most claimed faith in lenalidomide’s effectiveness, seeds of doubt emerged each time a blood test was due.
Gratitude and Grievances: Exploring patients’ mixed perceptions of care and communication
Perceptions of care
Most participants were positive about the MM department, and the perceived high standard of care received made several reticent to voice complaints for fear of causing offence. However, some described concerns about sudden changes in consultant and difficulties accessing the helpline.
Variable communication: seeking clarity about facts and side effects of lenalidomide
Several participants mentioned a lack of sufficient opportunity to discuss lenalidomide during consultations. Perceptions regarding the provision of side-effect information varied, with some reporting adequacy whilst others perceived ambiguity from clinicians themselves. Several turned to Myeloma UK/Facebook groups for lived experience about lenalidomide that was felt beyond the medical team’s remit.
Differing needs of younger patients
In this sample, patterns emerged in the narratives of patient needs that differed across age groups; younger patients (45–55 year olds) questioned and challenged the conventional doctor-patient paradigm, wanting a more balanced communication. They also sought detailed information about lenalidomide. Meanwhile, older participants mentioned that they mostly accepted what medics said without question. Continuity of care seemed crucial for all participants, but particularly so for younger males, as the medical team often served as their only outlet for discussing their illness. Moreover, younger participants expressed difficulty in finding MM support groups relatable, as they predominantly consisted of older individuals.
Patient dissatisfaction with remote medical consultations
Whilst acknowledging the need to avoid in-person consultations during the COVID-19 pandemic, many expressed dissatisfaction that remote doctor-patient interactions persisted. Telephone consultations were often perceived as impersonal, limiting the ability to be seen and heard by doctors.
Service evaluation
Findings were consolidated and presented to clinicians in a multidisciplinary team (MDT) meeting, with discussion around how they could integrate these into care (i.e. how they communicated information to patients who were going to begin lenalidomide maintenance). Main topics of interest for the clinicians were those presented in the final theme.
Discussion
This study found the timing of diagnosis impacted how maintenance was internalised by participants; consistent with other studies [26, 28], those diagnosed with pre-NICE approval were more likely to describe disappointment about missing treatment breaks. Conversely, later diagnosis reduced awareness of forfeiting a break in medication. Variations in understanding may have been compounded by participants’ distress at diagnosis, where shock hampered the ability to process information meaningfully, a finding noted in other studies [7].
Several participants reported how uncertainty about relapse adversely affected their lives, supporting findings from previous research [7]. Learning that lenalidomide can prolong PFS offered a semblance of certainty which juxtaposed with MM’s volatility. Furthermore, the act of taking one tablet was not perceived as ‘treatment’ per se, especially compared to induction chemotherapy/ASCT. Our study highlights that clinicians should aim to gradually disseminate information, highlighting that taking a daily pill offers the potential to prolong remission, thus deviating from the perception of it being a demanding regime.
In this sample, younger patients reported fewer side effects from lenalidomide treatment than older individuals, and a large mixed-age group viewed their symptoms as tolerable. These findings align with previous studies that showed the effects of lenalidomide are manageable [20, 21, 24]. However, a subset of predominantly older patients with comorbidities reported considerable symptom burden in this study, including digestive issues, bone pain, and fatigue, occasionally resulting in treatment discontinuation. Cessation of treatment due to adverse effects is reported in the literature, but with little detail [19,20,21, 24]. Whilst differences across ages were evident in this study, it is difficult to be conclusive, as evidence suggests the first 6 months of treatment are more likely to elicit side effects, and many participants in our sample had only recently started taking lenalidomide [20, 21]. Several participants were concerned about reducing/ missing doses, others worried if side effects did not materialise, and some underreported side effects for fear of being taken off it. These findings support a recent study that demonstrated reticence of some patients at describing side effects to their medical team [41], pointing towards a need to ensure patients understand the trade-off between efficacy and toxicity of lenalidomide, and for clinicians to encourage honest reporting of symptoms. Further research examining the impact of discontinuing maintenance treatment on patients would be a useful addition to the literature, specifically examining ways of supporting people who cannot tolerate it.
Several individuals conveyed experiences of strong negative emotions during transition from frontline to maintenance treatment, which is supported by research [12, 13]. Some expressed a desire to improve their health, aligning with studies demonstrating how MM patients assume the role of active consumers of medical information to inform self-care practices [7, 42]. These observations present an opportunity for the design/delivery of health behaviour interventions to help MM patients improve their well-being.
Whilst support groups clearly have a role, it is important to recognise their contribution to patient misinformation [43]. Whilst several patients held a realistic view of lenalidomide’s role, some recounted apocryphal tales of miraculous recoveries. Denial has been examined in previous research [44] showing that it constitutes a helpful coping strategy to navigate uncertainty [10]. Whilst denial can be dysfunctional, it may afford patients the space to absorb distressing information, and could have an adaptive role [45]. However, it does suggest a need to allocate adequate time/resources for patients to engage in discussions about lenalidomide to ensure clarity. This could include providing opportunities for pre-maintenance patients to interact with individuals further along in their treatment journey (moderated by a health professional), effectively fulfilling patients’ desire for lived experiences whilst reducing the spread of unsubstantiated information.
The qualitative literature on the experiences of younger MM patients is limited [46], and this study highlighted unique challenges faced by younger people who sought more inclusive communication, detailed information on lenalidomide, and continuity of care. It also emphasises the significance of personalised approaches and support services for managing MM in younger patients, highlighting the need for further exploration of this group to increase understanding.
Most participants trusted the care and expertise of healthcare staff in this MM department, but concerns arose over inconsistent information about lenalidomide. Criticisms of remote consultations’ cursory nature were also voiced. Studies on telemedicine barriers highlighted that phone/video calls reduce perceptions of emotional support [47, 48], suggesting that in-person consultations could enhance communication.
Strengths and limitations
To our knowledge, this is the first qualitative exploration of the influence of lenalidomide on patients’ lives. Qualitative research provides depth and understanding of individuals’s lived experiences. Interviews in this study were conducted by researchers unconnected to MM clinical service, which may have minimised social desirability. Our study had limitations: sampling at one NHS MM department limits generalisability; group comparisons (i.e. between younger and older patients) are based solely on the authors’ interpretations and need further studies to confirm this; telephone/video call interviews may have overlooked non-verbal cues and rapport-building observed in person.
Conclusions
Thanks to novel therapies MM has been transformed into a treatable disease with improving survival rates, yet it remains incurable. Patients might increasingly endure continuous medication to control the disease and prolong PFS and OS, whilst knowing that MM will eventually take its toll, and coming to terms with this can be challenging [49]. This study suggests that the promise of lenalidomide can sometimes cloud rational decision-making due to the intense desire for survival, leading to patients minimising side effects and experiencing anxiety about dosage and potential discontinuation of lenalidomide if they cannot tolerate it. Current knowledge about treatment effects is predominantly derived from clinical trials, and trial participants might not fully represent the broader MM population [50,51,52]. Findings provided key points for clinicians on how to personalise and improve service. Future studies could assess if changes were implemented to the service, and determine barriers and facilitators to change. This information could be implemented for a behavioural change intervention utilising the Integrated Promoting Action on Research Implementation in Health Services (i-PARIHS) framework [53]. Further qualitative research on the real-world symptom burden of treatments on patients’ lives could contribute to a more comprehensive understanding of the impact of MM, helping patients cope with the increasingly chronic nature of this disease.
Data availability
Can be made available on request.
References
Turesson I, Bjorkholm M, Blimark CH, Kristinsson S, Velez R, Landgren O (2018) Rapidly changing myeloma epidemiology in the general population: increased incidence, older patients, and longer survival. Eur J Haematol 101(2):237–244. https://doi.org/10.1111/ejh.13083
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67(1):7–30
Gasparetto C, Sivaraj D (2017) Understanding multiple myeloma. Jones & Bartlett Learning
National Institute for Health and Care Excellence (2016) Overview: myeloma: diagnosis and management: guidance. NICE. (n.d.-c). https://www.nice.org.uk/guidance/ng35. Accessed 5 Oct 2023
Boland E, Eiser C, Ezaydi Y, Greenfield DM, Ahmedzai SH, Snowden JA (2013) Living with advanced but stable multiple myeloma: a study of the symptom burden and cumulative effects of disease and intensive (hematopoietic stem cell transplant-based) treatment on health-related quality of life. J Pain Symptom Manage 46(5):671–680. https://doi.org/10.1016/j.jpainsymman.2012.11.003
Seitzler S, Finley-Oliver E, Simonelli C, Baz R (2019) Quality of life in multiple myeloma: considerations and recommendations. Expert Rev Hematol 12(6):419–424. https://doi.org/10.1080/17474086.2019.1613886
Stephens M, McKenzie H, Jordens CFC (2014) The work of living with a rare cancer: multiple myeloma. J Adv Nurs 70(12):2800–2809. https://doi.org/10.1111/jan.12430
Yong K, Delforge M, Driessen C, Fink L, Flinois A, Gonzalez-McQuire S, Safaei R, Karlin L, Mateos MV, Raab MS, Schoen P, Cavo M (2016) Multiple myeloma: patient outcomes in real-world practice. Br J Haematol 175(2):252–264. https://doi.org/10.1111/bjh.14213
Kumar SK, Therneau TM, Gertz MA, Lacy MQ, Dispenzieri A, Rajkumar SV, Fonseca R, Witzig TE, Lust JA, Larson DR, Kyle RA, Greipp PR (2004) Clinical course of patients with relapsed multiple myeloma. Mayo Clin Proc 79(7):867–874. https://doi.org/10.4065/79.7.867
Maher K, De Vries K (2011) An exploration of the lived experiences of individuals with relapsed multiple myeloma. Eur J Cancer Care 20(2):267–275
Hauksdóttir B (2017) Patients’ experiences with multiple myeloma: a meta-aggregation of qualitative studies. Number 2/March 2017 44(2):64-81
Ramsenthaler C, Osborne TR, Gao W, Siegert RJ, Edmonds PM, Schey SA, Higginson IJ (2016) The impact of disease-related symptoms and palliative care concerns on health-related quality of life in multiple myeloma: a multi-centre study. BMC Cancer 16(1). https://doi.org/10.1186/s12885-016-2410-2
Lamers J, Hartmann M, Goldschmidt H, Brechtel A, Hillengass J, Herzog W (2013) Psychosocial support in patients with multiple myeloma at time of diagnosis: who wants what? Psychooncology 22(10):2313–2320. https://doi.org/10.1002/pon.3284
Chakraborty R, Hamilton BK, Hashmi SK, Kumar SK, Majhail NS (2018) Health-related quality of life after autologous stem cell transplantation for multiple myeloma. Biol Blood Marrow Transplant 24(8):1546–1553. https://doi.org/10.1016/j.bbmt.2018.03.027
Zaleta AK, Miller MF, Olson JS, Yuen EYN, LeBlanc TW, Cole CE, McManus S, Buzaglo JS (2020) Symptom burden, perceived control, and quality of life among patients living with multiple myeloma. J Nat Compr Cancer Netw : JNCCN 18(8):1087–1095. https://doi.org/10.6004/jnccn.2020.7561
Landgren O, Iskander K (2017) Modern multiple myeloma therapy: deep, sustained treatment response and good clinical outcomes. J Intern Med 281(4):365–382. https://doi.org/10.1111/joim.12590
Gupta RK, Gupta A, Hillengass J, Holstein SA, Suman VJ, Taneja A, McCarthy PL (2022) A review of the current status of lenalidomide maintenance therapy in multiple myeloma in 2022. Expert Rev Anticancer Ther 22(5):457–469. https://doi.org/10.1080/14737140.2022.2069564
National Institute for Health and Care Excellence (2021) Overview: lenalidomide maintenance treatment after an autologous stem cell transplant for newly diagnosed multiple myeloma: Guidance. NICE. (n.d.-b). https://www.nice.org.uk/guidance/ta680. Accessed 5 Oct 2023
McCarthy PL, Holstein SA, Petrucci MT, Richardson PG, Hulin C, Tosi P, Attal M (2017) lenalidomide maintenance after autologous stem-cell transplantation in newly diagnosed multiple myeloma: a meta-analysis. J Clin Oncol 35(29):3279
Attal M, Lauwers-Cances V, Marit G, Caillot D, Moreau P, Facon T, Harousseau JL (2012) Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. New England J Med 366(19):1782–1791
McCarthy PL, Owzar K, Hofmeister CC, Hurd DD, Hassoun H, Richardson PG, ... & Linker C (2012) Lenalidomide after stem-cell transplantation for multiple myeloma. New England J Med 366(19):1770–1781
Palumbo A, Cavallo F, Gay F, Di Raimondo F, Ben Yehuda D, Petrucci MT, ... & Cavo M (2014) Autologous transplantation and maintenance therapy in multiple myeloma. New England J Med 371(10):895–905
Jackson G H, Davies FE, Pawlyn C, Cairns DA, Striha A, Collett C, ... & Morgan GJ (2019) Lenalidomide maintenance versus observation for patients with newly diagnosed multiple myeloma (Myeloma XI): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 20(1):57–73
Abonour R, Wagner L, Durie BG, Jagannath S, Narang M, Terebelo HR, ... & Rifkin RM (2018) Impact of post-transplantation maintenance therapy on health-related quality of life in patients with multiple myeloma: data from the Connect® MM Registry. Ann Hematol 97:2425–2436.
Holstein SA, Owzar K, Richardson PG, Jiang C, Hofmeister CC, Hassoun H, Hurd DD, Stadtmauer EA, Giralt S, Devine SM, Hars V, Postiglione JR, Weisdorf DJ, Vij R, Moreb JS, Callander NS, Martin TG, Shea TC, Anderson KC, McCarthy PL (2015) Updated analysis of CALGB/ECOG/BMT CTN 100104: Lenalidomide (LEN) vs. Placebo (PBO) maintenance therapy after Single Autologous Stem Cell Transplant (ASCT) for multiple myeloma (mm). J Clin Oncol 33(15_suppl):8523–8523. https://doi.org/10.1200/jco.2015.33.15_suppl.8523
Acaster S, Gaugris S, Velikova G, Yong K, Lloyd AJ (2012) Impact of the treatment-free interval on health-related quality of life in patients with multiple myeloma: a UK cross-sectional survey. Support Care Cancer 21(2):599–607. https://doi.org/10.1007/s00520-012-1548-y
Mühlbacher AC, Lincke HJ, Nübling M (2008) Evaluating patients’ preferences for multiple myeloma therapy, a Discrete-Choice-Experiment. GMS Psycho-Social Medicine 5
Camilleri M, Bekris G, Sidhu G, Buck C, Elsden E, McCourt O, Horder J, Newrick F, Lecat C, Sive J, Papanikolaou X, Popat R, Lee L, Xu K, Kyriakou C, Rabin N, Yong K, & Fisher A (2022) The impact of Covid-19 on autologous stem cell transplantation in multiple myeloma a single-centre service evaluation. https://doi.org/10.21203/rs.3.rs-1446612/v1
Burnette BL, Dispenzieri A, Kumar S, Harris AM, Sloan JA, Tilburt JC, Kyle RA, Rajkumar SV (2013) Treatment trade-offs in myeloma: a survey of consecutive patients about contemporary maintenance strategies. Cancer 119(24):4308–4315. https://doi.org/10.1002/cncr.28340
Mikhael JR (2017) Maintenance lenalidomide after transplantation in multiple myeloma prolongs survival-in most. J Clin Oncol 35(29):3269–3271
Pope C, Mays N (1995) Qualitative research: reaching the parts other methods cannot reach: an introduction to qualitative methods in health and Health Services Research. BMJ 311(6996):42–45. https://doi.org/10.1136/bmj.311.6996.42
Renjith V, Yesodharan R, Noronha JA, Ladd E, George A (2021) Qualitative methods in health care research. Int J Prev Med 12:20. https://doi.org/10.4103/ijpvm.IJPVM_321_19
NHS Health Research Authority (2017) Do I need NHS ethics approval? Retrieved from https://hra-decisiontools.org.uk
Malterud K, Siersma VD, Guassora AD (2016) Sample size in qualitative interview studies: guided by information power. Qual Health Res 26(13):1753–1760
Braun V, Clarke V (2021) Thematic analysis: a practical guide. SAGE, London
Braun V, Clarke V (2019) Reflecting on reflexive thematic analysis. Qual Res Sport, Exerc Health 11(4):589–597
Bhaskar R (2015) A realist theory of Science. Routledge
Andrews T (2012) What is social constructionism?. Grounded Theory Rev 11(1)
Braun V, Clarke V (2021) One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol 18(3):328–352
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19(6):349–357. https://doi.org/10.1093/intqhc/mzm042
McCourt O, Fisher A, Land J, Ramdharry G, Yong K (2023) The views and experiences of people with myeloma referred for autologous stem cell transplantation, who declined to participate in a physiotherapist-led exercise trial: a qualitative study. Physiotherapy Theory and Practice 1–13
Craike M, Hose K, Courneya KS, Harrison SJ, Livingston PM (2017) Physical activity preferences for people living with multiple myeloma: a qualitative study. Cancer Nurs 40(5):E1–E8
Wang Y, McKee M, Torbica A, Stuckler D (2019) Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med 240:112552
Vos MS, de Haes JC (2007) Denial in cancer patients, an explorative review. Psychooncology 16(1):12–25. https://doi.org/10.1002/pon.1051
Rabinowitz T, Peirson R (2006) “Nothing is wrong, doctor”: understanding and managing denial in patients with cancer. Cancer Investig 24(1):68–76. https://doi.org/10.1080/07357900500449678
Pydi VR, Bala SC, Kuruva SP, Chennamaneni R, Konatam ML, Gundeti S (2021) Multiple myeloma in young adults: a single centre real world experience. Indian J Hematol Blood Transfus 37(4):679–683. https://doi.org/10.1007/s12288-021-01410-3
Sanoff HK (2020) Managing grief, loss, and connection in oncology—what COVID-19 has taken. JAMA Oncol 6(11):1700–1701
Weaver MS, Neumann ML, Navaneethan H, Robinson JE, Hinds PS (2020) Human touch via touchscreen: rural nurses’ experiential perspectives on telehealth use in pediatric hospice care. J Pain Symptom Manage 60(5):1027–1033
Chakraborty R, Majhail NS (2020) Treatment and disease-related complications in multiple myeloma: implications for survivorship. Am J Hematol 95(6):672–690
LeBlanc MR, LeBlanc TW, Leak Bryant A, Pollak KI, Bailey DE, Smith SK (2021) A qualitative study of the experiences of living with multiple myeloma. Oncol Nurs Forum 48(2):151–160. https://doi.org/10.1188/21.ONF.151-160
LeBlanc MR, Hirschey R, Leak Bryant A, LeBlanc TW, Smith SK (2020) How are patient-reported outcomes and symptoms being measured in adults with relapsed/refractory multiple myeloma? A systematic review. Qual Life Res 29(6):1419–1431. https://doi.org/10.1007/s11136-019-02392-6
Costa LJ, Hari PN, Kumar SK (2016) Differences between unselected patients and participants in multiple myeloma clinical trials in US: a threat to external validity. Leuk Lymphoma 57(12):2827–2832. https://doi.org/10.3109/10428194.2016.1170828
Kitson A, Harvey G (2015) Facilitating an evidence-based innovation into practice. Implementing Evidence-Based Practice in Healthcare: A Facilitation Guide
Author information
Authors and Affiliations
Contributions
Methodology: C.B., A.F., and J.S.; formal analysis: C.B. and F.B.C.; investigation: C.B., F.B.C., and E.B.; data curation: C.B.; writing—original draft preparation: C.B.; writing—review and editing: C.B., F.B.C., O.M., J.L., J.S., A.F.; supervision: J.S. and A.F. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abigail Fisher and Jonathan Sive are joint senior authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Buck, C., Brenes Castillo, F., Bettio, E. et al. The impact of continuous lenalidomide maintenance treatment on people living with multiple myeloma—a single-centre, qualitative service evaluation study. Support Care Cancer 32, 479 (2024). https://doi.org/10.1007/s00520-024-08663-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08663-4