Abstract
Purpose
Research on symptom clusters in oncology is progressing, but knowledge gaps remain. One question is whether the number and types of symptom subgroups (i.e., latent classes) differ based on cancer diagnosis. The purpose of this study was to: (1) identify and compare latent class subgroups based on four highly prevalent symptoms (pain, fatigue, sleep disturbance, and depression), and (2) examine the differences in sociodemographic and clinical factors in the identified latent classes across the seven cancer types (i.e., prostate, non-small cell lung, non-Hodgkin’s lymphoma, breast, uterine, cervical, and colorectal cancer).
Methods
This study is a cross-sectional secondary analysis of data obtained from the My-Health study in partnership with four Surveillance, Epidemiology, and End Results (SEER) cancer registries located in California (two), Louisiana, and New Jersey. The sample included 4,762 cancer survivors 6-13 months following diagnosis of one of the seven cancer types mentioned. Latent class profile analysis was used.
Results
Subjects were primarily young (59% age 21-64 years), Caucasian (41%), married/cohabitating (58%) and unemployed (55%). The number and types of symptom subgroups varied across these seven cancer populations: four-subgroups were the common in prostate, lung, non-Hodgkin’s lymphoma, and breast cancer survivors. Unmarried, low education, and unemployment status were associated with high risk of symptom burden across the cancer types.
Conclusion
Identifying symptom subgroups by cancer diagnosis has the potential to develop innovative and effective targeted interventions in cancer survivors. Further research is needed to establish extensive knowledge in symptom clustering between treatment regimens, and short-term and long-term cancer survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well-established that individuals with cancer typically experience multiple symptoms [1], and pain, fatigue, sleep disturbance, and depression are common frequently concurrent symptoms reported by oncology patients [1, 2]. Recent literature in symptom management has emphasized a shift of focus from treating single symptoms to managing the dynamic nature of multiple symptom constellations, or symptom clusters [1]. A symptom cluster has been defined as two or more co-occurring symptoms that are related to each other. Symptom clusters are composed of stable groups of symptoms that are relatively independent of other clusters, and they may share underlying mechanisms and/or outcomes [3]. There is a growing body of evidence that symptom clusters might have significant effects on the health outcomes of patients with cancer, such as quality of life and functional status, often in a multiplicative rather than additive manner [4,5,6].
Although the identification of symptom clusters can result in effective symptom management interventions, gaps in symptom cluster research can be found in conceptual, methodological, and analytical issues [1, 7]. The conceptual issue relates to the manner in which symptom clusters are defined. Symptom clusters have been identified using two approaches: the empiric or “de novo” identification of symptom clusters, and the identification of subgroups of people based on their experiences with a specific symptom cluster (i.e., latent classes). Methodological issues include whether symptoms should be measured with unidimensional instruments assessing several symptoms or by several instruments, each focusing on more than one dimension of the same symptom. The analytical level is arguably the best manner of statistically identifying the existence of a symptom cluster [1]. The large number of measurements and statistical methods that have been used to identify symptom clusters, with little guidance regarding the justification of the choice of method, is a major barrier to the conceptual validity and clinical utility of statistically derived symptom clusters [1, 4].
Given the lack of consensus on conceptual, methodological, and analytical issues of symptom cluster research, numerous unanswered questions remain [1, 4]. One question is whether the number and types of symptom clusters differ depending on the cancer diagnosis. Using a heterogeneous sample can be challenging to determine if the symptom cluster presentation is inconsistent for a specific type of cancer. In addition, the extent to which the reported clusters are dependent on the cancer diagnoses is unclear. The use of different measurement tools and analytical methods to evaluate symptoms may also result in a different construction of symptom clusters. To compensate for heterogeneous samples and the use of inconsistent methodology, research is needed to evaluate for differences in the number and types of symptom clusters across cancer diagnoses using the same assessment tools and statistical methods. Consistent identification of symptom clusters is key to the development of targeted and tailored interventions for symptom clusters.
To date, relatively few studies have evaluated for symptom clusters across cancer diagnosis [8,9,10]. Dong and colleagues [8] investigated the consistency of symptom composition in patients with advanced cancer using three different statistical approaches (i.e., principal component analysis, exploratory factor analysis, cluster analysis) and demonstrated that symptom clusters were relatively consistent across five primary cancer sites (i.e., prostate, breast, lung, colorectal, myeloma). However, the patient samples used have been insufficient in size to allow comparison of cluster composition among cancer types. In addition, there have only been a few published studies that compared symptom clusters using the same statistical method [9, 10]. Harris and colleagues [9] identified symptom clusters using exploratory factor analysis in 1,329 oncology patients with four different cancer types (i.e., breast, gastrointestinal, gynecological, and lung cancers). In this study, psychological, weight gain and gastrointestinal clusters were stable across cancer types, while respiratory and hormonal clusters were unique to specific cancer diagnoses. Another study [10] assessing differences in symptom clustering across 1,330 survivors of five types of cancer (i.e., colorectal, breast, ovarian, thyroid, and hematological cancers) using the network analysis found that fatigue was consistently the most central symptom in the network with other symptoms (e.g., emotional symptoms, pain) across all cancer types.
However, previous studies in symptom clusters aforementioned above [8,9,10] have small sample size, inconsistent symptom measures across the studies, and variables-centered approaches (i.e., factor analysis). These limitations may hinder to identify distinct symptom phenotypes vary by different cancer types. The latent class model approach as a person-centered approach is a statistical method for identifying unobserved (i.e., latent) subgroups. The latent class analysis is beneficial for symptom research, where data often include heterogeneous groups of individuals with cancer experiencing multiple symptoms, and for identifying distinct subgroups, particularly with a group of common symptoms or a pre-defined symptom cluster, based on their symptoms [11, 12]. Although latent class modeling was used in a few studies in cancer survivors to identify symptom clusters [13,14,15], no published symptom cluster study using latent class analysis has compared distinct symptom subgroups across different cancer types. Comprehensive and representative samples of cancer survivors using the latent class approach in conjunction with well-validated and reliable patient-reported outcomes might be helpful in clarifying how subgroups of survivors may differ across different cancer diagnosis based on a symptom cluster. The purposes of this study were (1) to identify and compare latent class subgroups based on four highly prevalent symptoms (i.e., pain, fatigue, sleep disturbance, and depression) and (2) to investigate the differences in sociodemographic and clinical factors in the identified latent classes across seven populations of cancer survivors (i.e., prostate cancer, non-small cell lung cancer, non-Hodgkin’s lymphoma [NHL], breast cancer, uterine cancer, cervical cancer, and colorectal cancer).
Methods
Study cohort
This study was a cross-sectional secondary analysis of data from the Measuring Your Health (MY-Health) study, a prospective cohort study. In the parent study, data were collected to evaluate the health and well-being of a diverse cohort of individuals with cancer [16]. Participants in the MY-Health study were recruited through four Surveillance, Epidemiology, and End Results (SEER) registries located in California (two), Louisiana, and New Jersey between 2010 and 2012. Participants were eligible for the parent study if they (a) were 21-84 years old at the time of initial diagnosis of one of seven types of cancer (i.e., prostate cancer, non-small cell lung cancer, NHL, female breast cancer, uterine cancer, cervical cancer, and colorectal cancer); and (b) could read and speak English, Spanish, or Mandarin. Details of the study design, study procedures, and participant descriptions have been reported elsewhere [16]. This study was approved by the institutional review boards for each participating SEER site and Georgetown University (Washington, DC).
The survey was completed by 5,506 individuals with cancer. For this analysis, we restricted eligibility to individuals diagnosed with cancer within the previous six to thirteen months. Of 5,506 individuals with cancer, a total of 4,762 participants were included following the exclusion of 409 participants diagnosed thirteen or more months prior, 333 participants who had died during the survey period, and two participants with incomplete responses.
Measures
Symptoms were measured using the Patient Reported Outcomes Measurement Information System (PROMIS®) measures extensively validated in individuals with cancer [17]. The MY-Health study administered PROMIS® custom short forms assessing pain interference (10 items), fatigue (14 items), sleep disturbance (10 items), and depression (10 items). The PROMIS® measures are scored on a 5-point Likert-type scale from 1 (never) to 5 (always). Higher scores indicate higher symptom severity. The PROMIS® measures are calibrated and standardized to a T-score metric, with a mean of 50 and a standard deviation of 10 centered on the general United States population. The measure offers clinically relevant symptom thresholds and are as follows [18, 19].
-
Pain: <50 normal; 50-59 mild; 60-69 moderate; ≥70 severe
-
Fatigue: <50 normal; 50-54 mild; 55-74 moderate; ≥75 severe
-
Sleep disturbance: <45 normal, 45-54 mild; 55-59 moderate: ≥60 severe
-
Depression: <55 normal, 55-64 mild; 65-74 moderate; ≥75 severe
In this study, the internal consistency of the instrument was high (Cronbach’s alpha for pain interference = 0.98; fatigue = 0.96; sleep disturbance = 0.95; and depression = 0.97).
Statistical analysis
Latent class model approach, a type of finite mixture model, was used to divide our sample into unobserved (i.e., latent) homogeneous subgroups, which are called classes, using multiple observed variables. In the latent class analysis, categorical variables are typically used. When the indicators are continuous variables, it is termed latent class profile analysis (LCPA) [12]. In this study, seven separate LCPA (based on the seven cancer diagnoses) were conducted on the four symptom variables (i.e., pain, fatigue, sleep disturbance, depression). Estimation was carried out with the robust maximum-likelihood and Expectation-Maximization algorithms [12]. Statistical fit indices were used to both evaluate model fit and to determine the final number of latent classes. The model that fits the data best was selected by a combination of the following criteria: (1) the lowest Akaike information criterion (AIC); (2) the lowest Bayesian information criterion (BIC); (3) the lowest Vuong-Lo-Mendell Rubin likelihood ratio test (VLMR); (4) the lowest parametric bootstrapped likelihood ratio test (BLRT); and (5) entropy to be 0.80 or greater [12]. The latent classes were named based on established symptom cut points [18, 19]. Multivariate analysis of variance (MANOVA) was performed to analyze the differences in symptom severity among the latent classes. In addition, sociodemographic and clinical characteristics differ by latent class subgroups per cancer type were examined using Chi-square test. Mplus Version 8.6 was used for LCPA [20]. Other analyses were conducted with SPSS Version 28.0 for Windows [21].
Results
Sociodemographic and clinical characteristics of subjects
Data for 4,762 participants were examined in this analysis (Table 1). The participants were predominantly younger at diagnosis (21-64 years) (63.5%), female (60.3%), White (53.1%), non-Hispanic (80.3%), and married/cohabiting (58.9%). In terms of clinical characteristics, the majority of participants had cancer stages I and II (73.2%) and were primarily treated with surgery (69.3%).
Identification of latent class subgroups based on symptoms by cancer diagnosis
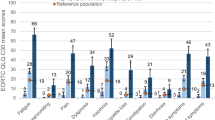
The results of statistical fit indices for the candidate models are shown in Table 2. As summarized in Table 3 and illustrated in Fig. 1, four distinct classes were identified in prostate, non-small cell lung, and breast cancer, and NHL survivors; three classes were discovered in uterus and cervical cancer survivors; and two classes were identified in colorectal cancer survivors based on symptom severity and types of symptoms.
Four-class solution
Prostate
Class 1 (67%), labeled Within Normal Limits (WNL), was characterized by all four symptoms within normal limits, based on established symptom cut points [18, 19]. Class 2 (15%) was characterized by mild pain with moderate fatigue and sleep disturbance, but no elevated depression (within normal limits), and was labeled Fatigue/sleep disturbance (SD)/Pain. Class 3 (10%) was characterized by mild sleep disturbance and depression with moderate fatigue, but pain was within normal limits, and was labeled as Fatigue/SD/Depression. Class 4 (8%), labeled All Symptoms, was characterized by moderate fatigue and sleep disturbance with severe pain and depression.
Non-small cell lung
Class 1 (46%), labeled WNL, was characterized by all four symptoms within normal limits. Class 2 (25%) was characterized by mild pain, fatigue, and sleep disturbance, but depression was within normal limits, and was labeled Fatigue/SD/Pain. Class 3 (13%) was characterized by mild sleep disturbance and depression, with moderate fatigue, but pain was within normal limits, and was labeled by Fatigue/SD/Depression. Class 4 (16%), labeled All Symptoms, was characterized by mild depression, with moderate pain, sleep disturbance, and fatigue.
NHL
Class 1 (55%), labeled WNL, was characterized by all four symptoms within normal limits. Class 2 (24%) was characterized by mild pain and sleep disturbance, with moderate fatigue, but depression was within normal limits, and was labeled Fatigue/SD/Pain. Class 3 (11%) was characterized by mild depression, with moderate fatigue and sleep disturbance, but pain was within normal limits, and was labeled by Fatigue/SD/Depression. Class 4 (10%), labeled All Symptoms, was characterized by moderate fatigue, sleep disturbance and depression, with severe pain.
Breast
Class 1 (57%), labeled WNL, was characterized by all four symptoms within normal limits. Class 2 (19%) was characterized by mild sleep disturbance, with moderate pain and fatigue, but depression was within normal limits, and was labeled Fatigue/Pain/SD. Class 3 (11%) was characterized by mild fatigue and depression, with moderate sleep disturbance, but pain was within normal limits, and was labeled by SD/Fatigue/Depression. Class 4 (13%), labeled All Symptoms was characterized by moderate pain, fatigue, and depression, with severe sleep disturbance.
Three-class Solution
Uterine
Class 1 (50%), labeled WNL, was characterized by all four symptoms within normal limits. Class 2 (34%) was characterized by mild pain and sleep disturbance, with moderate fatigue, but depression was within normal limits, and was labeled Fatigue/SD/Pain. Class 3 (16%) was characterized by mild depression, with moderate pain, fatigue, and sleep disturbance, and was labeled by All Symptoms.
Cervical
Three distinct classes of cervical cancer survivors were identified. Class 1 (42%), labeled WNL, was characterized by all four symptoms within normal limits. Class 2 (23%) was characterized by mild fatigue and sleep disturbance, but pain and depression were within normal limits, and was labeled Fatigue/SD. Class 3 (35%) was characterized by mild depression, with moderate pain, fatigue and sleep disturbance, and was labeled by All Symptoms.
Two-class Solution
Colorectal
Two distinct classes of cervical cancer survivors were identified. Class 1 (67%), labeled WNL, was characterized by all four symptoms within normal limits. Class 2 (33%) was characterized by mild depression, with moderate pain, fatigue, and sleep disturbance, and was labeled by All Symptoms.
Sociodemographic and clinical characteristics of the latent class subgroups
The sociodemographic and clinical characteristics of the latent classes in seven cancer survivors are shown in Table 4 and Supplementary Table S1. Among the sociodemographic factors examined, there were statistically significant differences in marital status, education level, and employment status across the identified latent classes in all seven cancer survivors. Class 1 (WNL) had a higher proportion of being married, survivors with an undergraduate degree or greater, and individuals who are working among identified latent classes than the symptomatic classes (Class 2, Class 3, and Class 3). In prostate, lung, breast, and colorectal cancers, age at diagnosis was associated with latent classes and younger age was associated with symptomatic classes than Class 1. Both race and ethnicity were associated with latent classes in NHL, breast, and colorectal cancers.
Among the clinical factors examined, cancer treatment history was associated with latent classes in breast and colorectal cancers (surgery), chemotherapy (NHL, breast and colorectal cancers), and radiotherapy (prostate and colorectal cancers). Of note, all three cancer treatments (surgery, chemotherapy, and radiotherapy) were associated with latent classes in colorectal cancer.
Discussion
To our knowledge, this study was the first to assess and compare distinct symptom subgroups based on symptoms by seven cancer diagnoses (i.e., prostate, non-small cell lung, NHL, breast, uterine, cervical, and colorectal cancer) in a large sample of cancer survivors using LCPA and a validated symptom measure (PROMIS®), ensuring reliable representations of distressing symptoms common or distinct to different cancers. Analyzing across cancers may unveil shared underlying mechanisms for more targeted interventions to pro-inflammatory status in cancers. Addressing shared inflammatory mechanisms could lead to targeted interventions.
Our study showed variability in the number and types of latent class subgroups based on the specific cancer diagnosis, indicating different symptom experiences among these groups. In prostate, lung, NHL, and breast cancers, four distinct latent classes of patients were identified (WNL, Fatigue/SD/Pain, Fatigue/SD/Depression, and All Symptoms). Fewer distinct symptom patterns were identified in uterine and cervical cancer (three latent classes) and colorectal cancer (two latent classes) compared to the previously mentioned cancer types. These findings have important implications for the management and care of patients across different cancer types. Common latent class subgroups across these seven cancer populations are WNL and All Symptoms groups. The most common four latent classes identified in prostate, lung, NHL, and breast cancers are consistent with previous literature. Our study findings in lung cancer different differ from a previous study on lung cancer survivors [22]. In a study of 378 lung cancer survivors based on pain, fatigue, sleep disturbance, depression, and cognitive impairment, all low and all high-symptom groups were identified [22]. These differences could be due to different sample sizes and instruments compared to our study. Despite fatigue, depression, anxiety, and sleep disturbance are prevalent symptoms in prostate cancer [23] and NHL [24], there is no previous study identified that specifically analyzes latent classes based on symptoms in prostate cancer and NHL. Therefore, our study shed light on the prevalence of these common symptom subgroups (i.e., Fatigue/SD/Pain, Fatigue/SD/Depression, and All Symptoms) in prostate cancer and NHL populations.
We found pain with fatigue and sleep disturbances and depression with fatigue and sleep disturbances were common latent classes across the cancer types, specifically for prostate, lung, NHL, and breast cancers. In 84 cancer patients with multiple cancer diagnoses, pain predicted fatigue and sleep disturbances and sleep disturbances mediated the link of pain with fatigue [24]. Among four common types of latent classes across prostate, lung, NHL, and breast cancers in our study, pain, and depression were associated with fatigue and sleep disturbances. Numerous studies in the literature have indicated a robust correlation between depression, fatigue, and sleep disturbances in cancer survivors [25,26,27]. Cancer-related fatigue is a distressing and persistent symptom frequently experienced by cancer survivors, often resulting from disrupted sleep patterns [26, 27]. The prevalence of fatigue and depression in cancer patients has been extensively researched, with a significant number of survivors reporting elevated depressive symptoms and experiencing fatigue [25]. Additionally, sleep disturbances are common among cancer patients, and studies have shown that these symptoms tend to co-occur, implying a potential shared underlying mechanisms such as proinflammatory cytokines [26]. While causal pathways for whether pain or depression predicts fatigue and sleep disturbances or vice versa are unknown, managing these interconnected symptoms is crucial for enhancing the quality of life and overall well-being of cancer survivors. Our findings showing pain or depression as a distinguishable factor of two latent classes (Fatigue/SD/Pain and Fatigue/SD/Depression) suggest addressing either pain or depression may help to alleviate co-occurring fatigue and sleep disturbances and improve the overall health of cancer survivors.
In uterine cancer survivors, Fatigue/SD/Pain symptom cluster was identified in our study. Pain is one of the most distressing and prevalent symptoms for women with uterine cancer [27]. Furthermore, a 24-month longitudinal study of gynecologic cancer patients found that pain persisted for up to 6-month post-cancer treatments [28]. Of note, women with gynecologic cancers with pain have reported subsequent psychological distress such as depression, anxiety, and fatigue [29]. Inflammation may play a significant role in pain experiences among uterine cancer survivors. Pain sensitization and perpetuation of symptoms are linked to cytokines, which activate both peripheral and central nervous system pathways. These mechanisms involve increased stimulation of the autonomic nervous system, cytokine release by brain glia, and localized and systemic actions of prostaglandins. Proinflammatory cytokines found in the bloodstream have been associated with pain symptoms in various populations, including those with chronic pain disorders and cancer [28]. Therefore, uterine cancer survivors may face an increased risk of inflammation-related pain due to the secretion of pro-inflammatory biomarkers, such as interleukin (IL)-6, by uterine tumors. Furthermore, proinflammatory cytokines are released in response to tissue damage from treatments like chemotherapy, radiation therapy, and surgery. Uterine cancer patients have reported various types of pain such as uterine cramps, pelvic pressure, and abdominal pain [30]. Therefore, types of pain experiences will be further investigated in future studies to better manage pain and pain-related symptom subgroups.
In our study, we found two latent classes (WNL and All Symptoms) in colorectal cancer survivors. Gastrointestinal symptom toxicities such as diarrhea, constipation, abdominal pain, bloating, nausea, and fecal leakage, after cancer treatments are prevalent and severe in colorectal cancer survivors, compared to non-gastrointestinal cancer types [31, 32]. Colorectal cancer survivors with high gastrointestinal symptoms also reported high psychoneurological symptoms [31,32,33]. Thus, further research to identify latent classes including gastrointestinal symptoms is warranted to better capture the complex symptom experiences in colorectal cancer survivors.
In our second aim, we investigated the relationships of sociodemographic and clinical factors with latent classes by cancer diagnosis to understand better the potential contributing factors of distinct latent classes that differ by cancer diagnosis. The research findings confirm that symptom experiences may differ across the various cancer types due to cancer-related specific factors such as cancer sites, cancer stages, as well as different cancer treatment regimens (e.g., surgery, chemotherapy, radiotherapy). Furthermore, our results indicating younger age groups with higher symptom burdens are consistent with previous findings [34]. Younger cancer survivors may experience a higher symptom burden compared to older patients due to their additional life responsibilities and potentially higher resilience levels. Younger individuals often juggle work, family, and caregiving responsibilities, which can exacerbate the impact of cancer-related symptoms [34]. Older patients, on the other hand, may have fewer external stressors and greater acceptance of their health conditions, leading to a perceived lower symptom burden. However, it is essential to consider individual variations in symptom experiences and coping mechanisms across different age groups. Our study findings align with previous research indicating a potentially high symptom burden among cancer survivors with unfavorable social determinants of health (SDOH) status, such as racial/ethnic minorities, low education, low-income status, or poor social support [35]. These factors may contribute to disparities in health outcomes and healthcare access, leading to poorer health literacy and exacerbating symptom experiences [36]. Addressing these disparities is crucial for improving the overall well-being and quality of life of cancer survivors [35].
Implications for clinical practice and further research
Based on our research findings, clinicians should consider that addressing one symptom in isolation given a specific cancer diagnosis may not be sufficient to manage a patient's overall symptom burden. Instead, a holistic approach is needed to comprehensively manage distinct subgroups based on symptoms. Furthermore, approximately 33-58% of cancer survivors in our study experience moderate-to-severe symptom burden, which significantly affects their quality of life. Clinicians should be attentive to these individuals and proactively identify patients with high symptom burdens. Symptom interventions need to be multi-faceted, addressing multiple symptoms simultaneously. For example, lifestyle interventions that incorporate improved sleep hygiene, exercise, and nutrition may positively impact sleep, fatigue, pain, and depression levels, by adopting an integrated approach. The similarities and differences in patterns of symptom subgroups observed in this study raise important theoretical and practical considerations that warrant further investigation. Lastly, understanding sociodemographic and cancer-specific factors can aid in tailoring interventions to meet the diverse needs related to symptom management, in particular, underserved cancer survivors.
Limitations
Our study has several limitations. Our study might have focused on specific seven cancer types or populations (e.g., Whites, female predominant samples), which could limit the generalizability of the findings to other cancer types or patient groups. The heterogeneity of cancer types and treatment regimens might impact symptom experiences differently in various patient populations. Secondly, the use of a cross-sectional design might limit the ability to establish causality and track the changes in symptom subgroups over time. Longitudinal studies would provide a more comprehensive understanding of the dynamic nature of symptom experiences in cancer survivors. Third, we used subjective symptom measures, thus symptom reports might vary based on individual perceptions and reporting biases. Some symptoms may be underreported or overlooked, affecting the accuracy of the identified symptom subgroups. The selected symptom domains for analysis might not capture the full spectrum of symptoms experienced by cancer survivors with various types of cancer diagnoses. Additional symptoms relevant to specific cancer types or treatments might be omitted, potentially influencing the psychoneurological symptoms (e.g., respiratory symptoms in lung cancer, gastrointestinal symptoms in colorectal cancer, and pelvic pain in uterine cancer).
Conclusions
This study explored and compared latent classes based on pain, fatigue, depression, and sleep disturbances among cancer survivors across multiple cancer diagnoses. Our findings add to prior results that numbers and types of symptom subgroups are relatively similar across the four cancer types (prostate, lung, NHL, and breast), and the variation exists in the number of symptom subgroups in uterine, cervical, and colorectal cancers. Cancer-specific factors were significant factors in distinguishing latent classes, while younger age and poor SDOH status were common factors contributing to high symptom burden across seven cancer types. The findings of this study guide future research such as the development of individualized symptom management to target co-occurring symptoms, understanding risk factors of high symptom groups including biosocial mechanisms of co-occurring symptoms, and a longitudinal study examining changes in symptom subgroups over the course of cancer treatments as well as in long-term follow up of cancer survivors.
Data availability
The data that support the findings are openly available in HealthMeasures Dataverse at https://dataverse.harvard.edu/dataverse/HealthMeasures.
References
Miaskowski C, Barsevick A, Berger A et al (2017) Advancing Symptom Science Through Symptom Cluster Research: Expert Panel Proceedings and Recommendations. J Natl Cancer Inst 109(4):djw253. https://doi.org/10.1093/jnci/djw253
Doong SH, Dhruva A, Dunn LB et al (2015) Associations between cytokine genes and a symptom cluster of pain, fatigue, sleep disturbance, and depression in patients prior to breast cancer surgery. Biol Res Nurs 17(3):237–247. https://doi.org/10.1177/1099800414550394
Kim HJ, McGuire DB, Tulman L, Barsevick AM (2005) Symptom clusters: concept analysis and clinical implications for cancer nursing. Cancer Nurs 28(4):270–284. https://doi.org/10.1097/00002820-200507000-00005
Harris CS, Kober KM, Conley YP, Dhruva AA, Hammer MJ, Miaskowski CA (2022) Symptom clusters in patients receiving chemotherapy: A systematic review. BMJ Support Palliat Care 12(1):10–21. https://doi.org/10.1136/bmjspcare-2021-003325
Xiao C (2010) The state of science in the study of cancer symptom clusters. Eur J Oncol Nurs 14(5):417–434. https://doi.org/10.1016/j.ejon.2010.05.011
Li G (2021) A review of the research on symptom clusters in cancer survivors. Open J. Nurs 11:423–434. https://doi.org/10.4236/ojn.2021.116036
Barsevick AM, Whitmer K, Nail LM, Beck SL, Dudley WN (2006) Symptom cluster research: conceptual, design, measurement, and analysis issues. J Pain Symptom Manage 31(1):85–95. https://doi.org/10.1016/j.jpainsymman.2005.05.015
Dong ST, Costa DS, Butow PN et al (2016) Symptom clusters in advanced cancer patients: An empirical comparison of statistical methods and the impact on quality of life. J Pain Symptom Manage 51(1):88–98. https://doi.org/10.1016/j.jpainsymman.2015.07.013
Harris CS, Kober K, Cooper B et al (2022) Symptom clusters in oncology outpatients: stability and consistency across a cycle of chemotherapy. BMJ Support Palliat Care Advance online publication. https://doi.org/10.1136/spcare-2022-003785
de Rooij BH, Oerlemans S, van Deun K et al (2021) Symptom clusters in 1330 survivors of 7 cancer types from the PROFILES registry: A network analysis. Cancer 127(24):4665–4674. https://doi.org/10.1002/cncr.33852
Kim HJ, Abraham I, Malone PS (2013) Analytical methods and issues for symptom cluster research in oncology. Curr Opin Support Palliat Care 7(1):45–53. https://doi.org/10.1097/SPC.0b013e32835bf28b
Vermunt JK, Magidson J (2002) Latent class cluster analysis. In: Hagenaars JA, McCutcheon AL (eds) Applied latent class analysis. Cambridge University Press, Cambridge, pp 89–106
Lee L, Ross A, Griffith K, Jensen RE, Wallen GR (2020) Symptom clusters in breast cancer survivors: A latent class profile analysis. Oncol Nurs Forum 47(1):89–100. https://doi.org/10.1188/20.ONF.89-100
Han CJ, Saligan L, Crouch A et al (2023) Latent class symptom profiles of colorectal cancer survivors with cancer-related cognitive impairment. Support Care Cancer 31(10):559. https://doi.org/10.1007/s00520-023-08031-8
Shin H, Dudley WN, Bhakta N et al (2023) Associations of symptom clusters and health outcomes in adult survivors of childhood cancer: A report from the St Jude lifetime cohort study. J Clin Oncol 41(3):497–507. https://doi.org/10.1200/JCO.22.00361
Jensen RE, Moinpour CM, Keegan THM et al (2016) The Measuring Your Health Study: Leveraging Community-Based Cancer Registry Recruitment to Establish a Large, Diverse Cohort of Cancer Survivors for Analyses of Measurement Equivalence and Validity of the Patient Reported Outcomes Measurement Information System® (PROMIS®) Short Form Items. Psychol Test Assess Model 58:99–117
Cella D, Riley W, Stone A et al (2010) The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol 63(11):1179–1194. https://doi.org/10.1016/j.jclinepi.2010.04.011
Cella D, Choi S, Garcia S et al (2014) Setting standards for severity of common symptoms in oncology using the PROMIS item banks and expert judgment. Qual Life Res 23(10):2651–2661. https://doi.org/10.1007/s11136-014-0732-6
Rothrock NE, Cook KF, O'Connor M, Cella D, Smith AW, Yount SE (2019) Establishing clinically-relevant terms and severity thresholds for Patient-Reported Outcomes Measurement Information System® (PROMIS®) measures of physical function, cognitive function, and sleep disturbance in people with cancer using standard setting. Qual Life Res 28(12):3355–3362. https://doi.org/10.1007/s11136-019-02261-2
Muthén LK, Muthén BO (2021) Mplus Version 8.6. Muthén & Muthén
Corp IBM (2021) IBM SPSS Statistics for Windows, Version 28.0. IBM Corp
Luo J, Liu R, Luo Y et al (2023) The high burden of symptoms associated with cognitive impairment in lung cancer patients: A latent class analysis. Asia Pac J Oncol Nurs 10(4):100200. https://doi.org/10.1016/j.apjon.2023.100200
Baden M, Lu L, Drummond FJ, Gavin A, Sharp L (2020) Pain, fatigue and depression symptom cluster in survivors of prostate cancer. Support Care Cancer 28(10):4813–4824. https://doi.org/10.1007/s00520-019-05268-0
Beck SL, Dudley WN, Barsevick A (2005) Pain, sleep disturbance, and fatigue in patients with cancer: Using a mediation model to test a symptom cluster. Oncol Nurs Forum 32(3):542. https://doi.org/10.1188/04.ONF.E48-E55
He X, Ng M, Choi K et al (2022) Synergistic interactions among fatigue, sleep disturbance, and depression in women with breast cancer: A cross-sectional study. Oncol Nurs Forum 49(3):243–254. https://doi.org/10.1188/22.ONF.243-254
Santoso AMM, Jansen F, Peeters CFW et al (2022) Psychoneurological symptoms and biomarkers of stress and inflammation in newly diagnosed head and neck cancer patients: A network analysis. Curr Oncol 29(10):7109–7121. https://doi.org/10.3390/curroncol29100559
Hacker KE, Reynolds RK, Uppal S (2018) Ongoing strategies and updates on pain management in gynecologic oncology patients. Gynecol Oncol 149(2):410–419. https://doi.org/10.1016/j.ygyno.2018.01.034
Honerlaw KR, Rumble ME, Rose SL, Coe CL, Costanzo ES (2016) Biopsychosocial predictors of pain among women recovering from surgery for endometrial cancer. Gynecol Oncol 140(2):301–306. https://doi.org/10.1016/j.ygyno.2015.09.005
Linden W, Vodermaier A, Mackenzie R, Greig D (2012) Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord 141(2-3):343–351. https://doi.org/10.1016/j.jad.2012.03.025
Boeckstaens S, Dewalheyns S, Heremans R et al (2020) Signs and symptoms associated with uterine cancer in pre- and postmenopausal women. Heliyon 6(11):e05372. https://doi.org/10.1016/j.heliyon.2020.e05372
Han CJ, Reding K, Cooper BA et al (2019) Stability of symptom clusters in patients with gastrointestinal cancers receiving chemotherapy. J Pain Symptom Manage 58(6):989–1001.e10. https://doi.org/10.1016/j.jpainsymman.2019.07.029
Han CJ, Reding KW, Kalady MF, Yung R, Greenlee H, Paskett ED (2023) Factors associated with long-term gastrointestinal symptoms in colorectal cancer survivors in the women's health initiatives (WHI study). PLoS One 18(5):e0286058. https://doi.org/10.1371/journal.pone.0286058
Han CJ, Yang GS, Syrjala K (2020) Symptom experiences in colorectal cancer survivors after cancer treatments: A systematic review and meta-analysis. Cancer Nurs 43(3):E132–E158. https://doi.org/10.1097/NCC.0000000000000785
Johannessen MS, Miaskowski C, Kleven AG et al (2023) Age-related differences in the occurrence, severity, and distress of symptoms in older patients at the initiation of chemotherapy. BMC Geriatr 23(1):481. https://doi.org/10.1186/s12877-023-04198-1
Badger TA, Segrin C, Crane TE et al (2023) Social determinants of health and symptom burden during cancer treatment. Nurs Res 72(2):103–113. https://doi.org/10.1097/NNR.0000000000000636
Coughlin SS (2021) Social determinants of health and cancer survivorship. J Environ Health Sci 7(1):11–15
Funding
Open access funding provided by the National Institutes of Health. This research was supported by the Intramural Research Program at the National Institutes of Health, Clinical Center.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Lena J. Lee (first author) and reviewed by all authors. Lena J. Lee conducted primary data analyses. The first draft of the manuscript was written by Lena J. Lee and Claire J. Han, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was a secondary analysis of data obtained from the Measuring Your Health (MY-Health) Study. The Office of Human Subjects Research Protections at the National Institutes of Health Clinical Center determined that the research was not human subject research.
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 53 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, L.J., Han, C.J., Saligan, L. et al. Comparing symptom clusters in cancer survivors by cancer diagnosis: A latent class profile analysis. Support Care Cancer 32, 308 (2024). https://doi.org/10.1007/s00520-024-08489-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08489-0