Abstract
Purpose
To evaluate the effect of telehealth interventions on adherence to endocrine therapy among patients with breast cancer.
Methods
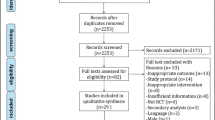
A systematic search of five English databases (PubMed, Web of Science, Embase, the American Psychological Association PsycNet, and the Cochrane Library) and four Chinese databases (Chinese National Knowledge Infrastructure, SinoMed, WanFang Data, and WeiPu Data) was performed from inception to March 31, 2023. Two investigators independently screened the available studies for eligibility and extracted relevant data. Quality assessment was conducted using the Cochrane Risk of Bias Tool. The effect size was computed based on the risk ratio for dichotomous data and standardized mean difference for continuous data using Review Manager 5.4.
Results
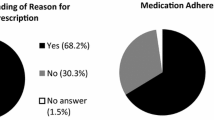
A total of 1,780 participants from eight randomized controlled trials were included. These studies involved treatment with aromatase inhibitors only (n = 3) or aromatase inhibitors plus tamoxifen (n = 5). Telehealth interventions involved web-based interventions, telephone-based interventions, interventions via mobile applications, and interventions based on technology. In three studies, subjective measures were used, while objective measures were utilized in another three. Two studies incorporated a combination of both subjective and objective measures. The duration of the interventions varied among studies, ranging from a week to 36 months. The follow-up duration ranged from 4 weeks to 36 months. The quality of included studies was moderate to high. The meta-analysis of the five studies reporting dichotomous data showed that telehealth interventions had a significant effect on adherence to endocrine therapy (RR = 0.86, 95% CI = 0.76–0.97). Moreover, four studies reported continuous data. The meta-analysis demonstrated that telehealth interventions significantly improved adherence to endocrine therapy at 1 month (SMD = 0.50, 95% CI = 0.10–0.90), 3 months (SMD = 0.58, 95% CI = 0.17–0.99), and 6 months (SMD = 0.27, 95% CI = 0.08–0.47) of follow-up.
Conclusion
Telehealth interventions may facilitate adherence to endocrine therapy among patients with breast cancer. Further research should adopt a theory-based design and explore the longer-term effects.






Similar content being viewed by others
Data availability
The data that supported the analysis in this review were all extracted from the original studies. All data relevant to the study are included in the article.
Code availability
Not applicable.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Waks AG, Winer EP (2019) Breast cancer treatment: a review. Jama 321:288–300. https://doi.org/10.1001/jama.2018.19323
Burstein HJ, Lacchetti C, Anderson H et al (2019) Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol 37:423–438. https://doi.org/10.1200/jco.18.01160
Davies C, Godwin J, Gray R et al (2011) Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet 378:771–784. https://doi.org/10.1016/s0140-6736(11)60993-8
Ibrar M, Peddie N, Agnew S et al (2022) Breast cancer survivors’ lived experience of adjuvant hormone therapy: a thematic analysis of medication side effects and their impact on adherence. Front Psychol 13:861198. https://doi.org/10.3389/fpsyg.2022.861198
Yussof I, Mohd Tahir NA, Hatah E, Mohamed Shah N (2022) Factors influencing five-year adherence to adjuvant endocrine therapy in breast cancer patients: a systematic review. Breast 62:22–35. https://doi.org/10.1016/j.breast.2022.01.012
De Geest S, Sabaté E (2003) Adherence to long-term therapies: evidence for action. Eur J Cardiovasc Nurs 2:323. https://doi.org/10.1016/s1474-5151(03)00091-4
Franzoi MA, Agostinetto E, Perachino M et al (2021) Evidence-based approaches for the management of side-effects of adjuvant endocrine therapy in patients with breast cancer. Lancet Oncol 22:e303–e313. https://doi.org/10.1016/s1470-2045(20)30666-5
Villarreal-Garza C, Mesa-Chavez F, Ferrigno AS et al (2021) Adjuvant endocrine therapy for premenopausal women with breast cancer: patient adherence and physician prescribing practices in Mexico. Breast 59:8–15. https://doi.org/10.1016/j.breast.2021.05.013
McCowan C, Wang S, Thompson AM et al (2013) The value of high adherence to tamoxifen in women with breast cancer: a community-based cohort study. Br J Cancer 109:1172–1180. https://doi.org/10.1038/bjc.2013.464
Bright EE, Finkelstein LB, Nealis MS et al (2023) A systematic review and meta-analysis of interventions to promote adjuvant endocrine therapy adherence among breast cancer survivors. J Clin Oncol 41:4548–4561. https://doi.org/10.1200/JCO.23.00697
Conn VS, Ruppar TM (2017) Medication adherence outcomes of 771 intervention trials: systematic review and meta-analysis. Prev Med 99:269–276. https://doi.org/10.1016/j.ypmed.2017.03.008
Wang J, Wang Y, Wei C et al (2014) Smartphone interventions for long-term health management of chronic diseases: an integrative review. Telemed J E Health 20:570–583. https://doi.org/10.1089/tmj.2013.0243
Dario AB, Moreti Cabral A, Almeida L et al (2017) Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J 17:1342–1351. https://doi.org/10.1016/j.spinee.2017.04.008
Li J, Liu Y, Jiang J et al (2021) Effect of telehealth interventions on quality of life in cancer survivors: a systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud 122:103970. https://doi.org/10.1016/j.ijnurstu.2021.103970
Larson JL, Rosen AB, Wilson FA (2018) The effect of telehealth interventions on quality of life of cancer patients: a systematic review and meta-analysis. Telemed J E Health 24:397–405. https://doi.org/10.1089/tmj.2017.0112
Al-Arkee S, Mason J, Lane DA et al (2021) Mobile apps to improve medication adherence in cardiovascular disease: systematic review and meta-analysis. J Med Internet Res 23:e24190. https://doi.org/10.2196/24190
Basit SA, Mathews N, Kunik ME (2020) Telemedicine interventions for medication adherence in mental illness: a systematic review. Gen Hosp Psychiatry 62:28–36. https://doi.org/10.1016/j.genhosppsych.2019.11.004
Park HR, Kang HS, Kim SH, Singh-Carlson S (2022) Effect of a smart pill bottle reminder intervention on medication adherence, self-efficacy, and depression in breast cancer survivors. Cancer Nurs 45:E874-e882. https://doi.org/10.1097/ncc.0000000000001030
Yu KD, Zhou Y, Liu GY et al (2012) A prospective, multicenter, controlled, observational study to evaluate the efficacy of a patient support program in improving patients’ persistence to adjuvant aromatase inhibitor medication for postmenopausal, early stage breast cancer. Breast Cancer Res Treat 134:307–313. https://doi.org/10.1007/s10549-012-2059-8
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Higgins JP, Altman DG, Gøtzsche PC et al (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Higgins JP, Thomas J, Chandler J et al (2019) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons
Rice ME, Harris GT (2005) Comparing effect sizes in follow-up studies: ROC area, cohen’s d, and r. Law Hum Behav 29:615–620. https://doi.org/10.1007/s10979-005-6832-7
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Bmj 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Jacobs JM, Post K, Massad K et al (2022) A telehealth intervention for symptom management, distress, and adherence to adjuvant endocrine therapy: a randomized controlled trial. Cancer 128:3541–3551. https://doi.org/10.1002/cncr.34409
Hershman DL, Unger JM, Hillyer GC et al (2020) Randomized trial of text messaging to reduce early discontinuation of adjuvant aromatase inhibitor therapy in women with early-stage breast cancer: SWOG S1105. J Clin Oncol 38:2122–2129. https://doi.org/10.1200/jco.19.02699
Tan EH, Wong ALA, Tan CC et al (2020) Improving medication adherence with adjuvant aromatase inhibitor in women with breast cancer: a randomised controlled trial to evaluate the effect of short message service (SMS) reminder. Breast 53:77–84. https://doi.org/10.1016/j.breast.2020.06.012
Ziller V, Kyvernitakis I, Knöll D et al (2013) Influence of a patient information program on adherence and persistence with an aromatase inhibitor in breast cancer treatment–the COMPAS study. BMC Cancer 13:407. https://doi.org/10.1186/1471-2407-13-407
Zhu Y, Hu Y, Wu M et al (2015) Effect of nurse-led follow-up on medication adherence and quality of life of patients with breast cancer. Chin J Nurs 50:69–73
Wang C, Hu Y, Wu M et al (2017) The effectiveness of computer-based monitoring system for patients with breast cancer receiving adjuvant hormonal therapy. Chin J Nurs 52:261–266
Xu H (2020) Intervention study to improve disease knowledge and health behavior of breast cancer patients with endocrine therapy based on cross-theoretical models. Dissertation, China Medical University
Koç Z, Kaplan E, Tanrıverdi D (2022) The effectiveness of telehealth programs on the mental health of women with breast cancer: a systematic review. J Telemed Telecare 1357633x211069663. https://doi.org/10.1177/1357633x211069663
Singleton AC, Raeside R, Hyun KK et al (2022) Electronic health interventions for patients with breast cancer: systematic review and meta-analyses. J Clin Oncol 40:2257–2270. https://doi.org/10.1200/jco.21.01171
DeKoekkoek T, Given B, Given CW et al (2015) mHealth SMS text messaging interventions and to promote medication adherence: an integrative review. J Clin Nurs 24:2722–2735. https://doi.org/10.1111/jocn.12918
Skrabal Ross X, Gunn KM, Patterson P, Olver I (2018) Mobile-based Oral chemotherapy adherence-enhancing interventions: scoping review. JMIR Mhealth Uhealth 6:e11724. https://doi.org/10.2196/11724
Tan EH, Wong ALA, Tan CC et al (2021) Facilitators and barriers to medication adherence with adjuvant endocrine therapy in women with breast cancer: a structural equation modelling approach. Breast Cancer Res Treat 188:779–788. https://doi.org/10.1007/s10549-021-06204-9
Paranjpe R, John G, Trivedi M, Abughosh S (2019) Identifying adherence barriers to oral endocrine therapy among breast cancer survivors. Breast Cancer Res Treat 174:297–305. https://doi.org/10.1007/s10549-018-05073-z
Riley WT, Rivera DE, Atienza AA et al (2011) Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med 1:53–71. https://doi.org/10.1007/s13142-011-0021-7
Yang H, Zhang H, Lu Y et al (2022) A program to improve the knowledge, attitudes, and practices of needle stick and sharps injuries through bundled interventions among nurses: an KAP mode-based approach to intervention. Psychol Health Med 27:999–1010. https://doi.org/10.1080/13548506.2020.1830132
Stirratt MJ, Dunbar-Jacob J, Crane HM et al (2015) Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med 5:470–482. https://doi.org/10.1007/s13142-015-0315-2
Acknowledgements
The authors would like to be thankful to the National Natural Science Foundation of China for the fund support.
Funding
This study was supported by the National Natural Science Foundation of China (Grant number: 71974218).
Author information
Authors and Affiliations
Contributions
Conceptualization: MFZ.
Acquisition of data: SHS and BYZ.
Analysis and/or interpretation of data: SHS and MYZ.
Drafting the manuscript: SHS and BYZ.
Revising the manuscript critically for important intellectual content: MYZ, NZ and YHZ.
Data validation: SHS, NZ, YHZ and MYZ.
Supervision: MFZ.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shihao Sun and Baoyi Zhang are joint first authors and contributed equally to this paper.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, S., Zhang, B., Zhang, N. et al. Effect of telehealth interventions on adherence to endocrine therapy among patients with breast cancer: a systematic review and meta-analysis. Support Care Cancer 32, 151 (2024). https://doi.org/10.1007/s00520-024-08339-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08339-z